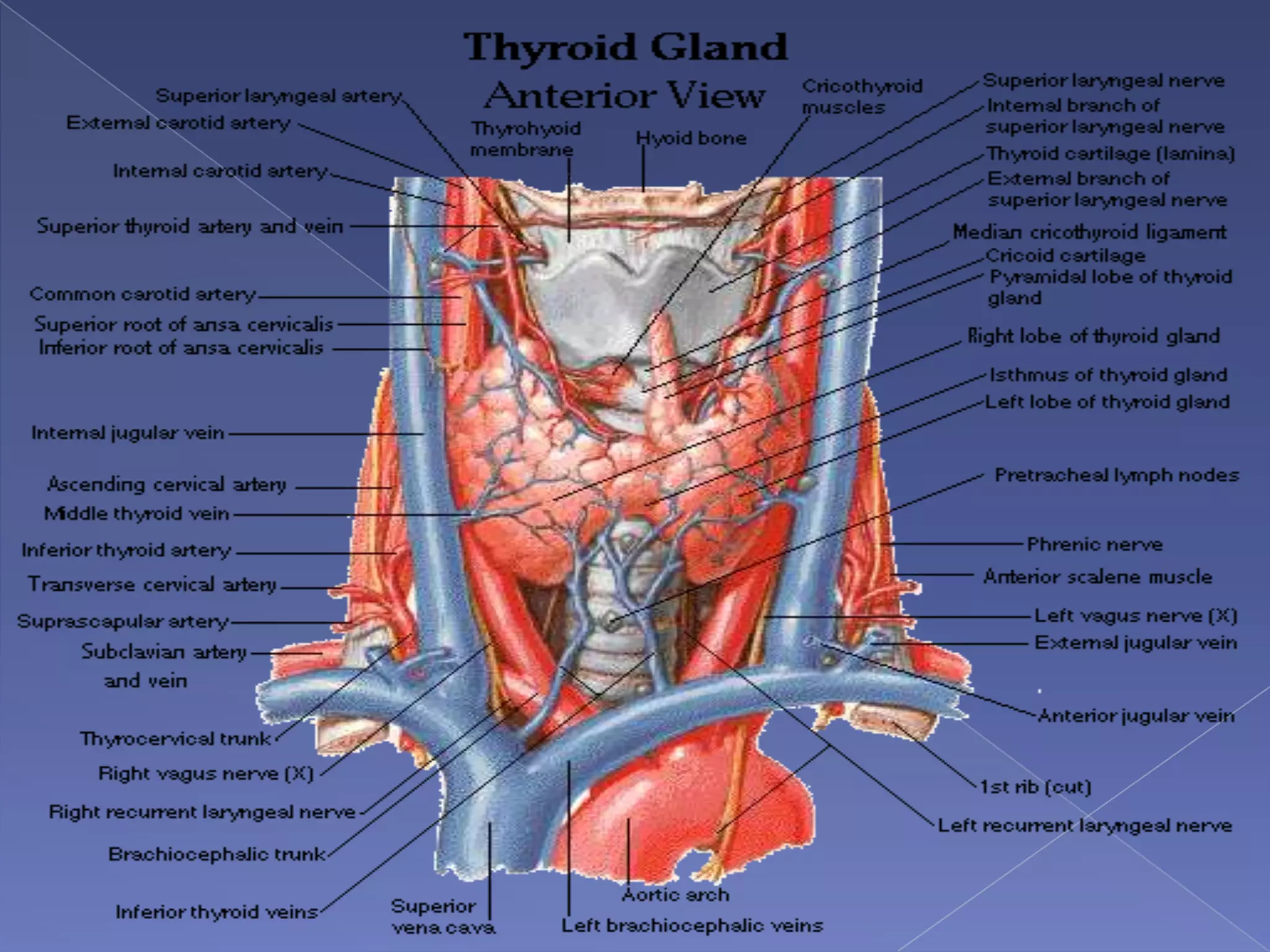
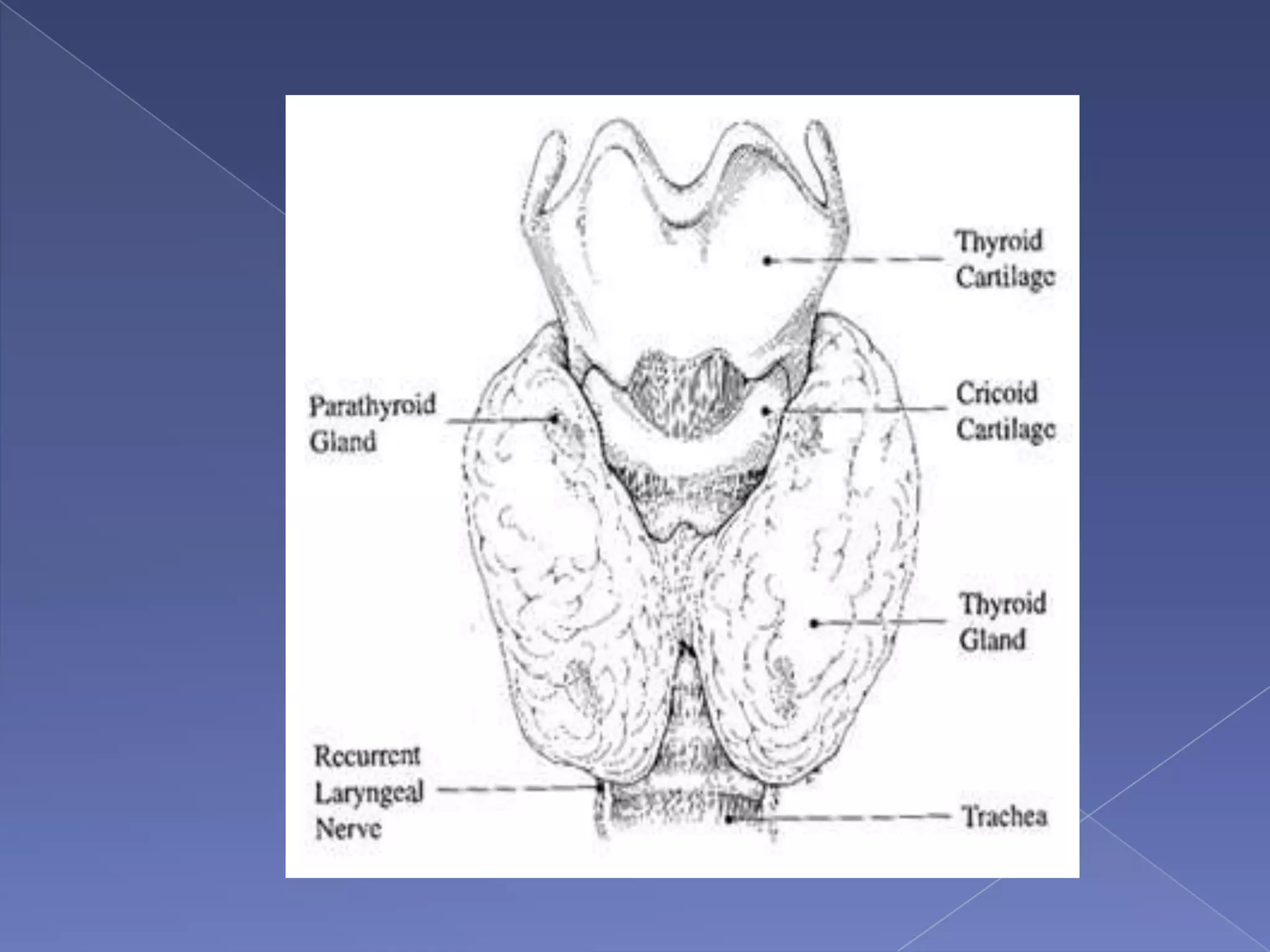
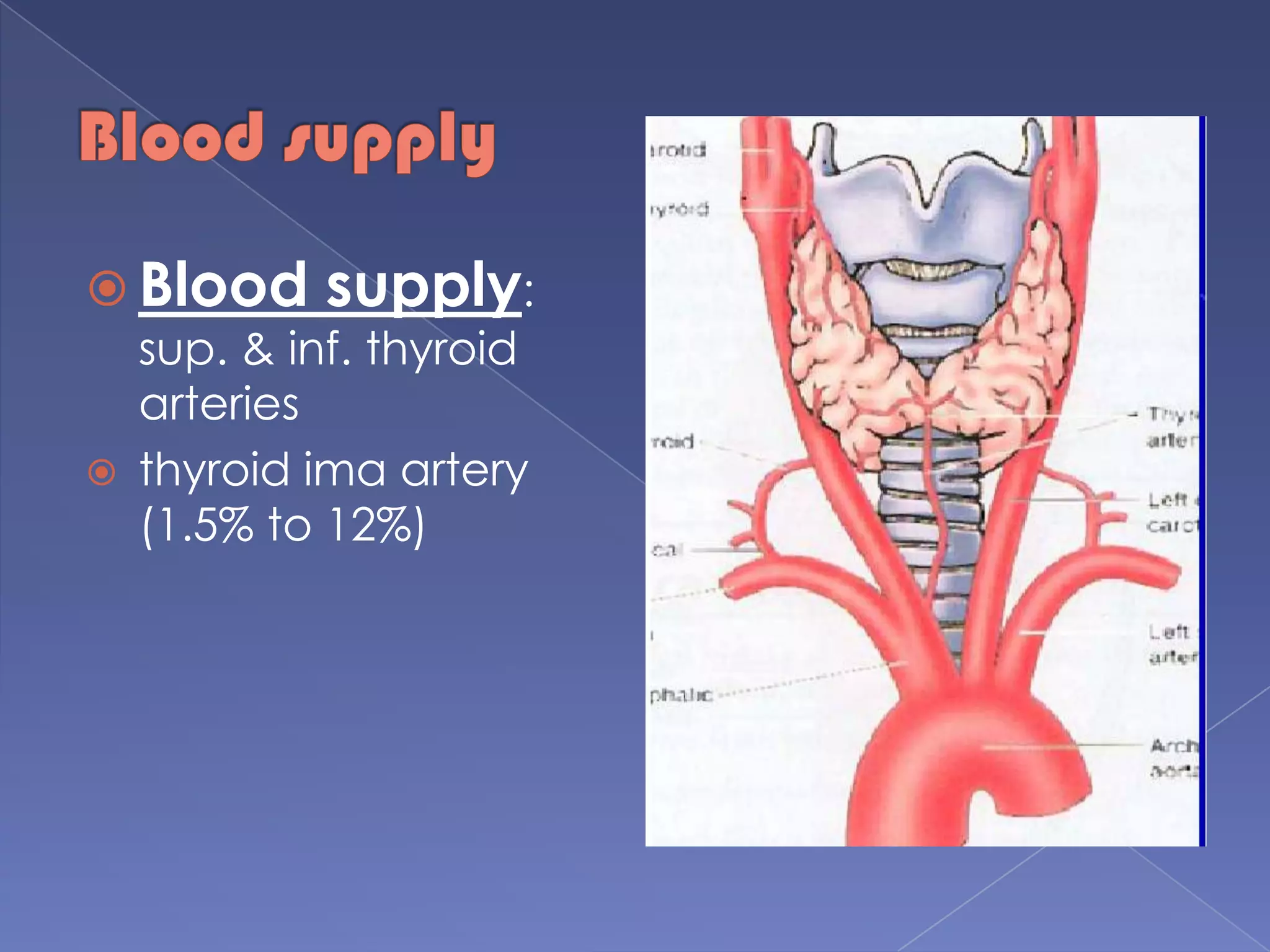
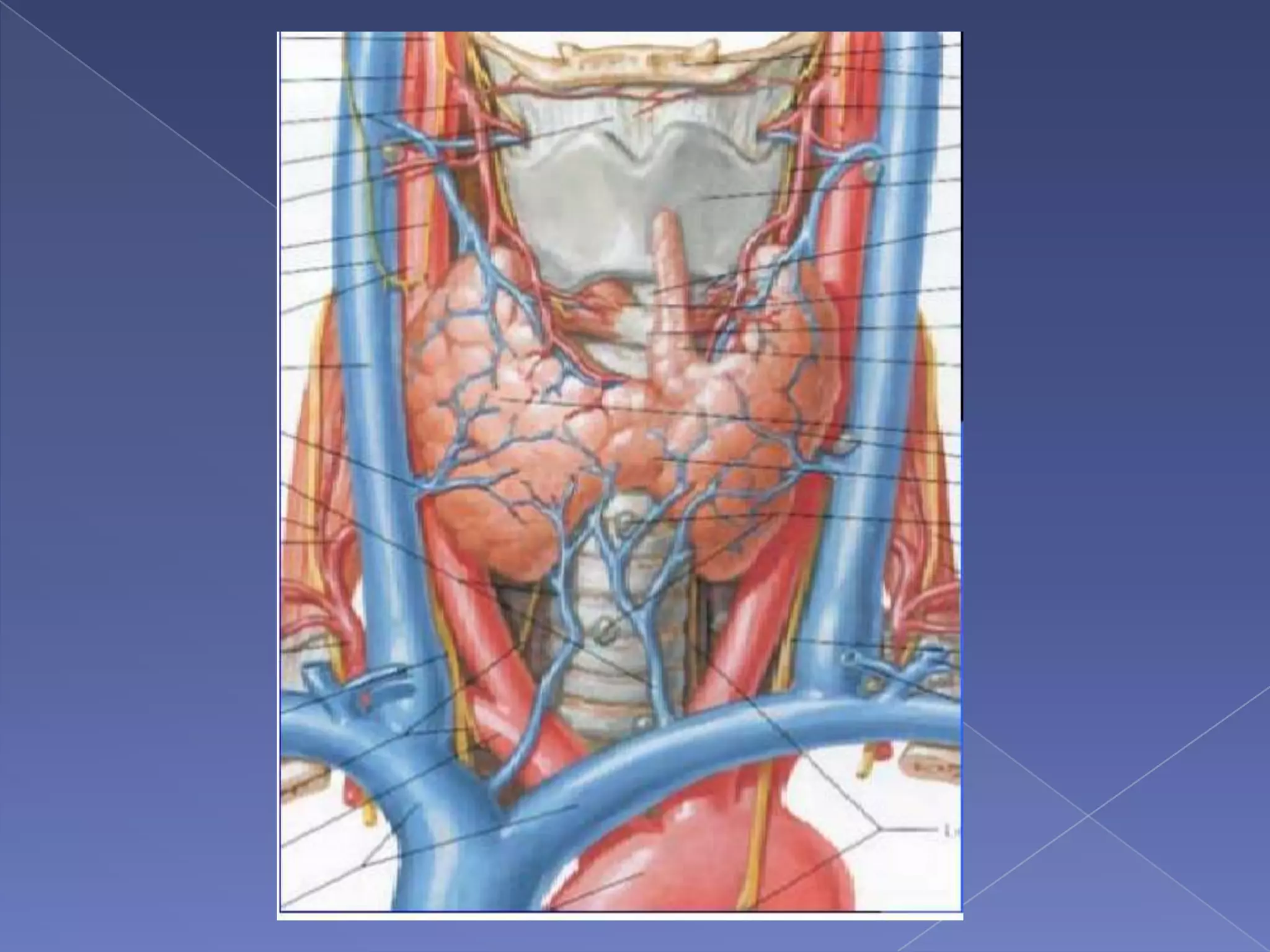
