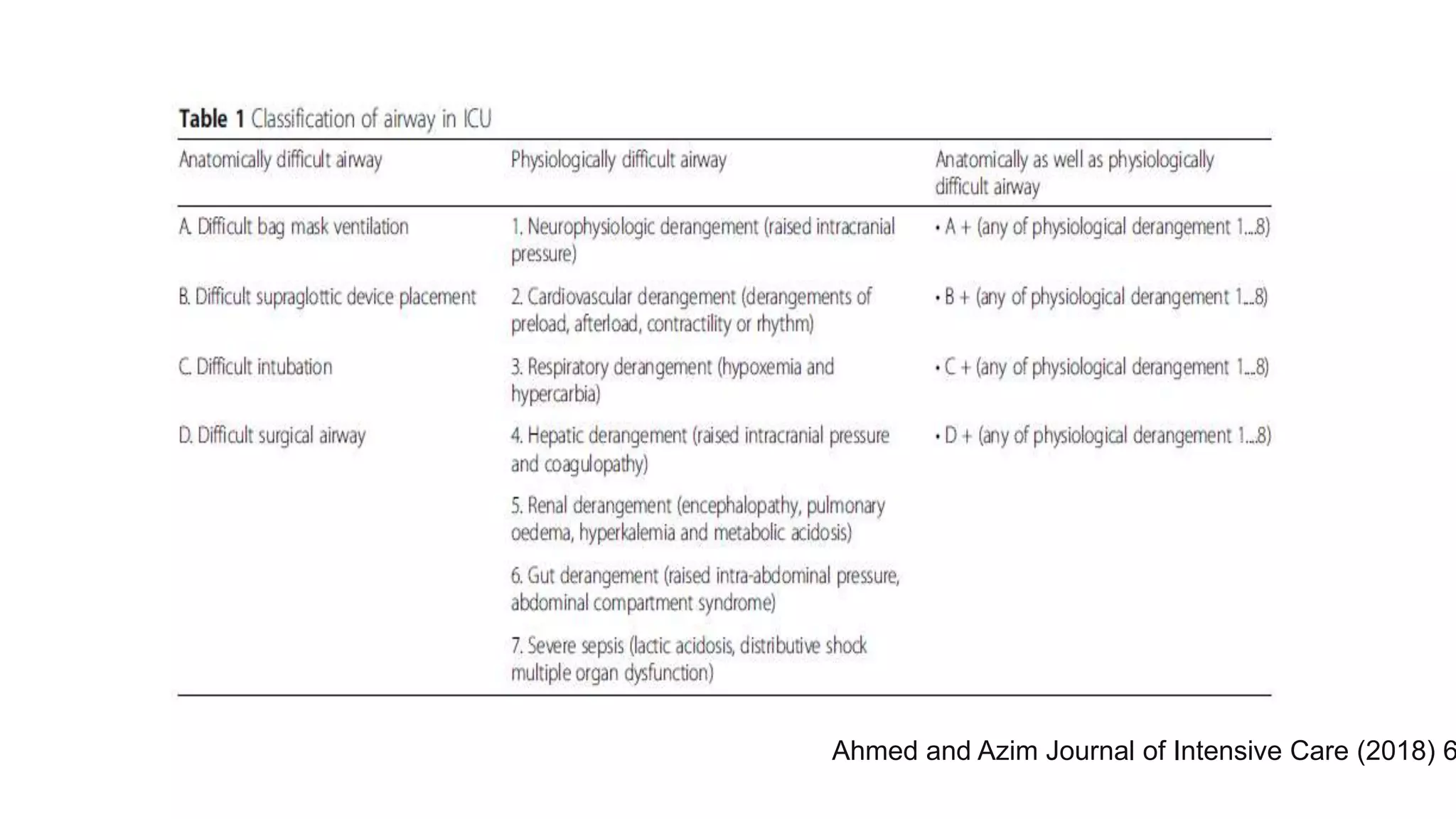
1) The document discusses physiologically difficult airways which are ones where patient physiology makes intubation high risk rather than anatomical issues. Common risks are hypotension, hypoxemia, and right ventricular failure.
