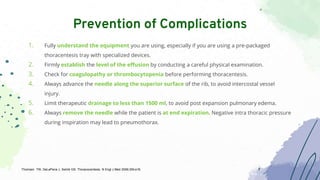
1. Thoracentesis is a procedure to remove fluid from the pleural cavity for diagnostic or therapeutic purposes using a needle. It has few contraindications and complications can include pain, bleeding and pneumothorax.
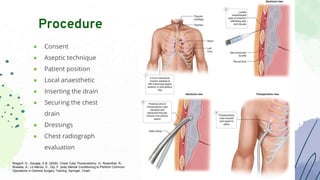
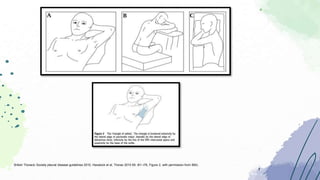
2. Chest tubes are flexible tubes inserted into the pleural space to drain fluid or air. They are used for large pneumothoraces or complicated pleural effusions. Complications include bleeding, infection and re-expansion pulmonary edema.
3. Indwelling pleural catheters are long term soft silicone tubes that allow recurrent pleural effusions to be drained outside the hospital. They are useful for malignant or trapped lung effusions. Complications include pain, infection and block
![● Thoracentesis is a procedure that is performed to remove fluid or air from the thoracic
cavity for both diagnostic and/or therapeutic purposes.
Thoracentesis
Wiederhold BD, Amr O, Modi P, et al. Thoracentesis. [Updated 2022 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK441866/
Diagnostic
• Effusion with unknown etiology
• Malignancy or infection
• First time thoracentesis
Therapeutic
• Large effusion with clinically
significant symptomps
Contraindication
• Absolute - none
• Relative
• Uncontrolled coagulation deficit
• Unsafe positioning
• Mechanical ventilation](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-4-320.jpg)
![1. Patient education and consent
2. Equipment (needle 16-20 G, syringe 10 mL, 5
mL, 20 mL, antiseptic, lidocaine, drainage
bag, sterile towels)
3. Positioning (leaning slightly forward and
resting the head on the arms or hands or on
a pillow
● An invasive procedure → semi-sterile field
● Effusion estimation → absent sounds on
auscultation, dullness to percussion, and
decreased or absent fremitus
● Bedside USG → puncture site
Procedure
Wiederhold BD, Amr O, Modi P, et al. Thoracentesis. [Updated 2022 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK441866/](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-5-320.jpg)
![● Preferred site :
○ Either the midaxillary line if the procedure is being performed in the supine position
○ Posterior midscapular line if the procedure is being performed in the upright or seated position.
1. Bedside ultrasound to identify an appropriate location for the procedure
2. Prep and drape the patient in a sterile fashion.
3. Cleanse the skin with an antiseptic solution.
4. Administer local anesthesia to the skin (make a wheal in the skin surface)
5. Continue infiltration of local anestesia to the tissue around the rib, marching the needle tip just above the
rib margin
6. Proof puncture
7. Mark the puncture spot
8. Use a larger gauge needle connected to a three way (syringe and collection tube)
9. Collect pleural effusion using syringe and if necessary, drain larger effusion into a plastic drainage bag
Technique and Steps
Wiederhold BD, Amr O, Modi P, et al. Thoracentesis. [Updated 2022 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK441866/](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-6-320.jpg)
![● Bleeding, pain, and infection at the point
of needle entry
● Re-expansion pulmonary edema
● Splenic and hepatic puncture
● Pneumothorax (most common)
○ Indications of chest tube placement
to manage the pneumothorax
following thoracentesis :
1. large pneumothorax
2. progressive
3. symptomatic pneumothorax
Complications
Wiederhold BD, Amr O, Modi P, et al. Thoracentesis. [Updated 2022 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK441866/
National Heart, Lung and Blood Institute ( PD-US NIH)](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-7-320.jpg)
![● A flexible tube that can be inserted through the chest wall between the ribs into the
pleural space.
Chest Tube
Ravi C, McKnight CL. Chest Tube. [Updated 2021 Oct 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK459199/
Indication
• Pneumothorax: persistent/recurrent, tension, large
secondary spontaneous pneumothorax (>2cm),
iatrogenic
• Pleural fluid: malignancy, empyema and
complicated parapneumonic pleural effusion
• Traumatic pneumothorax or hemopneumothorax
• Peri-operative: thoracotomy, esophageal surgery,
cardiothoracic surgery
Contraindication
• Absolut - none
• Relative:
• Pulmonary adhesions from previous surgery,
pulmonary disease, and/or trauma.
• Coagulopathy and diaphragmatic hernias](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-11-320.jpg)
![● Bleeding, superficial site infection
● Deep organ space infection (empyema)
● Dislodgement of the tube
● Clogging of the tube
● Re-expansion pulmonary edema
● Injury to intraabdominal and intrathoracic
organs
Complications
● No air leak is visualized
● Output is serohemorrhagic with no signs of
bleeding
● Output is less than 150 cc to 400 cc over a 24-
hour period (debatable)
● Nonexistent or stable mild pneumothorax on
chest x-ray
● Patient is minimized on positive pressure from
the ventilator
Discontinuation
Ravi C, McKnight CL. Chest Tube. [Updated 2021 Oct 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK459199/](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-14-320.jpg)
![● A long-term soft silicone tubes that allow patients with recurrent pleural effusions (usually
malignant pleural effusions) to be brought outside hospital care
● Talc pleurodesis and indwelling pleural catheters are the standard therapeutic options for patients
presenting with symptomatic malignant pleural effusions
● Indwelling catheters are particularly useful in patients with trapped lung or failed pleurodesis.
IPC
Sivagnaname, Y. , Krishnamurthy, D. , Radhakrishnan, P. , Selvam, A. M. . Indwelling Pleural Catheters. In: Sandri, A. , editor. Pleura - A Surgical Perspective [Internet].
London: IntechOpen; 2021 [cited 2022 Sep 15]. Available from: https://www.intechopen.com/chapters/79289 doi: 10.5772/intechopen.100645](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-16-320.jpg)