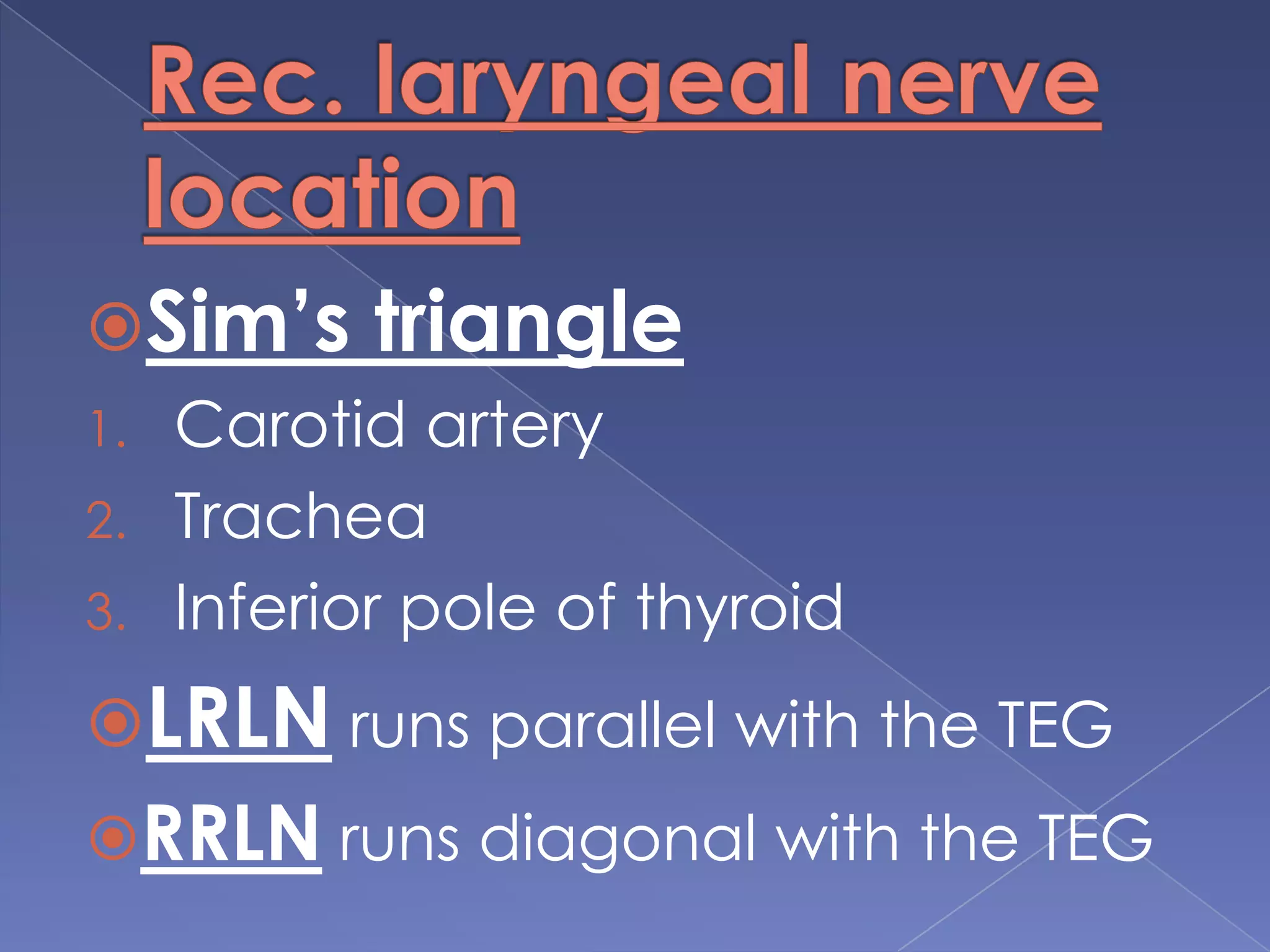
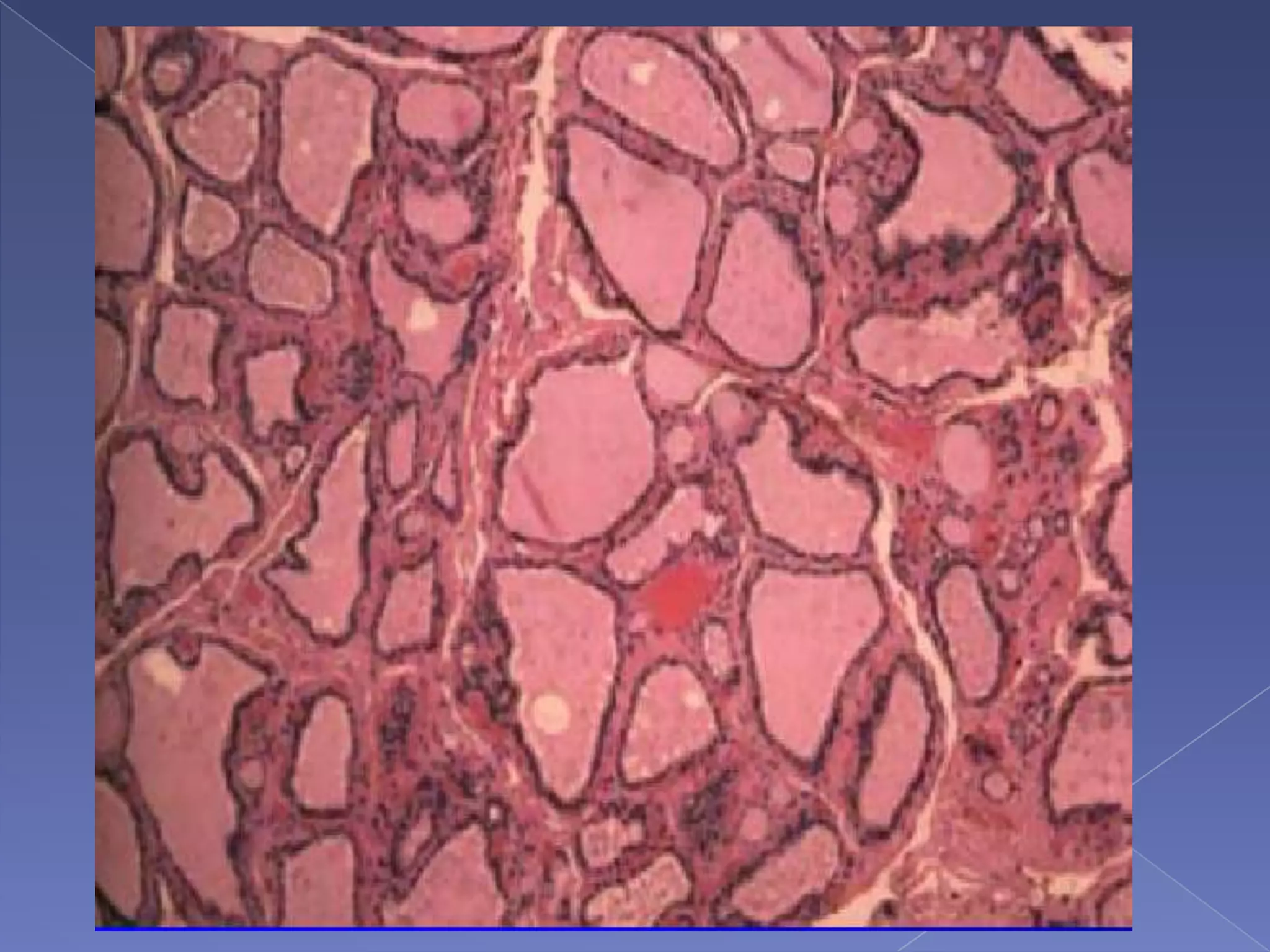
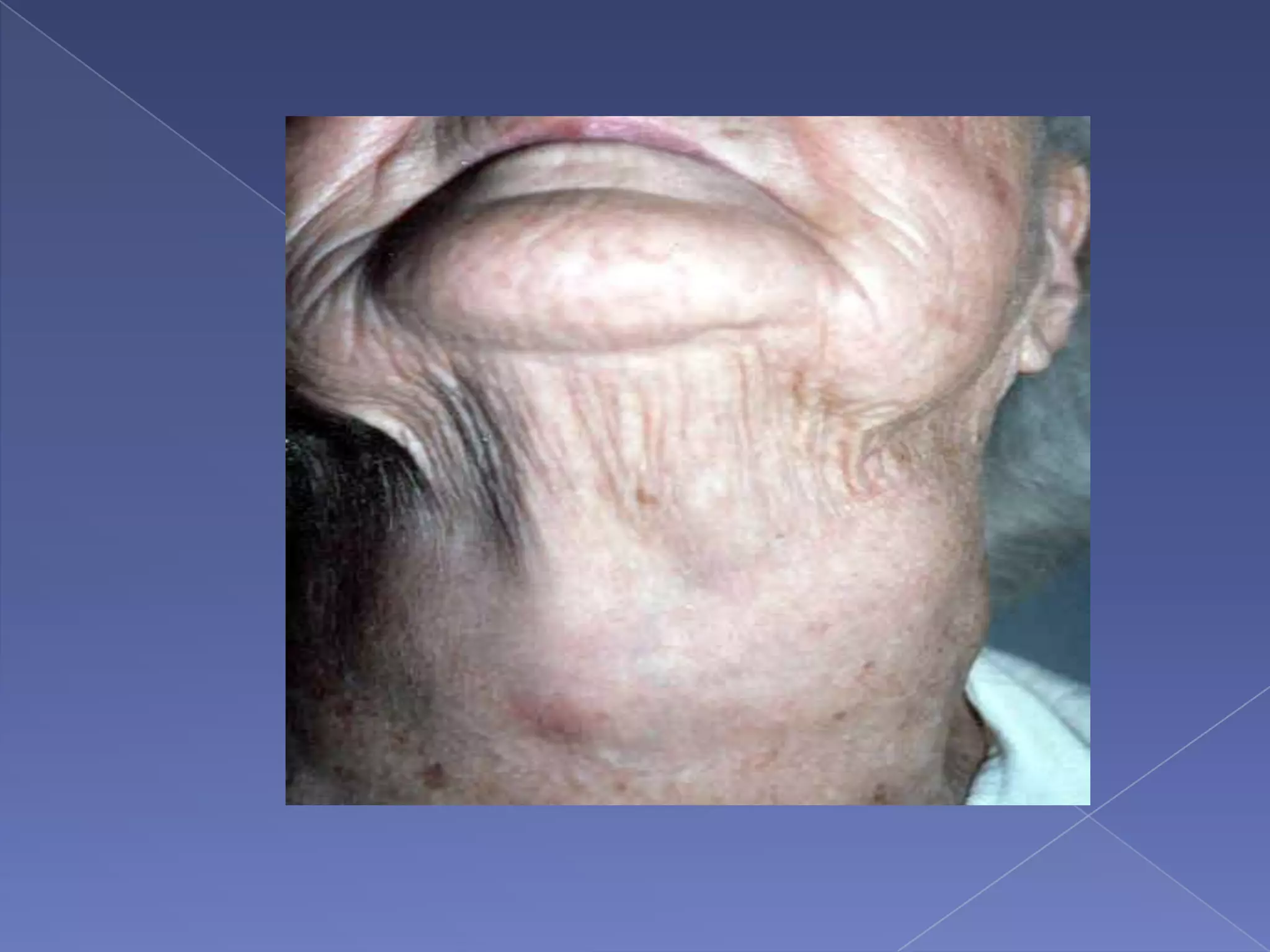
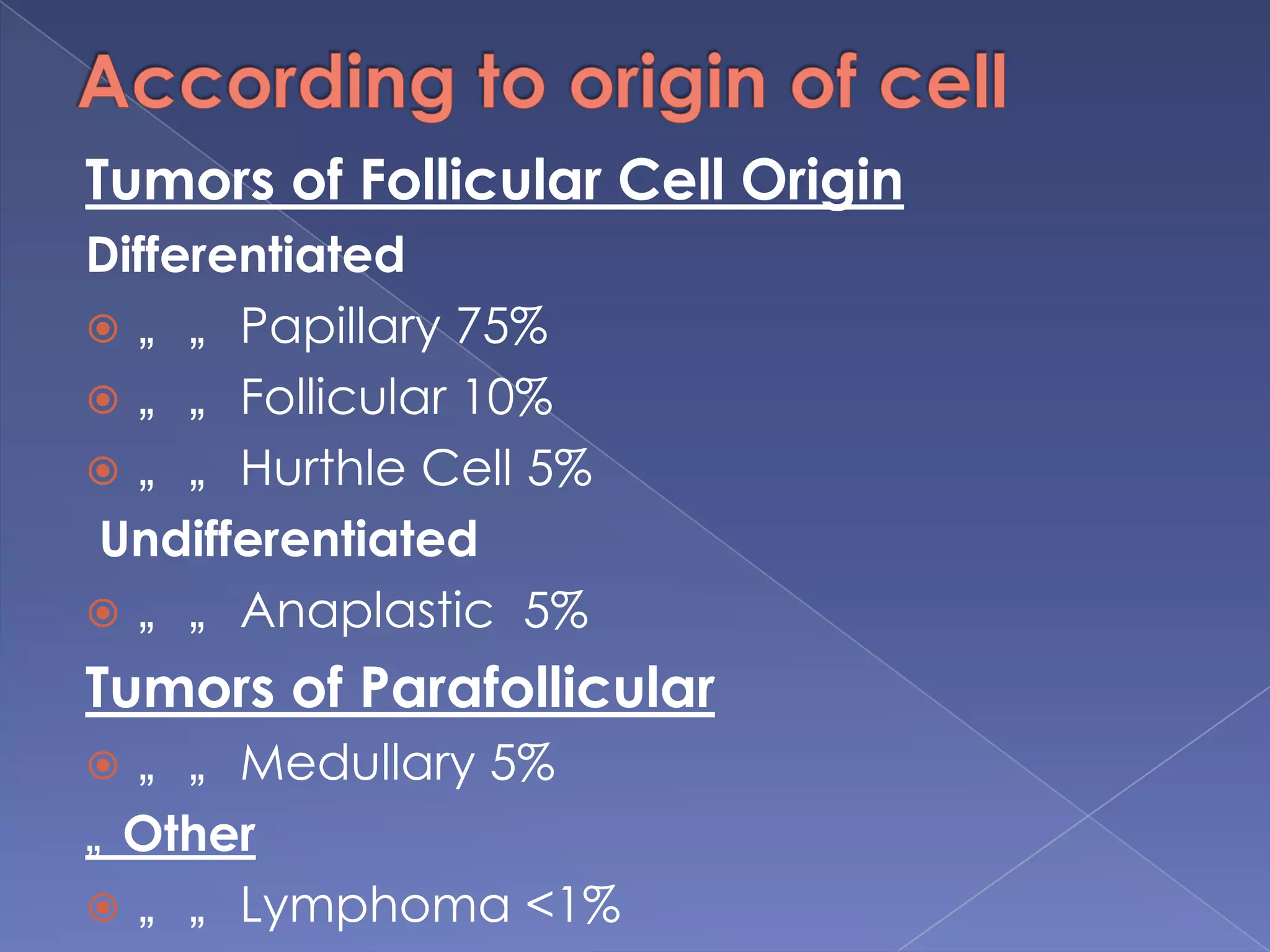
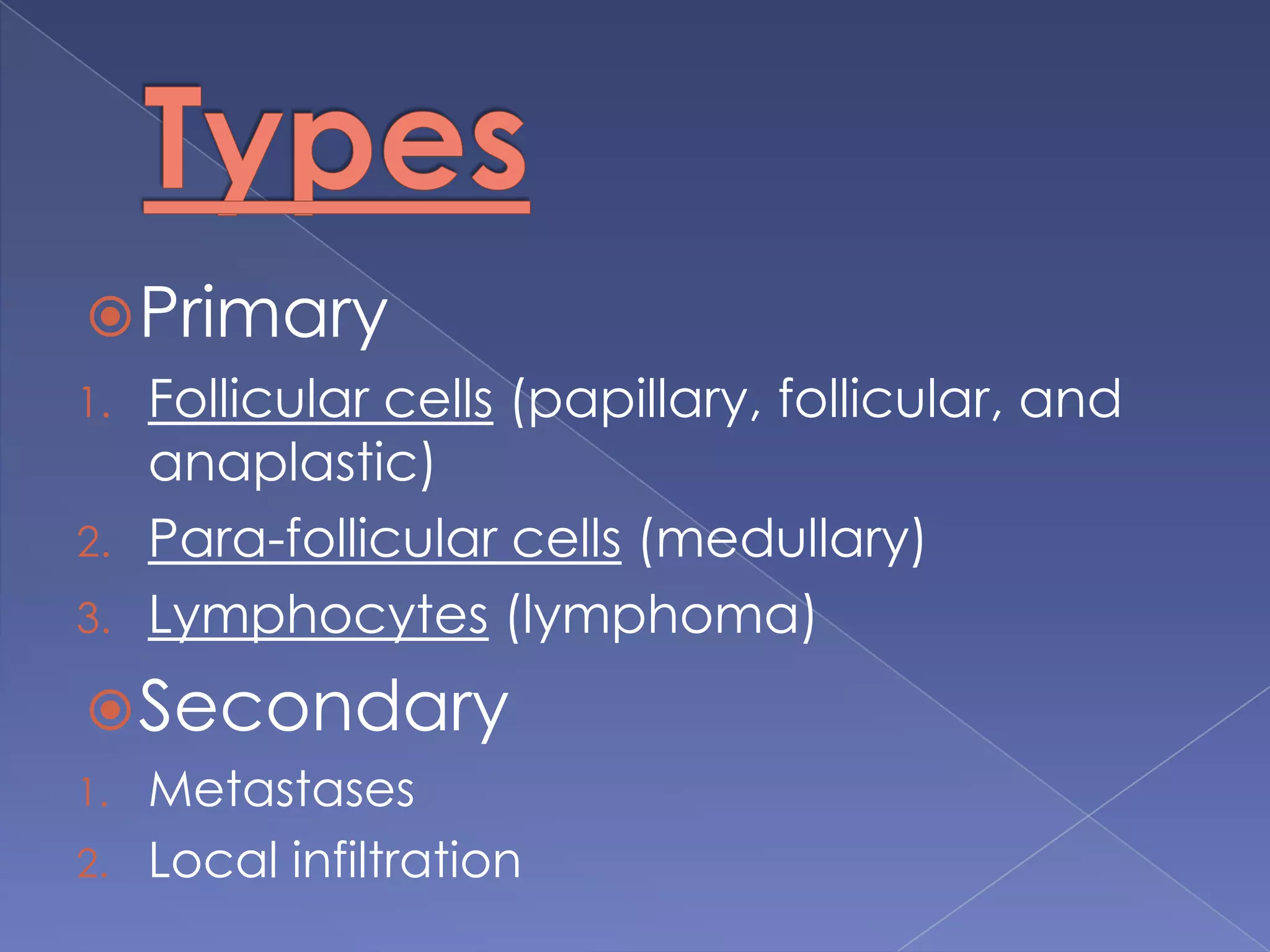
