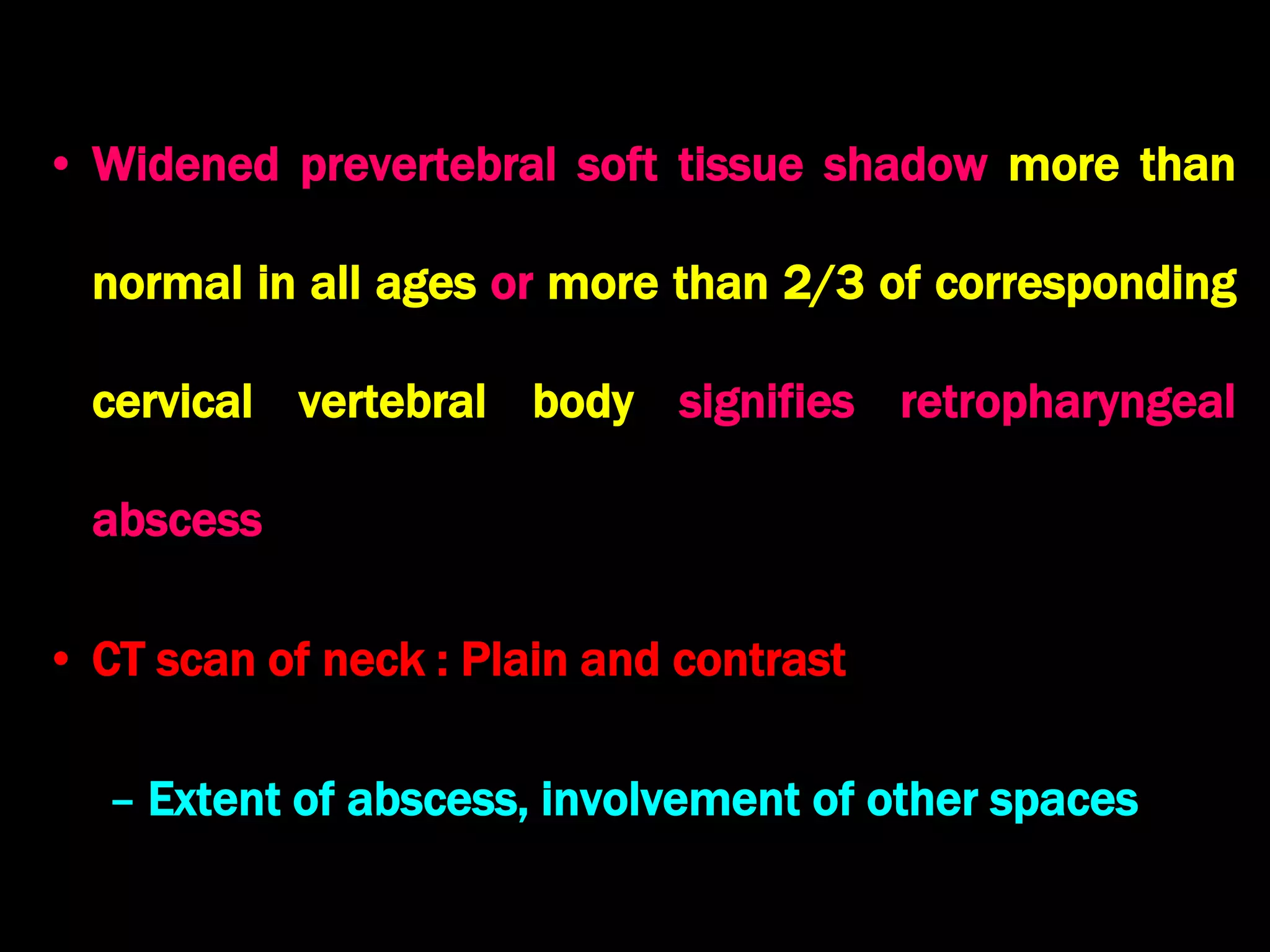
