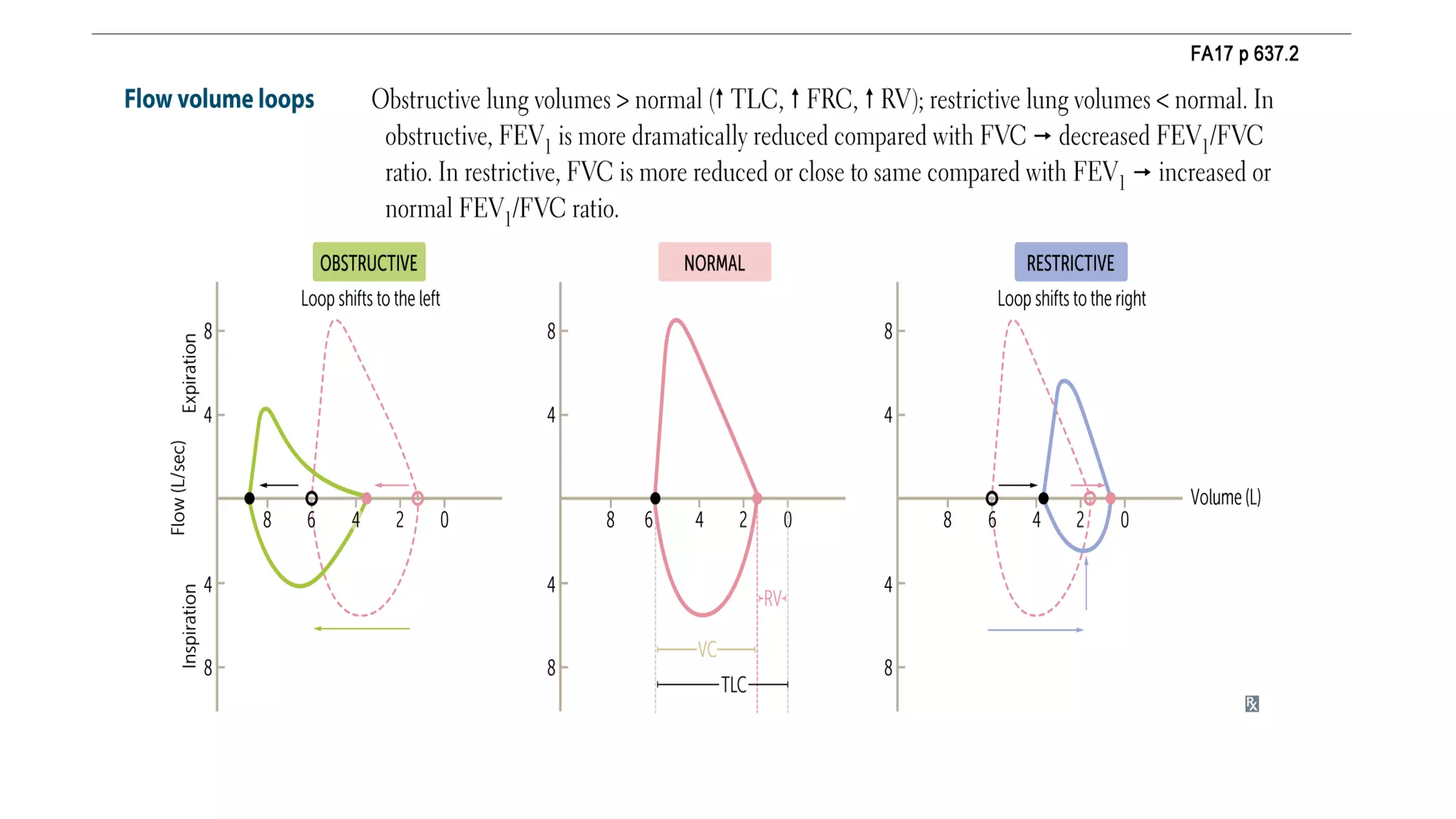
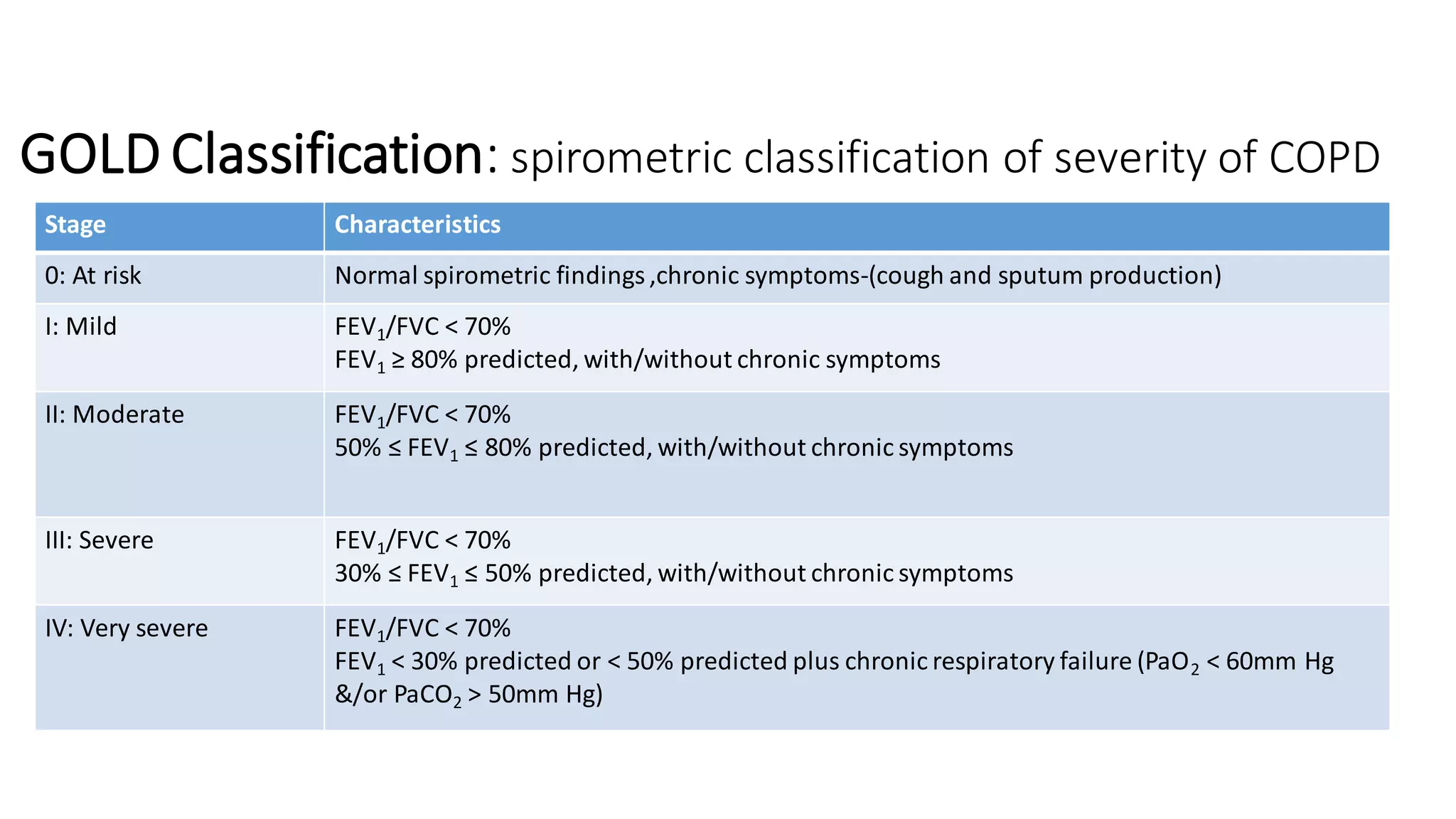
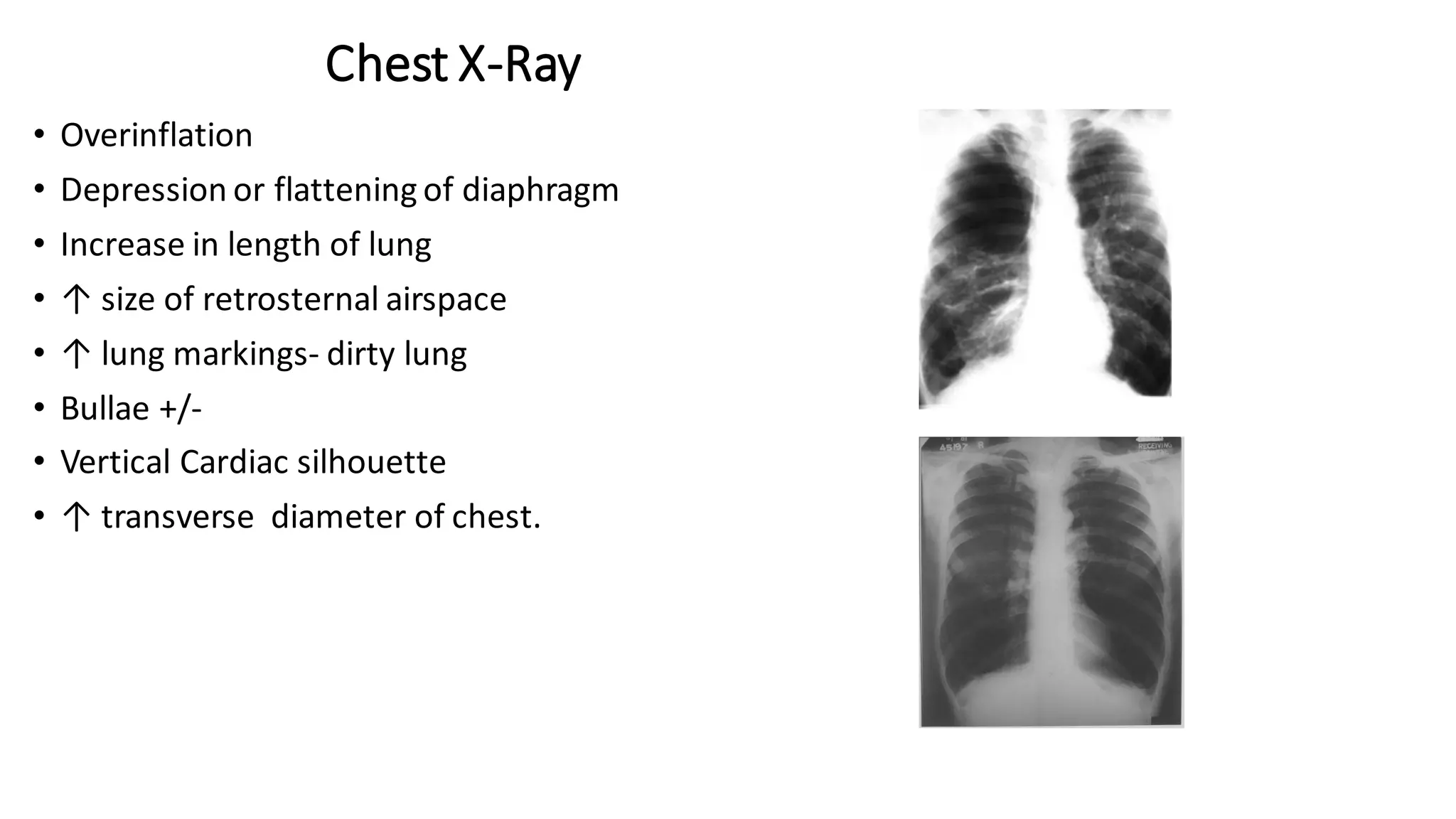