![IPC
Indication
•Recurrent pleural effusion due to malignant
etiology.
•Trapped lung with symptomatic pleural effusions.
•Recurrent pleural effusion due to benign
etiologies:
•Hepatic hydrothorax
•Chylothorax
•CKD related effusions, loculated effusions and
empyema
Contraindication
•Inability for the patient and care givers to handle
or tolerate the drain.
•Significant coagulopathy
•Parapneumonic effusion/empyema.
•Local cellulitis in the insertion site.
•Individuals in immunocompromised state due to
systemic diseases.
Sivagnaname, Y. , Krishnamurthy, D. , Radhakrishnan, P. , Selvam, A. M. . Indwelling Pleural Catheters. In: Sandri, A. , editor. Pleura - A Surgical Perspective [Internet].
London: IntechOpen; 2021 [cited 2022 Sep 15]. Available from: https://www.intechopen.com/chapters/79289 doi: 10.5772/intechopen.100645](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-18-320.jpg)
![Immediate
● Small pneumothorax
● Subcutaneous
emphysema
● Pain, bleeding
Late
● Infections
● Catheter tract
metastasis
● Catheter fracture
● IPC blockage
● Leakage
Complications
Drainage
● At least 3 times a week or
in presence of symptoms
● Normal drainage timing
may last for 15–20 min
Removal
● Pleural sepsis
● Nonfunctional/defective
IPC
● Severe pain with local
cellulitis
● Usually not necessary,
especially in spontaneous
pleurodesis
Drainage and Removal
Sivagnaname, Y. , Krishnamurthy, D. , Radhakrishnan, P. , Selvam, A. M.Indwelling Pleural Catheters. In: Sandri, A., editor. Pleura - A Surgical Perspective [Internet].
London: IntechOpen; 2021 [cited 2022 Sep 15]. Available from: https://www.intechopen.com/chapters/79289 doi: 10.5772/intechopen.100645](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-19-320.jpg)

![● A minimally invasive way to obtain a cell sample for diagnosis, an alternative to more invasive
methods such as incisional or excisional biopsy.
● Common sites of aspiration: breast, thyroid, superficial lymph nodes, or skin masses
FNA
Sigmon DF, Fatima S. Fine Needle Aspiration. [Updated 2022 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK557486/
Indication
• Confirm suspected reactive
hyperplasia
• Diagnose a specific infection
• Diagnose a neoplastic infiltration
• Unknown primary
Contraindication
• Absolute - none
• Relative - Risk outweighs benefit
• Bleeding diathesis
• Carotid body tumour
• High risk respiratory compromise](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-21-320.jpg)
![• Bleeding
• Damage to surrounding
structures
• Fistula
• Seed tissue with infection
or neoplastic cells (rare)
• No hospitalisation – outpatient
procedure
• No sutures or scars
• Minimal pain
• Inexpensive
• Less morbidity
Advantages
Complications
Sigmon DF, Fatima S. Fine Needle Aspiration. [Updated 2022 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK557486/](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-23-320.jpg)

![● A rapid method used to achieve definitive diagnosis for most thoracic lesions, whether the
lesion is located in the pleura, the lung parenchyma, or the mediastinum.
● Usually guided by ultrasound or CT
● Work up of lesions using cytopathology, histopathology, or microbiologic examination
TTNA/TTB
Indication
• Metastatic, inoperable, or recurrent neoplastic
disease
• Obtain material for culture of suspected infection
• Lung nodule, unfit for surgery
Contraindication
• Uncooperative patient
• Incorrectable bleeding
• Contraindications to sedation
• Pulmonary hypertension, incorrectable hypoxemia
• Deep lesions are not contraindication
Young M, Shapiro R. Lung Biopsy. [Updated 2022 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK513290/](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-25-320.jpg)
![● Pneumothorax
● Hemorrhage/Hemoptysis
○ puncturing a pulmonary cavity or enlarged bronchus
○ patient can be placed biopsy side down
○ consider bronchoscopic tamponade of the lobar bronchus, bronchial artery embolization,
pulmonary artery embolization, and surgery.
● Air embolism
○ trocar has been removed from a needle tip located in a pulmonary vein and/or 2) iatrogenic
creation of a bronchovenous fistula.
○ signs of a stroke or seizure
○ Patient should be in left lateral decubitus position
● Needle-track seeding with malignant cells
Complications
Young M, Shapiro R. Lung Biopsy. [Updated 2022 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK513290/](https://image.slidesharecdn.com/dtbasicintpulm-221015113941-a3a6e199/85/DT-Basic-Int-Pulm-pptx-28-320.jpg)
