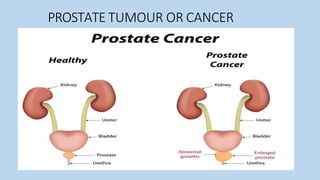
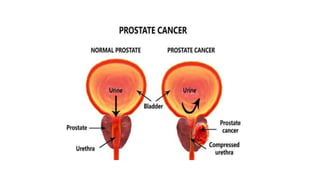
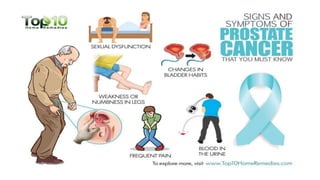
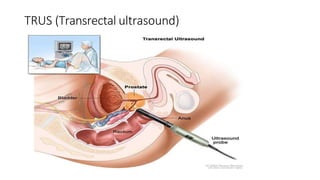
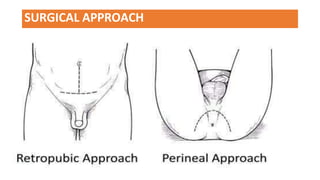
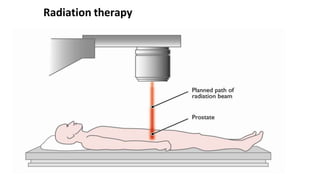
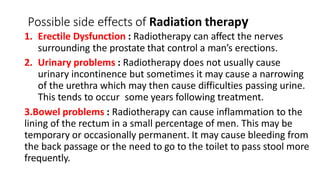
Prostate cancer is the most common malignancy in men, particularly affecting those over 65. Risk factors include age, family history, diet high in fats, obesity, smoking, and alcohol. Diagnosis involves techniques such as digital rectal examinations and PSA testing, with treatment options varying from watchful waiting to radical prostatectomy based on disease stage and patient condition.