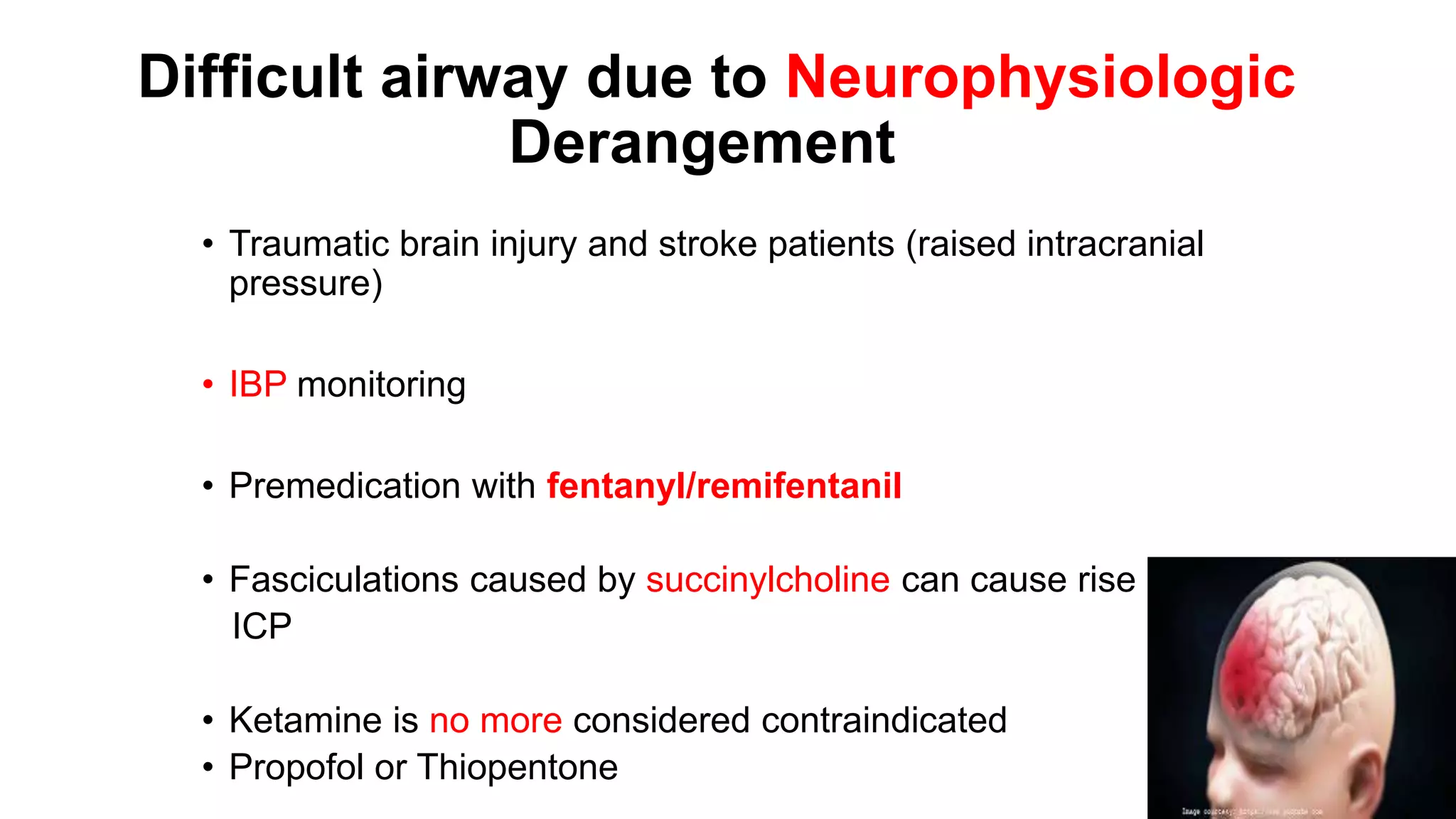
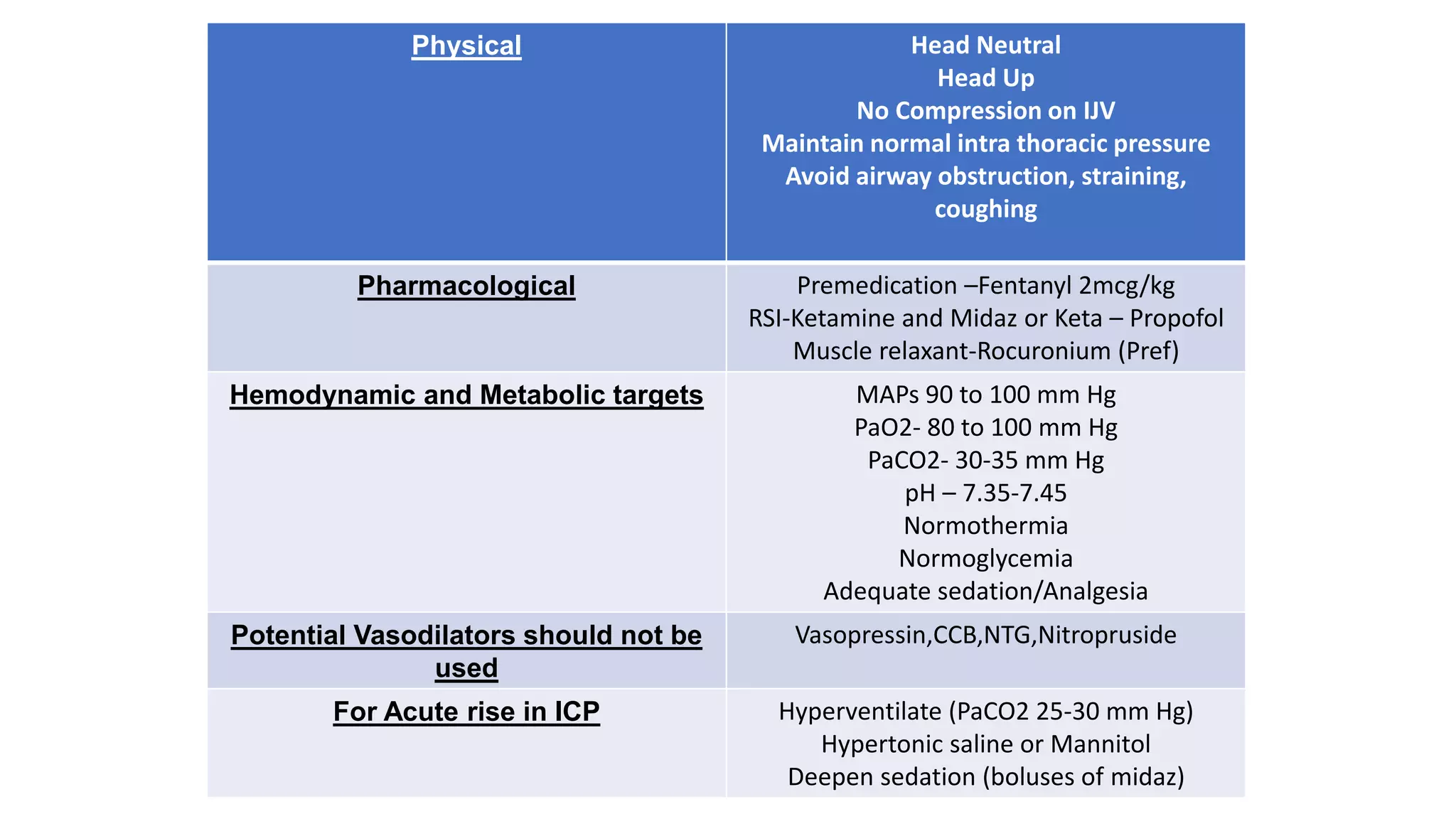
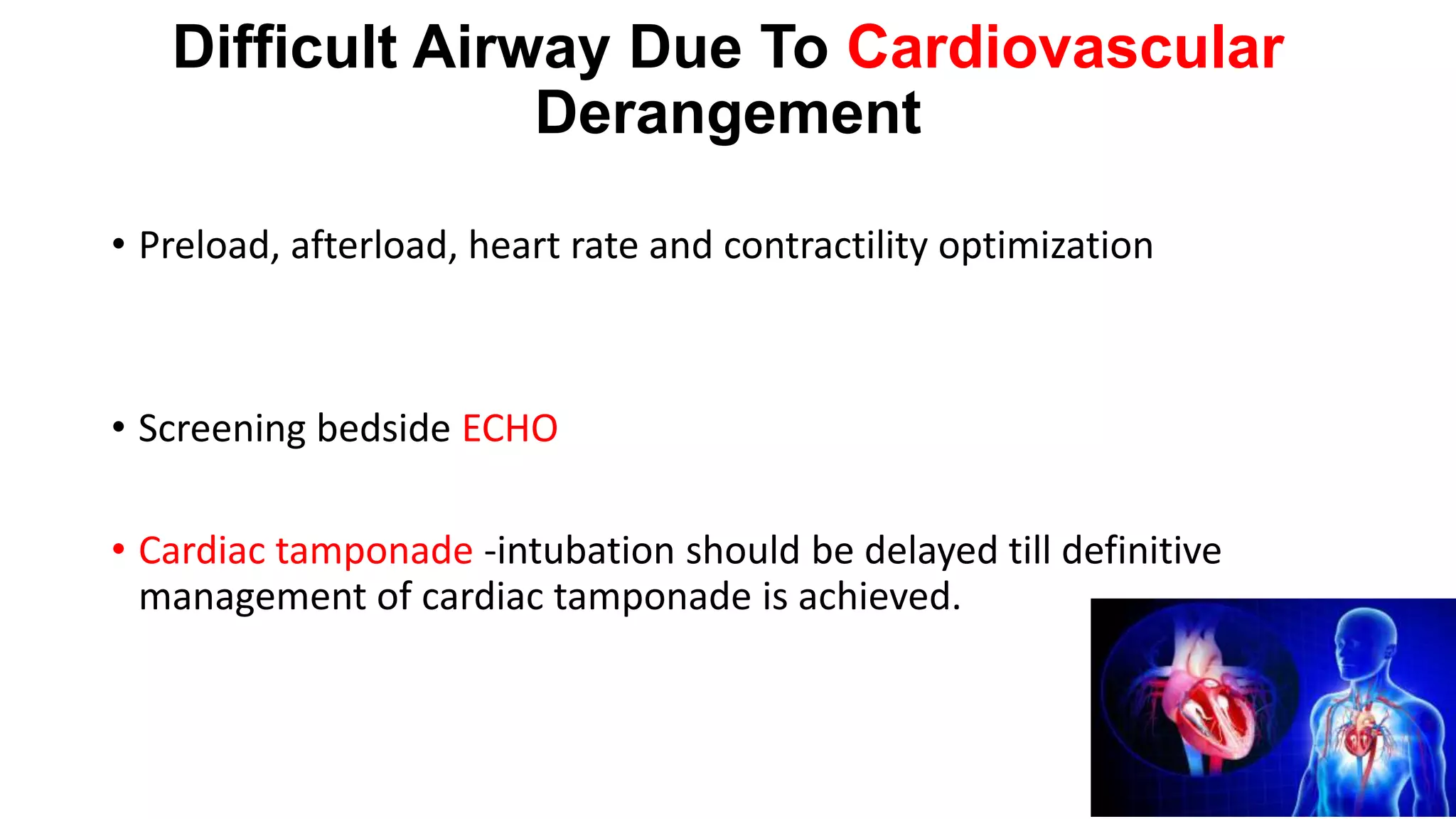
2) Strategies are presented for managing airways complicated by issues like brain injury, cardiovascular problems, respiratory disease, liver or kidney failure, sepsis, and more.
3) The document recommends techniques like rapid sequence intubation, awake intubation, double setup approaches, and having specialized equipment and drugs available to manage difficult airways. Optimizing patient physiology is key to reducing risks of intubation.