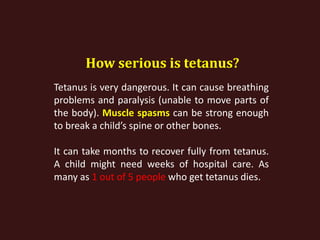
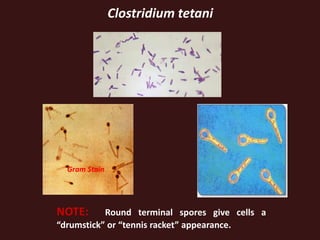
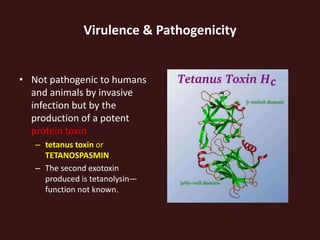
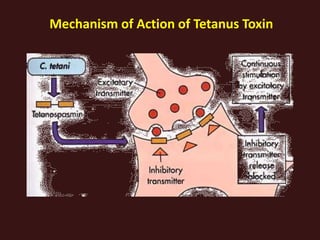
Tetanus, caused by the bacterium Clostridium tetani, is a life-threatening infection of the nervous system that leads to symptoms such as muscle spasms, paralysis, and potentially death due to respiratory complications. It can be prevented through vaccination, with booster shots needed every ten years, but still poses a significant health risk globally, especially in unimmunized populations. Treatment involves antibiotics, wound care, and supportive measures, with a high mortality rate if not treated promptly.