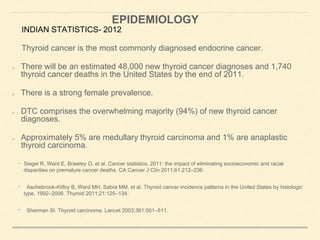
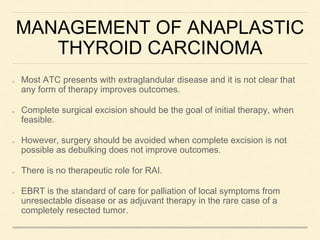
This document discusses the anatomy, physiology, pathology, staging, diagnosis, and treatment of thyroid cancer. Some key points:
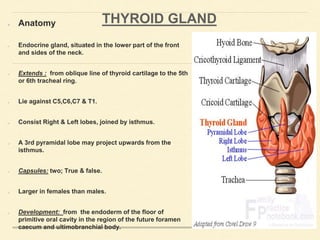
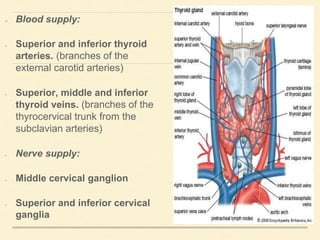
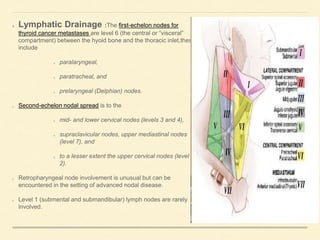
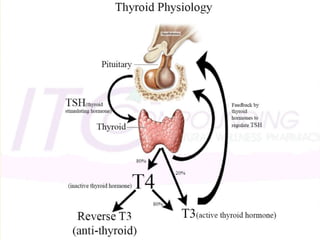
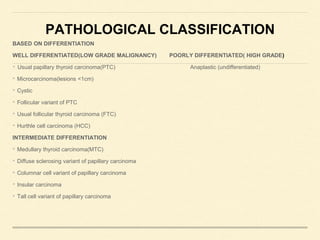
- The thyroid gland is located in the neck and produces thyroid hormones which regulate metabolism. Thyroid cancers are classified based on their level of differentiation.
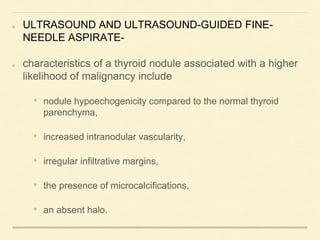
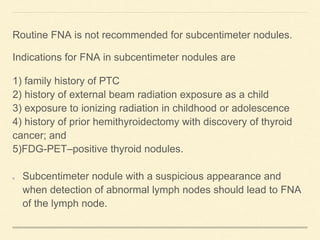
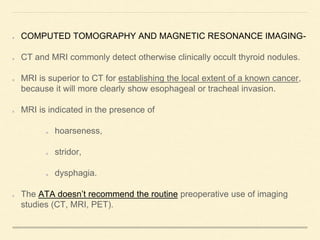
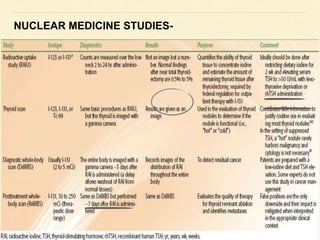
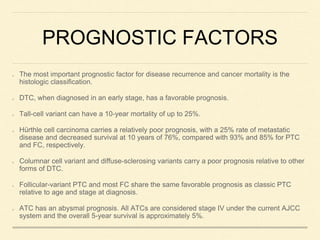
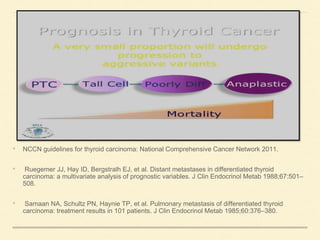
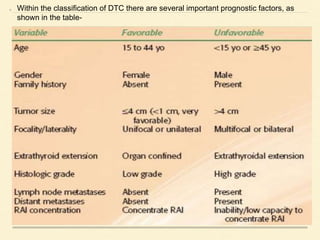
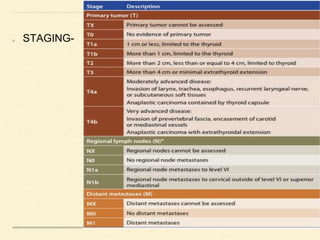
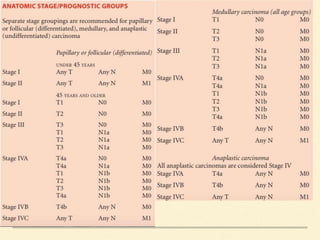
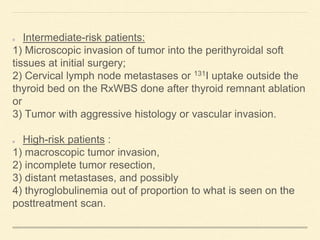
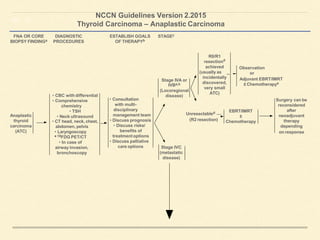
- Diagnostic evaluation includes laboratory tests, ultrasound of the thyroid, and fine needle aspiration if a nodule is detected. Prognostic factors like histology, stage, and tumor size help determine a patient's risk level.
