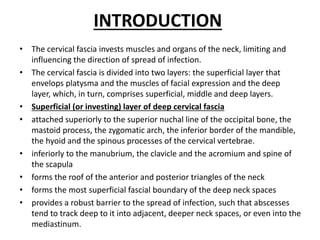
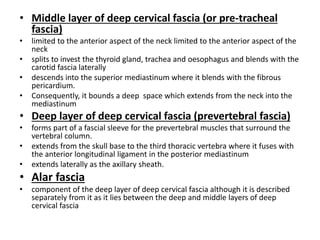
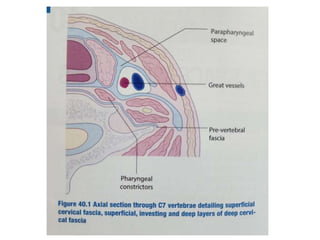
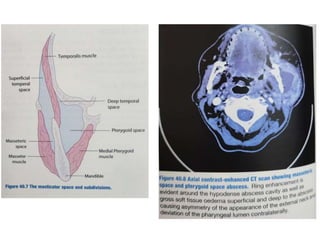
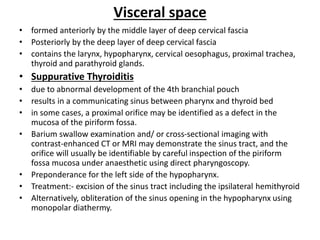
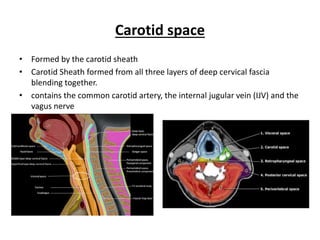
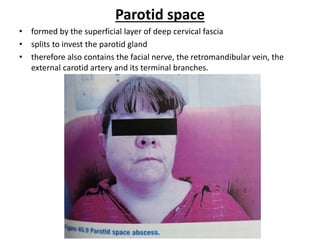
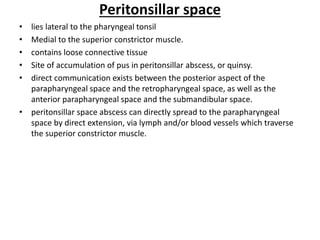
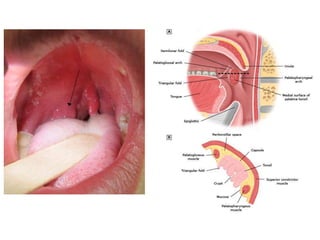
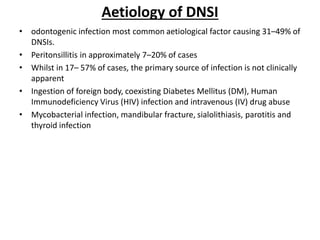
The document provides an overview of deep neck spaces and infections that can occur within these spaces. It discusses the layers of cervical fascia that divide the neck into various spaces. Some key spaces mentioned include the parapharyngeal, retropharyngeal, masticator, visceral, and carotid spaces. Common causes of deep neck space infections are discussed. Clinical features, investigations including imaging, and treatment approaches like antibiotics and surgical drainage are summarized. Maintaining a patent airway is emphasized as critical, and tracheostomy may be needed in some severe cases to protect the airway. Complications are also reviewed.