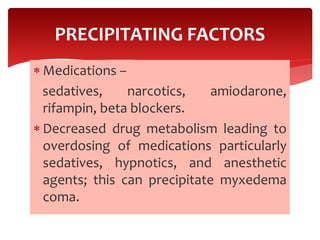
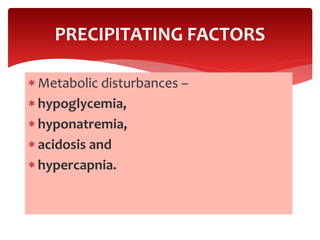
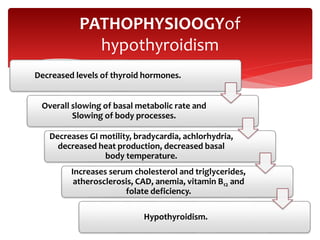
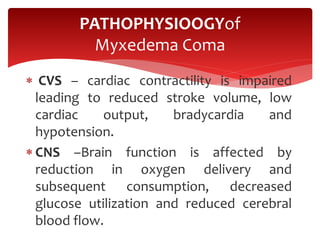
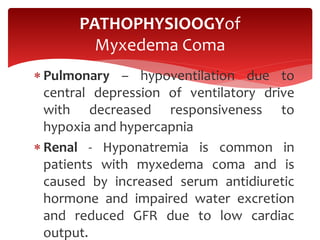
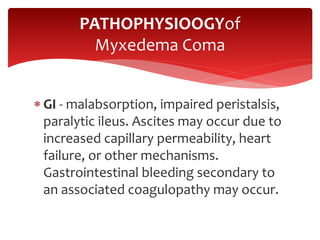
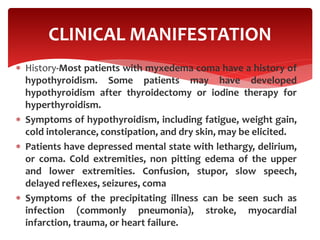
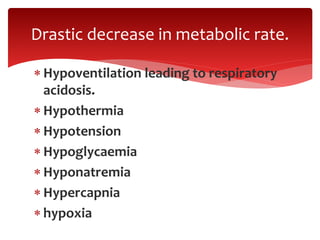
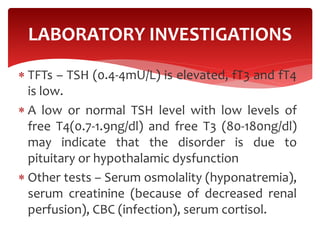
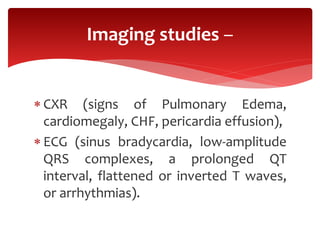
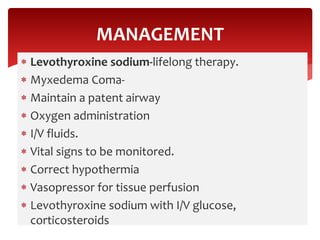
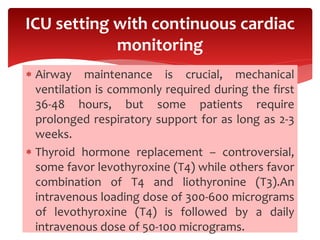
Myxedema coma is a rare, life-threatening condition resulting from severe hypothyroidism, characterized by hypothermia and unconsciousness, often occurring in older women during winter. It can be precipitated by factors such as infections, trauma, and certain medications, leading to significant metabolic disturbances and multi-organ dysfunction. Management includes airway support, intravenous levothyroxine, and monitoring for complications, with a focus on correcting hypothermia and electrolyte imbalances.