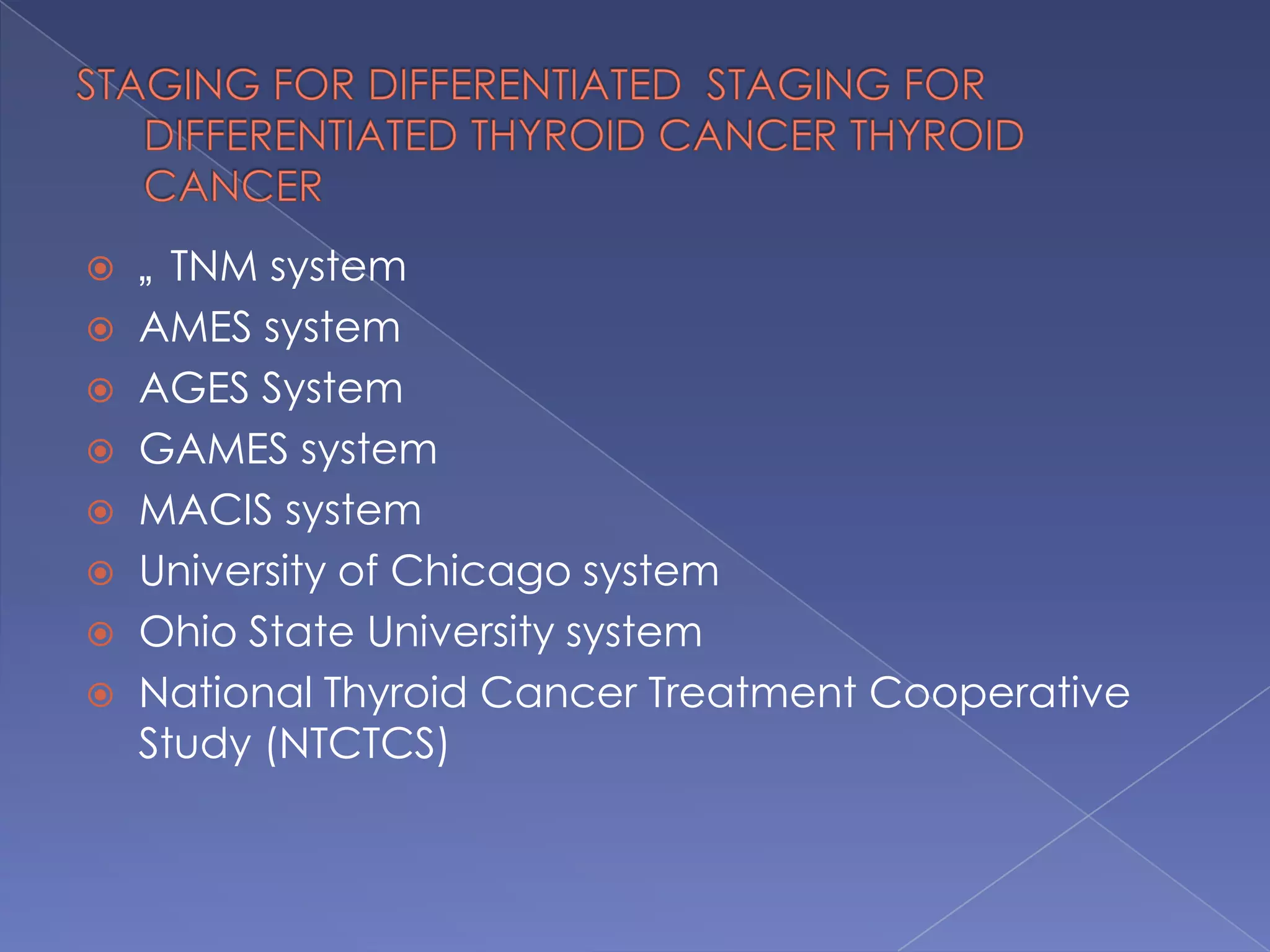
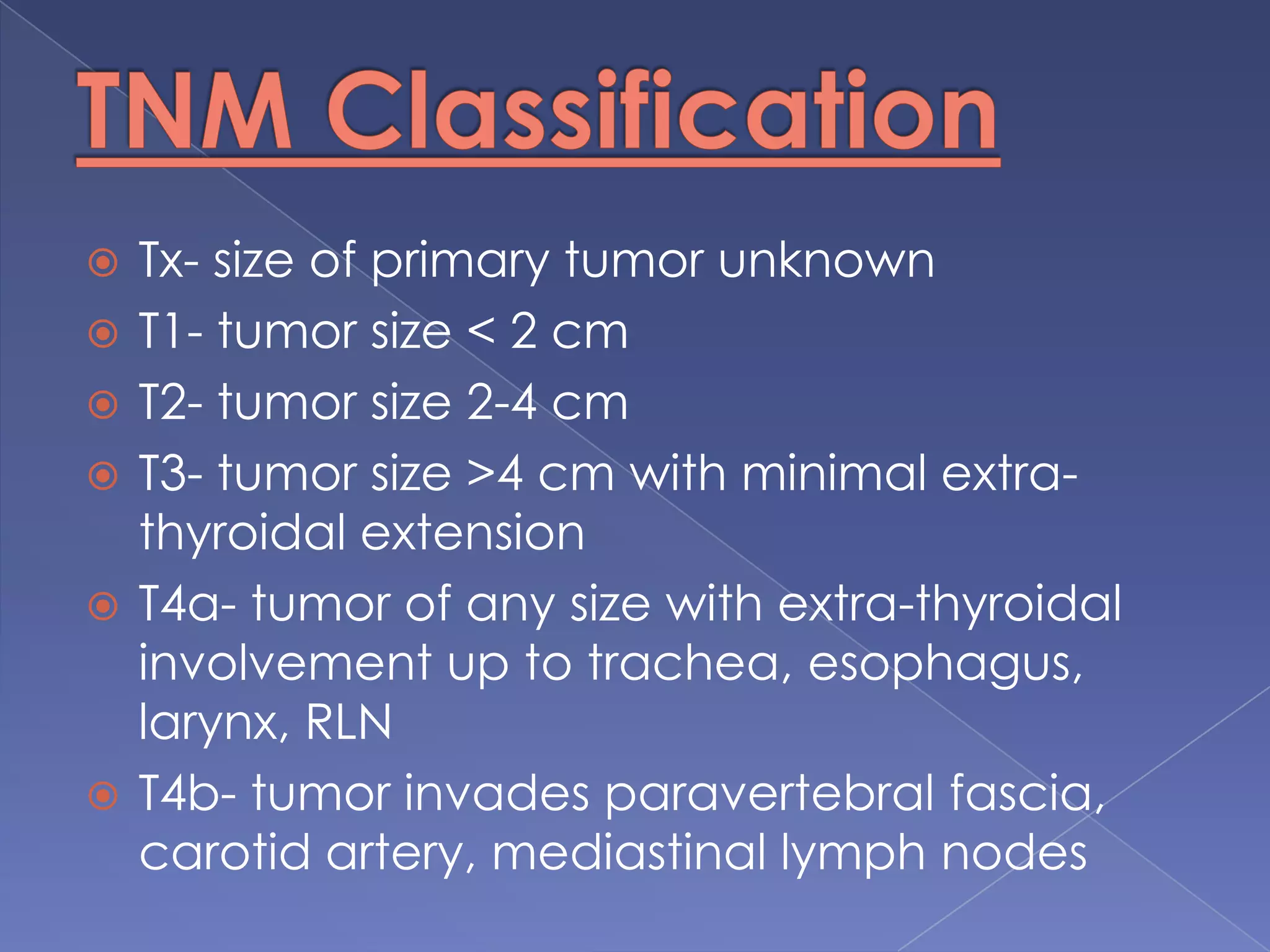
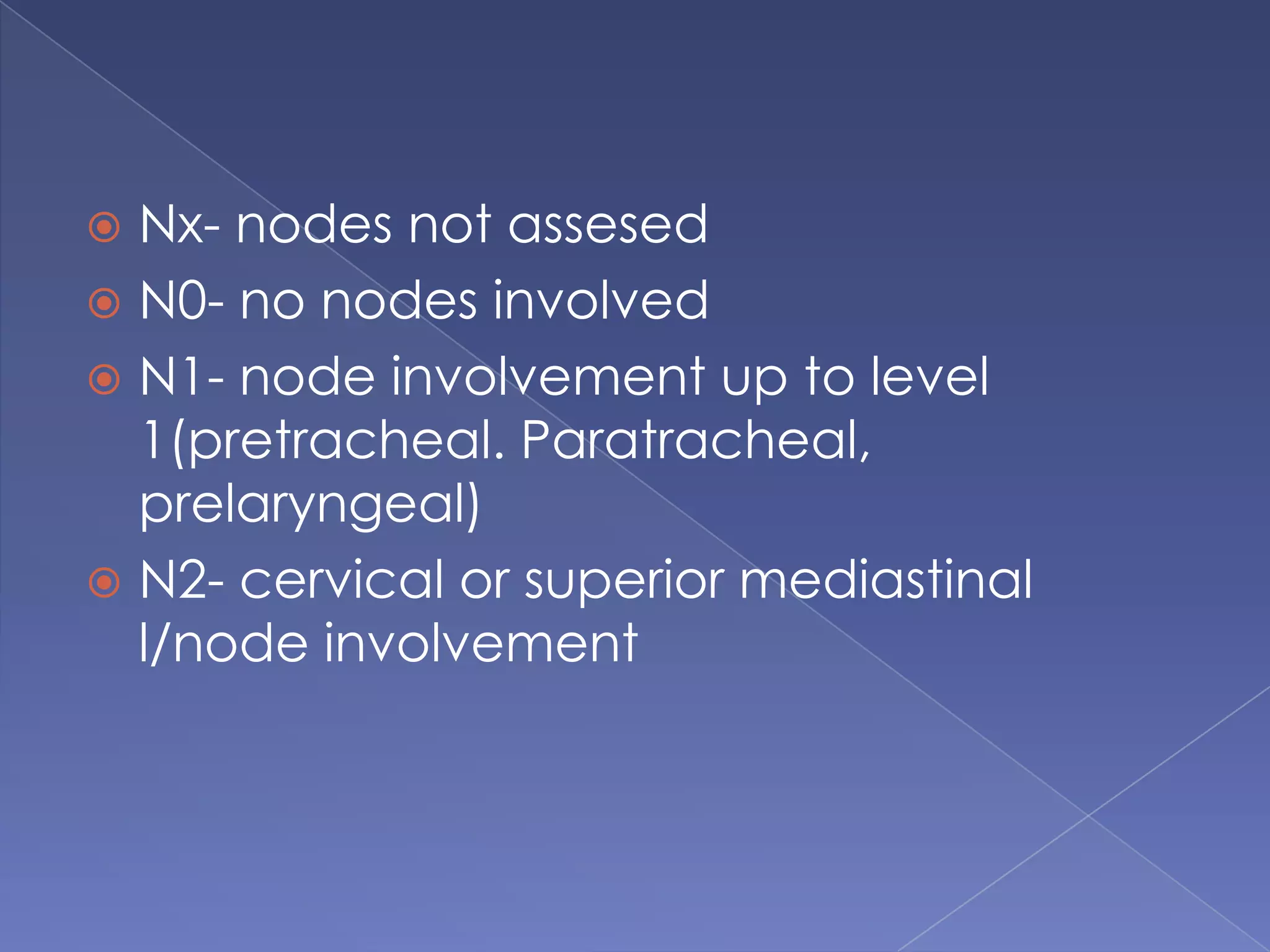
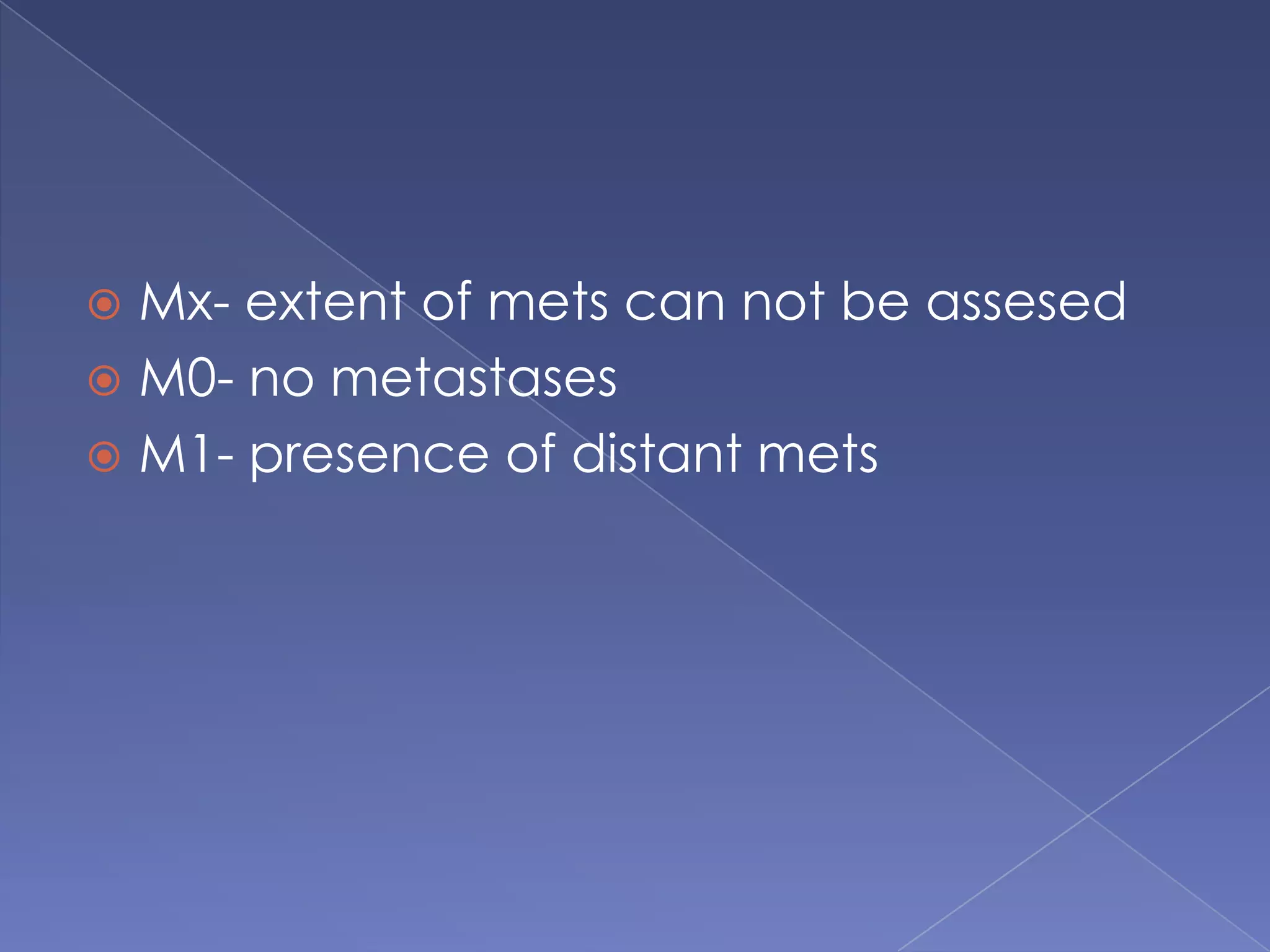
