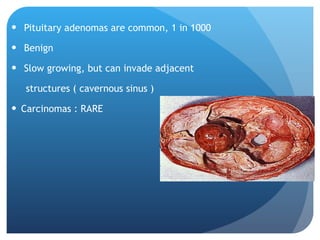
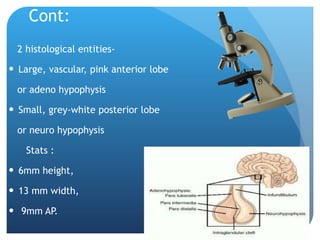
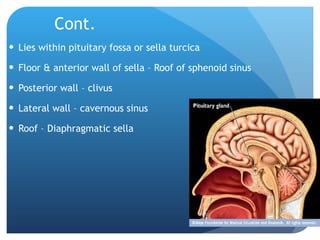
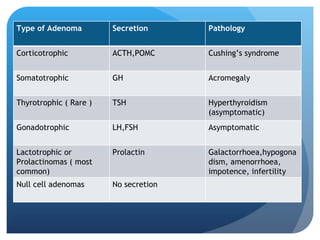
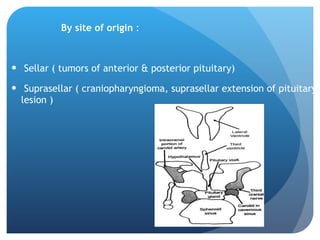
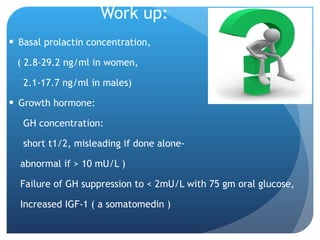
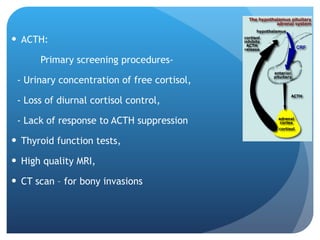
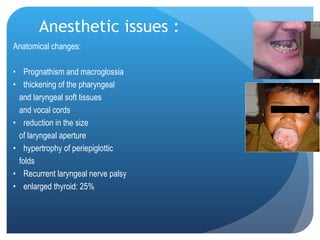
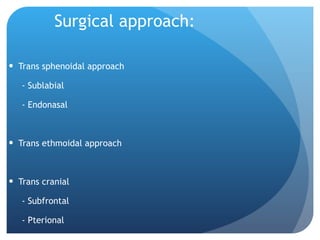
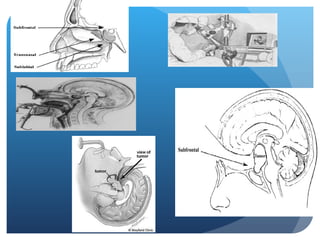
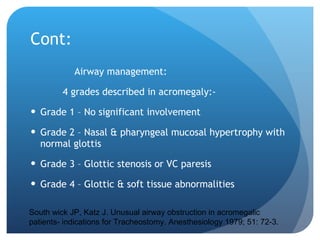
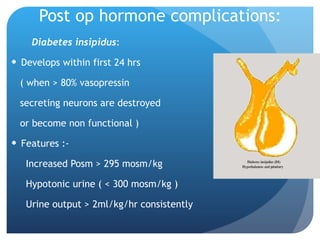
This document discusses anesthesia management for pituitary tumor surgery. Pituitary adenomas are common benign tumors that can invade surrounding structures. Risk factors include genetic conditions. Pre-operative evaluation assesses hormonal levels and effects, as well as comorbidities related to hormonal hypersecretion like acromegaly and Cushing's syndrome. Anesthetic management aims to maintain hemodynamic stability, cerebral oxygenation, and facilitate surgery while preventing complications. Special considerations include potential airway difficulties and post-operative hormone replacement or complications such as diabetes insipidus or hyponatremia.