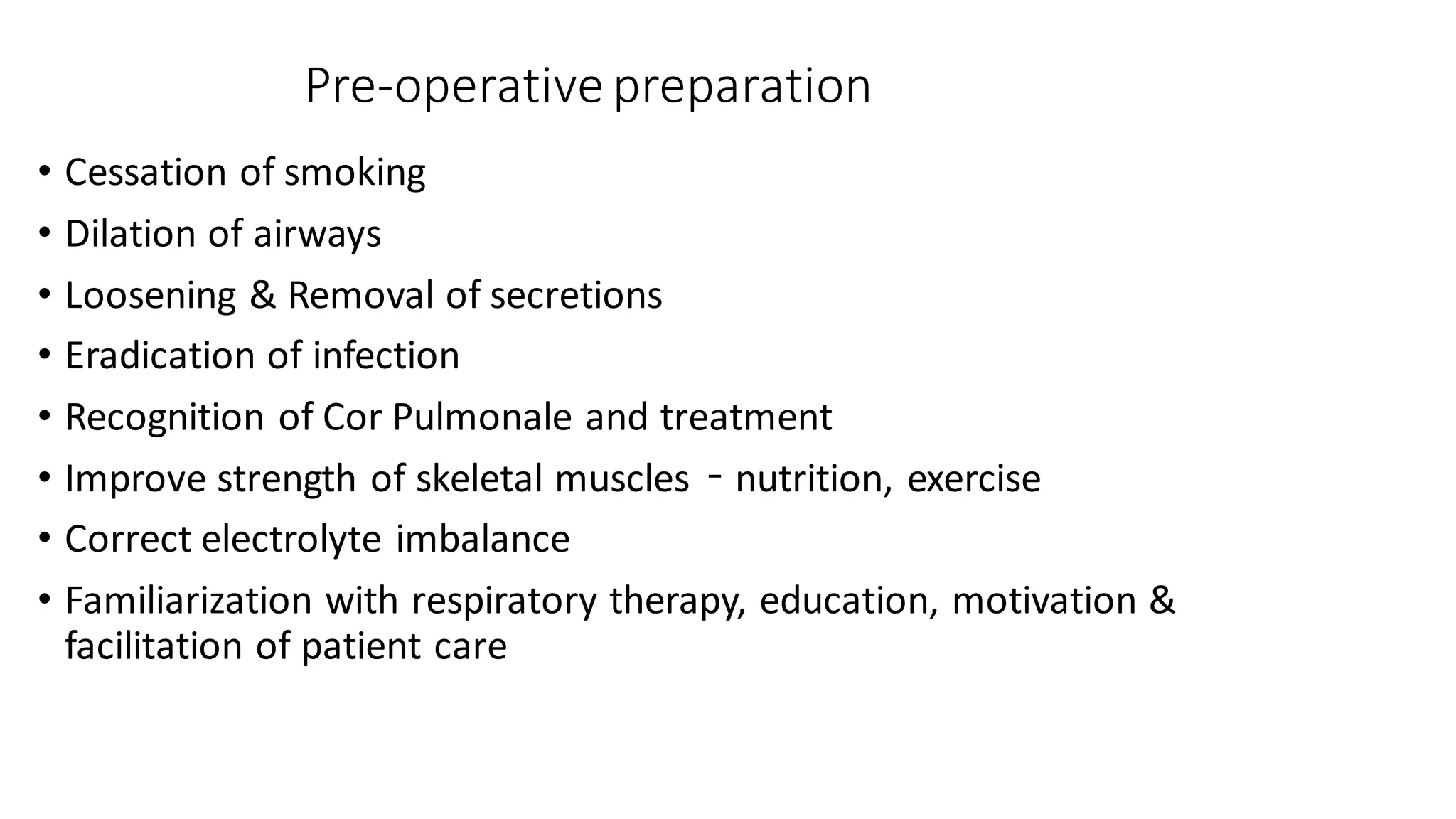
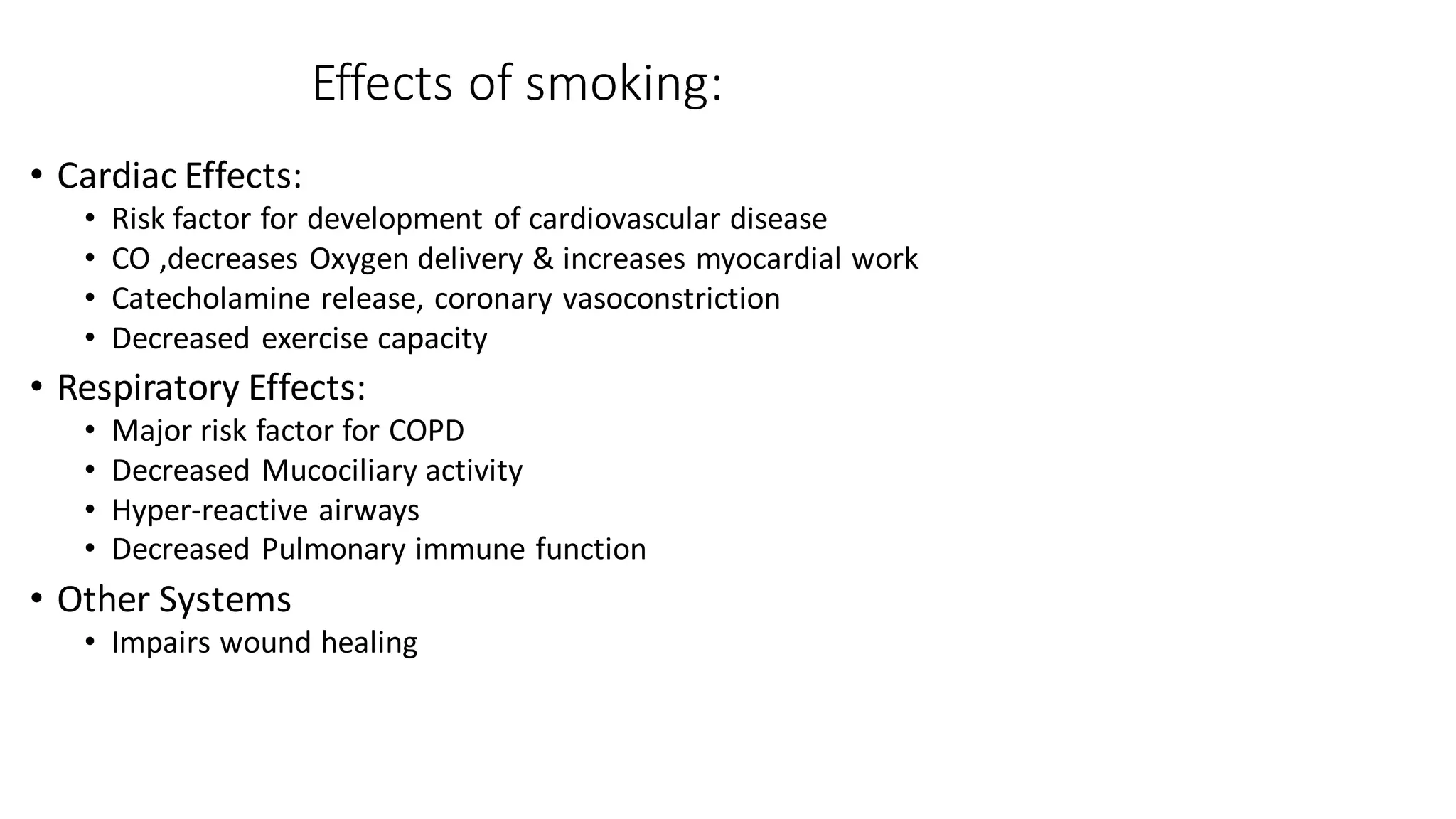
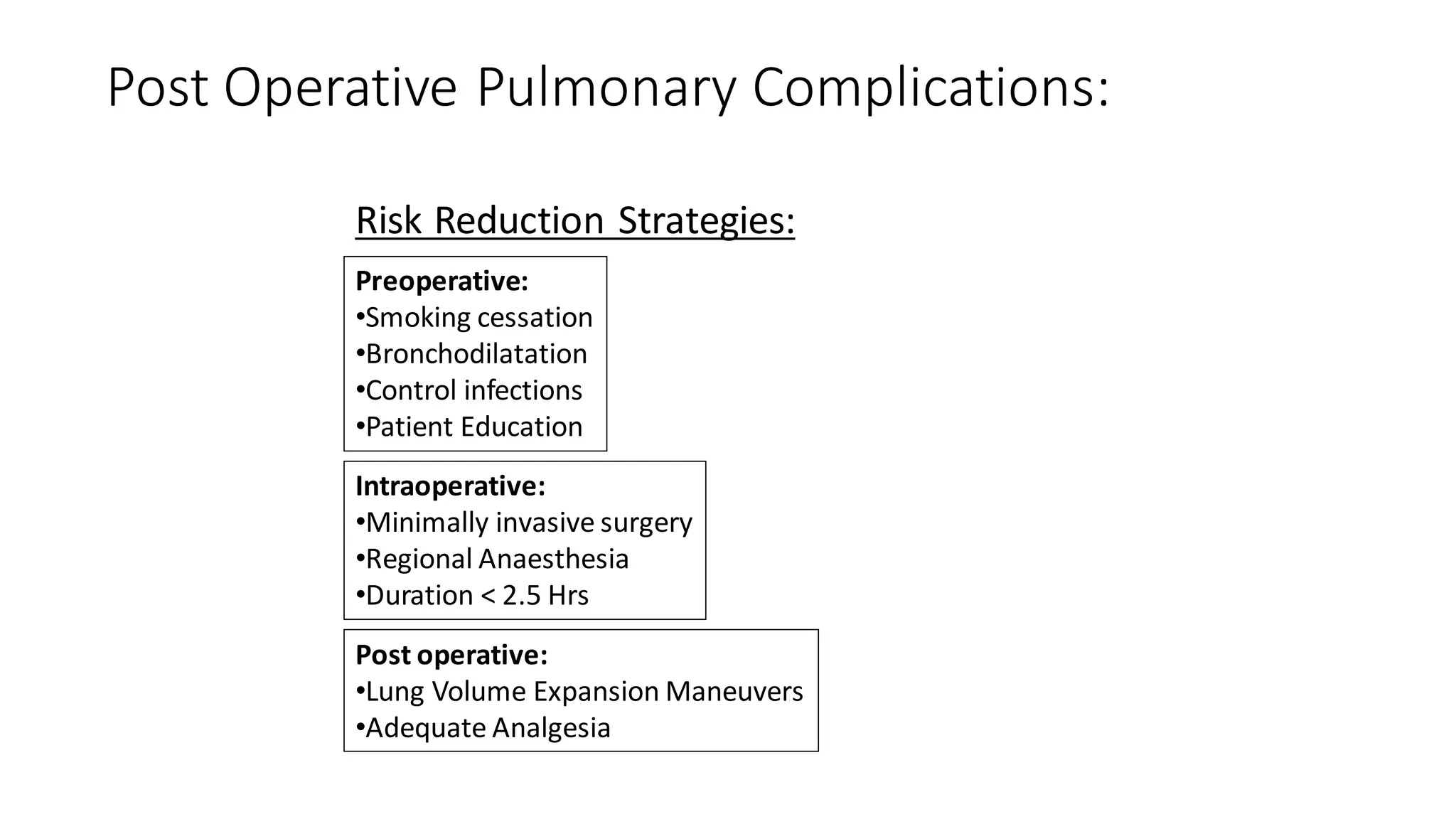
COPD patients pose challenges for anesthesiologists due to increased risk of intraoperative and postoperative complications. The document discusses COPD definitions, pathophysiology, preoperative evaluation including pulmonary function tests, effects of smoking and benefits of smoking cessation. It also covers preoperative preparation including bronchodilation and options for anesthetic technique including benefits of neuraxial anesthesia for COPD patients.