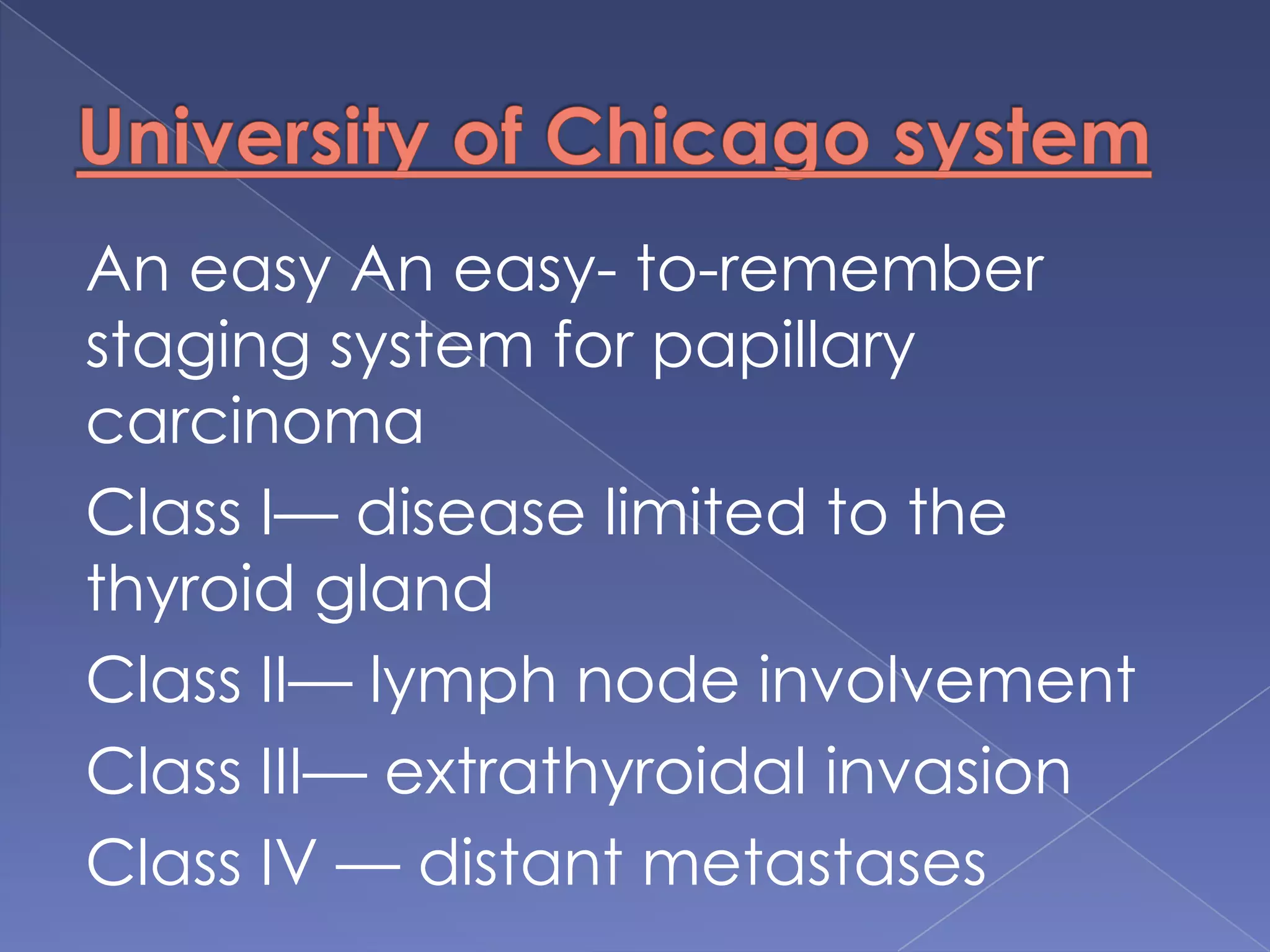
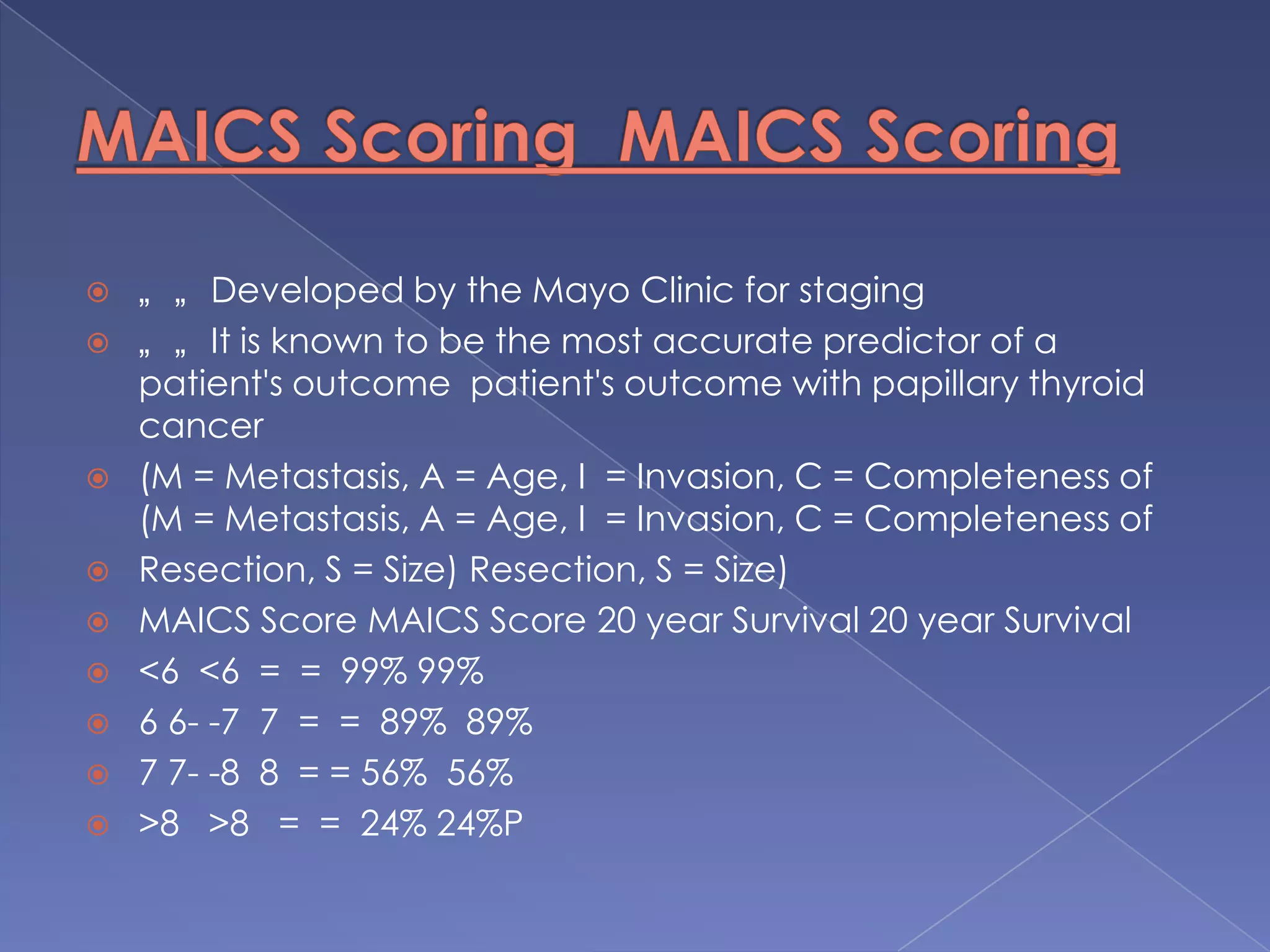
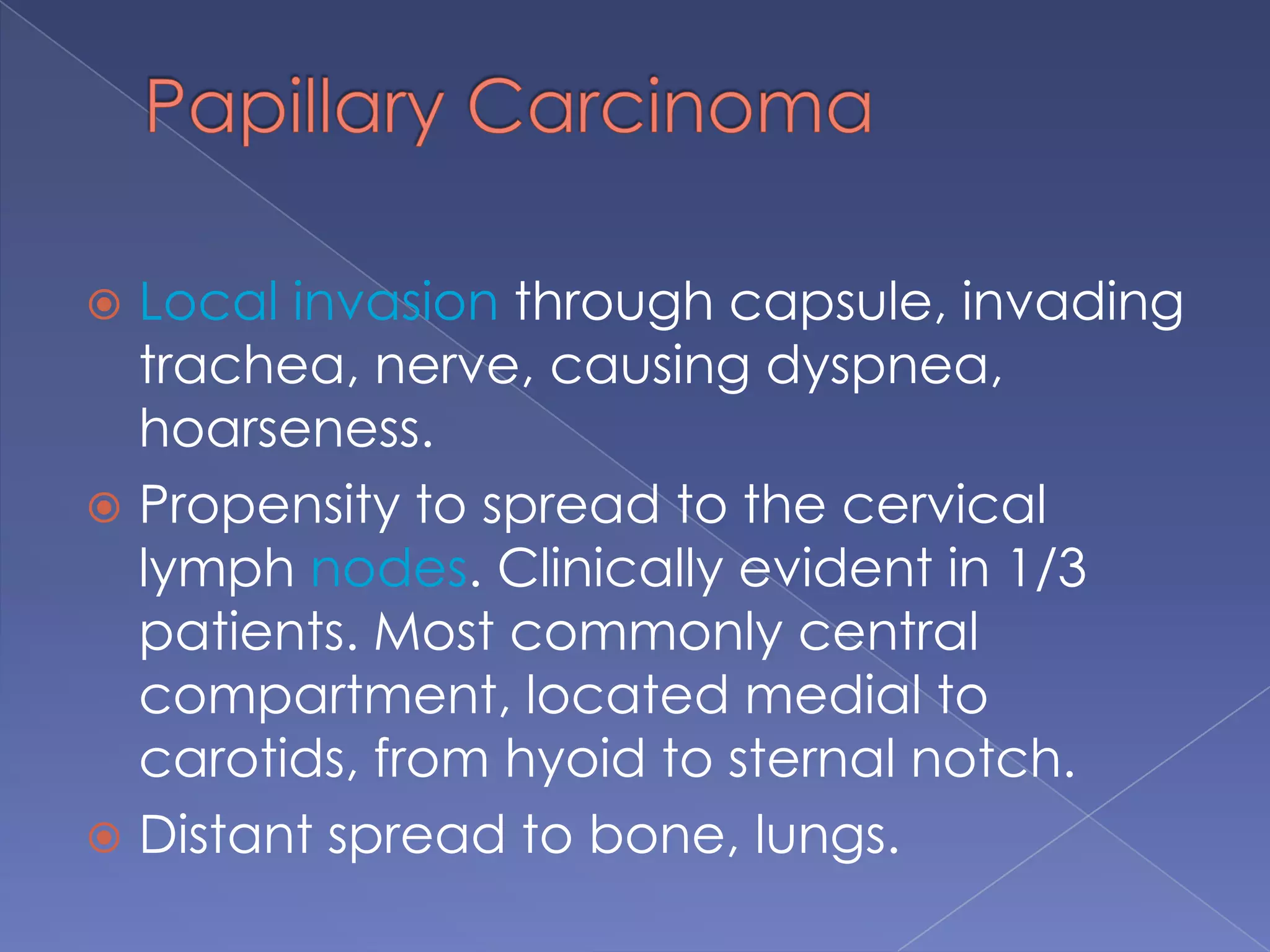
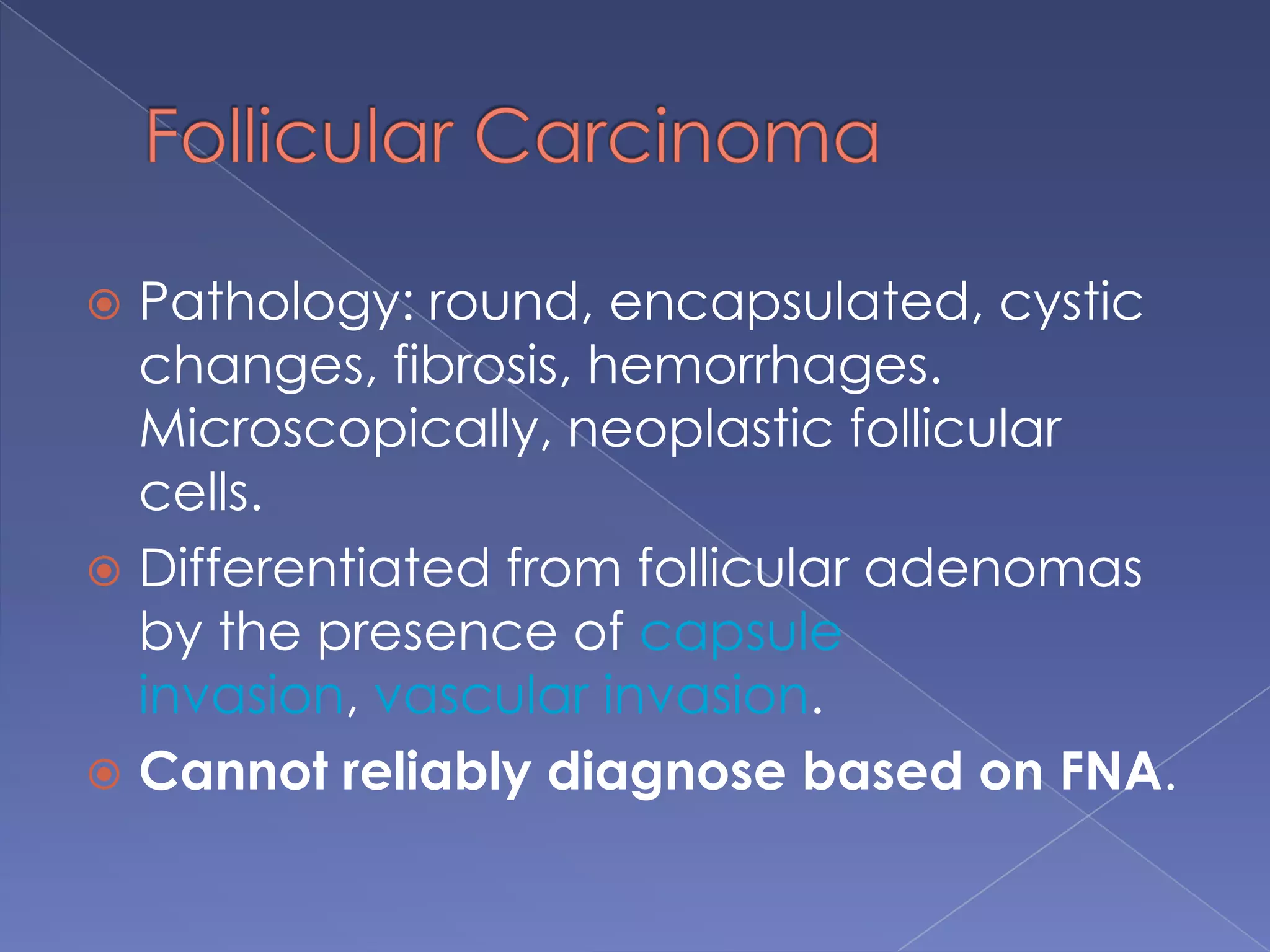
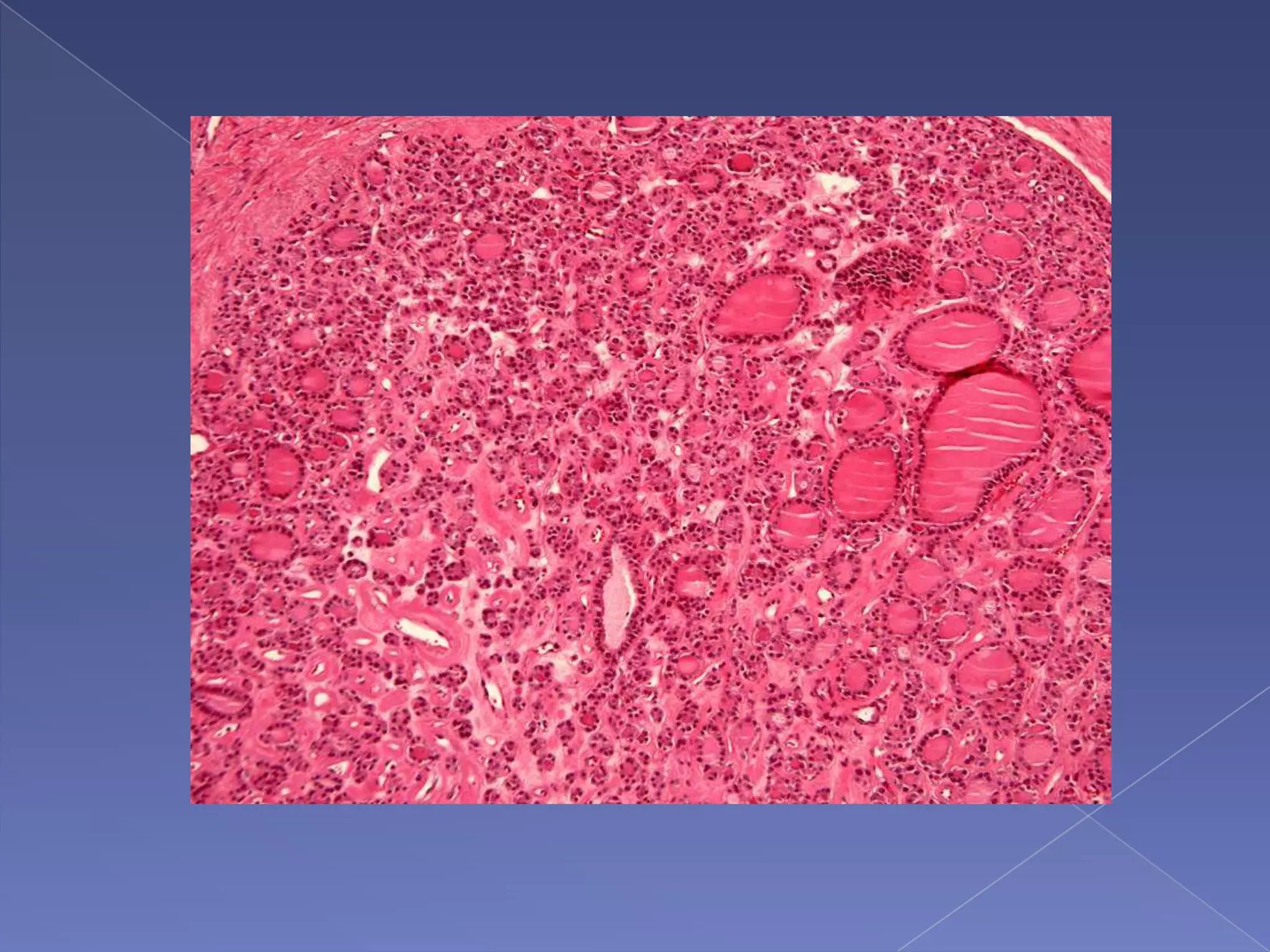
