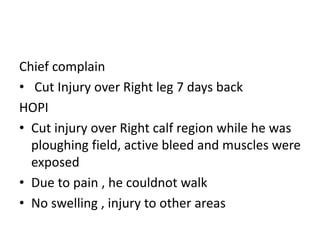
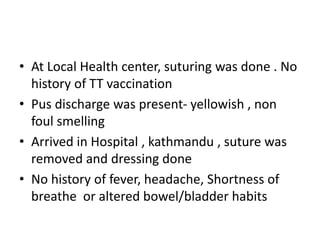
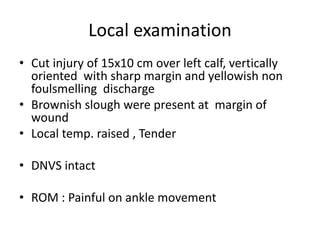
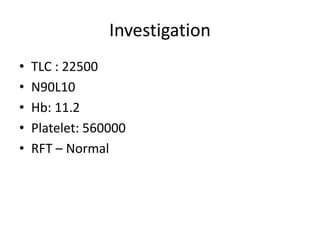
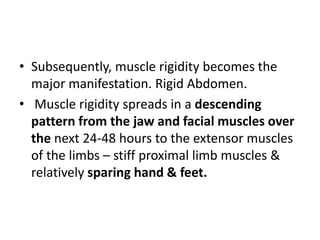
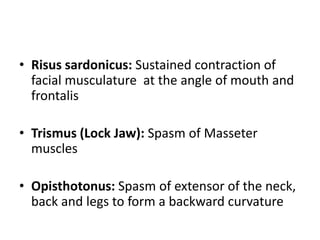
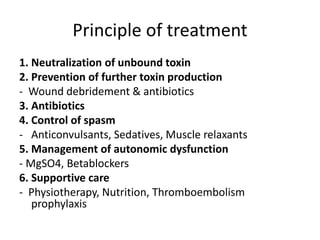
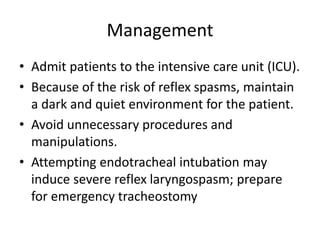
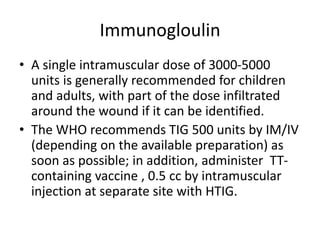
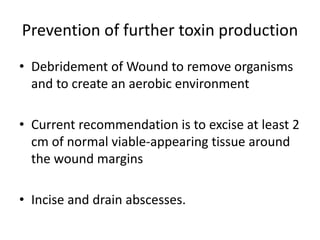
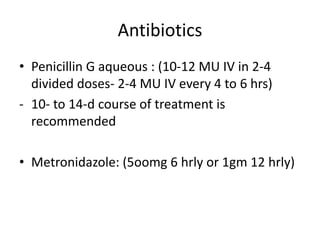
This document presents a case report of a 50-year-old male farmer who was admitted to the hospital with symptoms of tetanus. He had sustained a deep cut on his right calf while working in his field one week prior that had been sutured at a local health center. On admission, he exhibited stiffness of the neck muscles and inability to open his mouth. He was diagnosed with tetanus and admitted to the intensive care unit for management. Treatment included wound debridement, antibiotics, tetanus immunoglobulin, sedation and muscle relaxants. Tetanus is a vaccine-preventable neurological disease caused by Clostridium tetani spores entering the body through wounds. It causes painful muscle