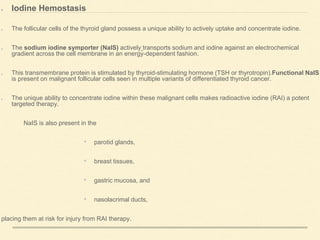
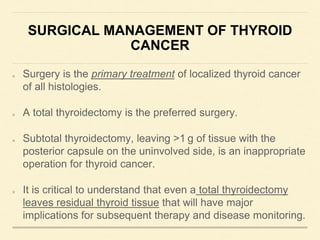
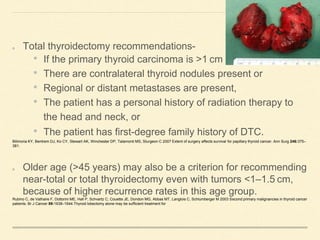
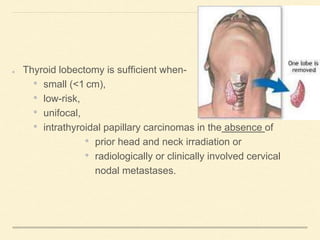
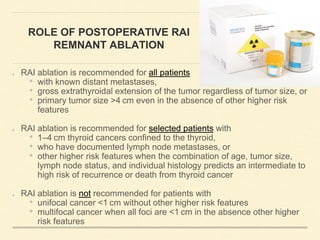
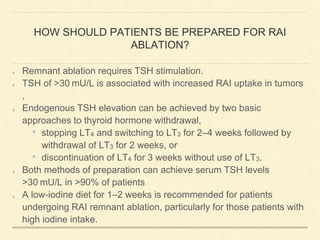
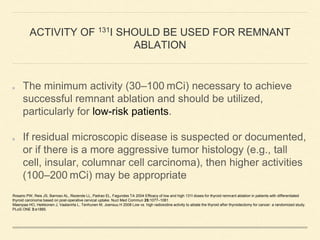
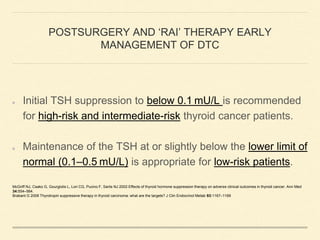
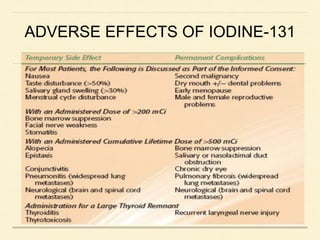
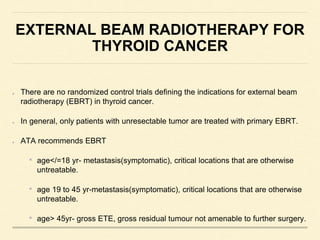
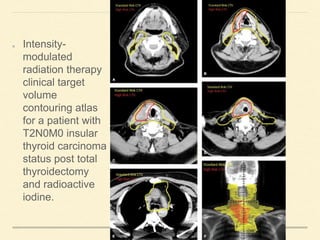
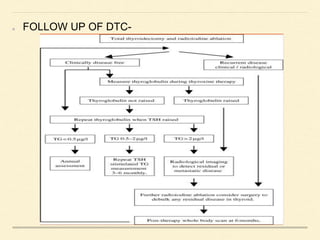
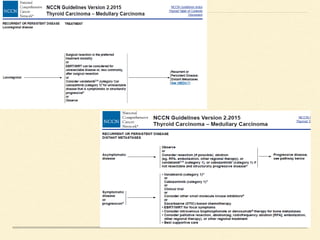
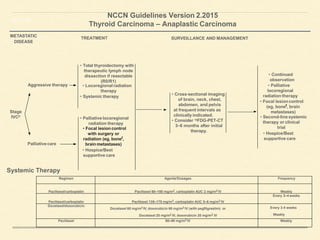
- Surgical treatment typically involves total thyroidectomy. Lymph node dissection may also be performed. Postoperative radioactive iodine remnant ablation is recommended for intermediate- and high-risk