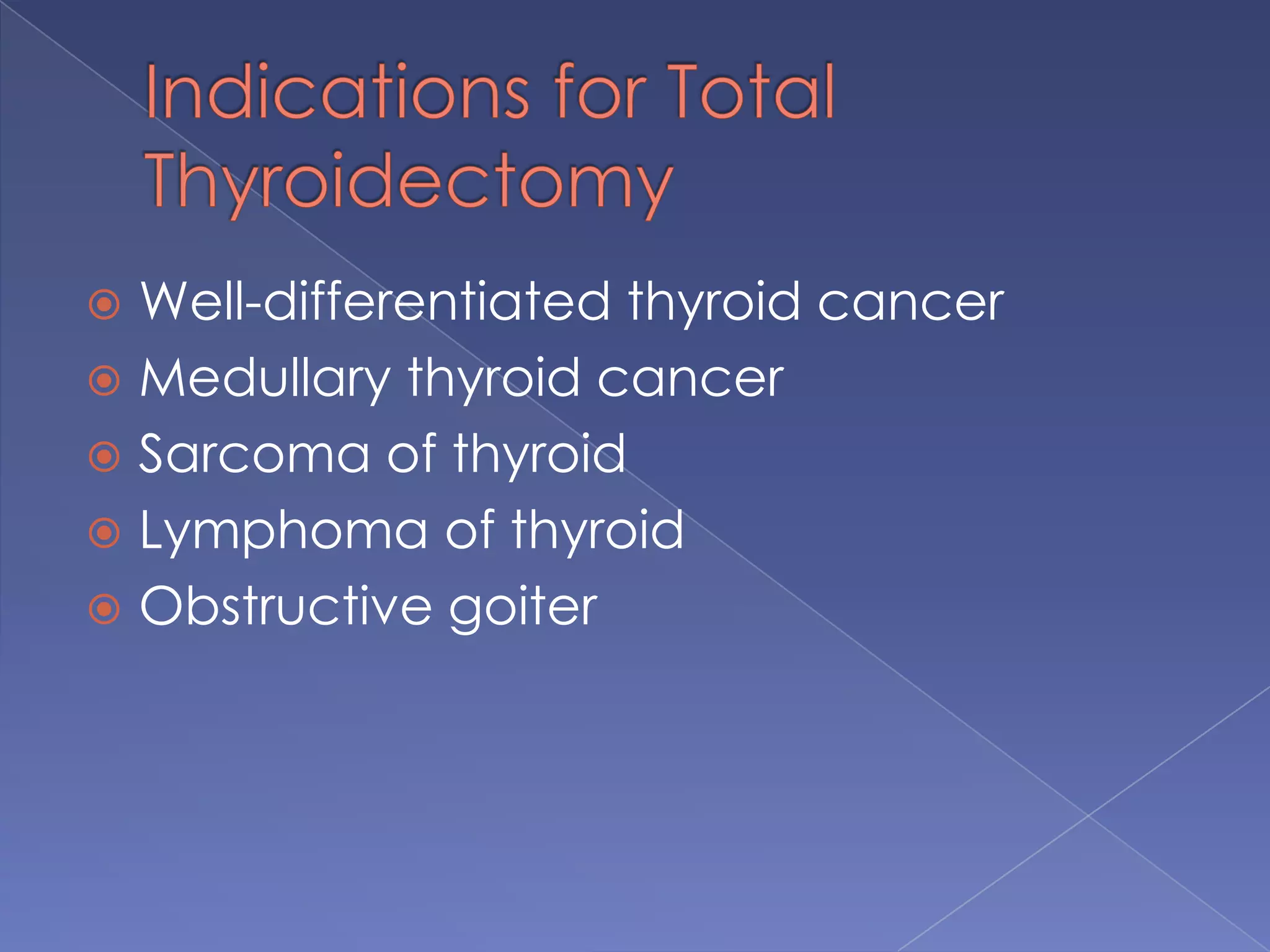
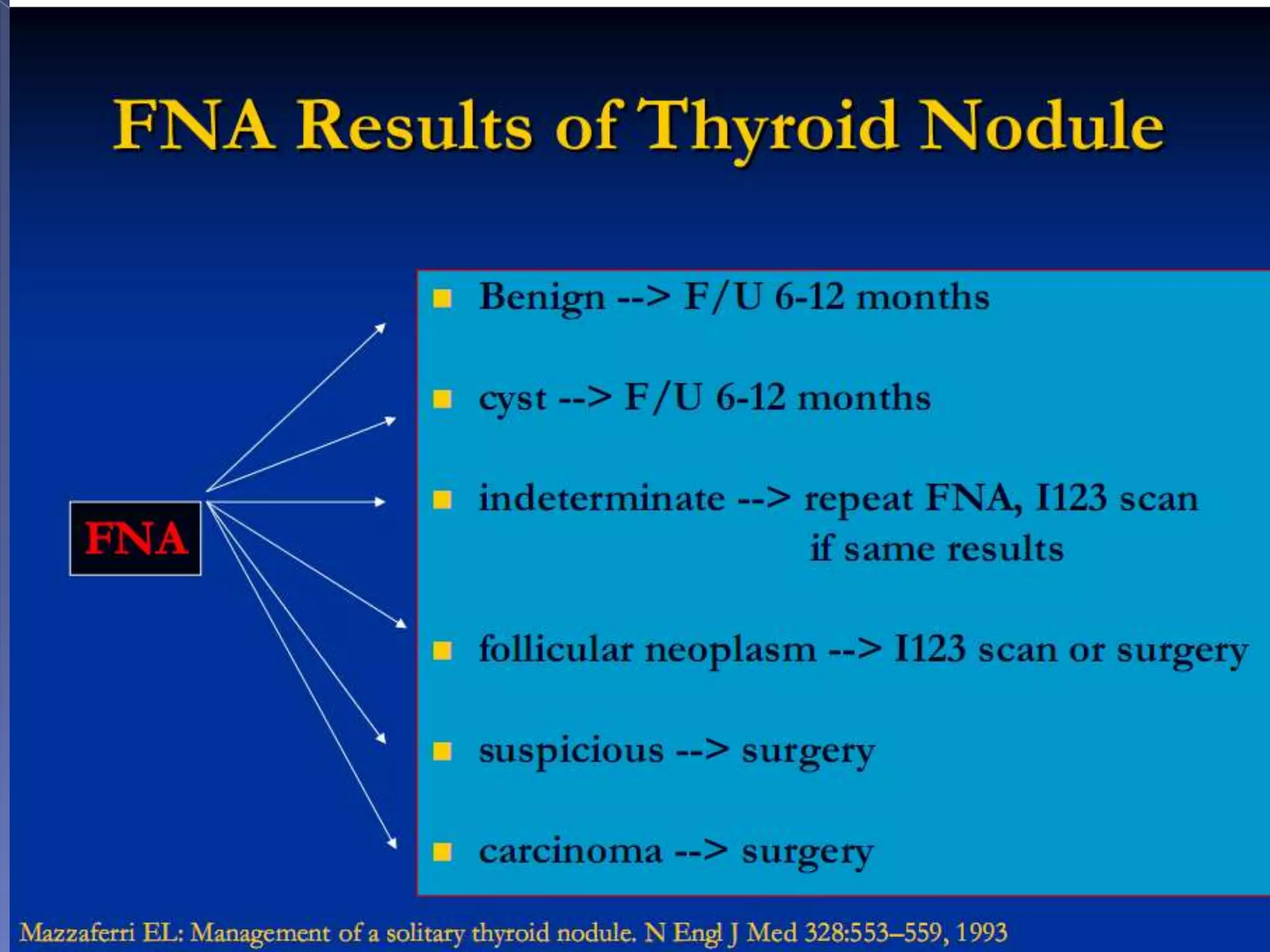
This document discusses thyroid carcinoma and provides details on the anatomy, histology, types, staging, treatment, and prognosis of different thyroid cancers. It covers the embryology, blood supply, innervation and drainage of the thyroid gland. The main types discussed are papillary carcinoma, follicular carcinoma, hurthle cell carcinoma, and medullary carcinoma. Staging systems like TNM, University of Chicago, and MAICS scoring are explained. Treatment typically involves surgical excision and radioactive iodine for differentiated cancers. Prognosis depends on factors like age, histology, tumor size and invasion.