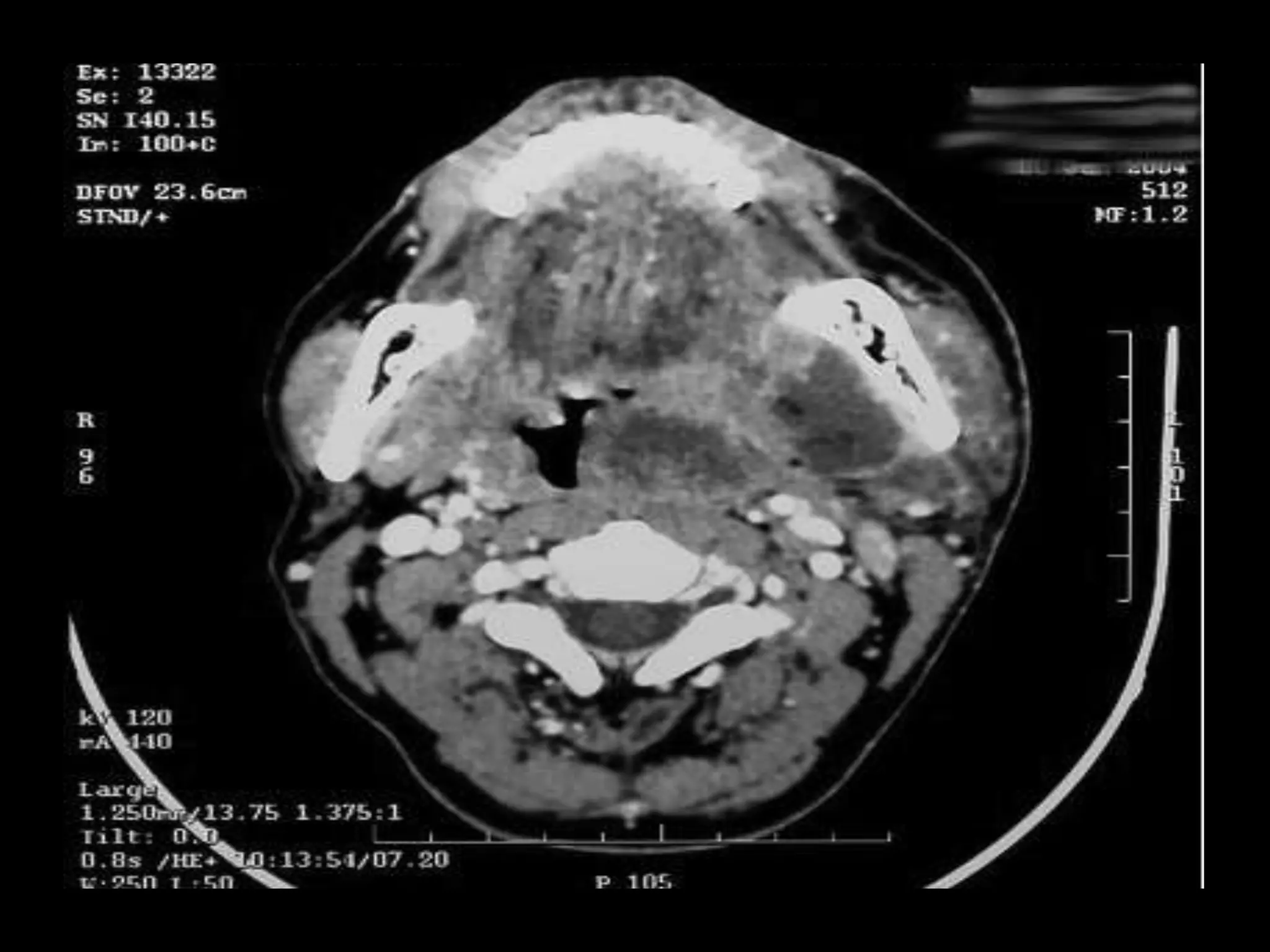
This document discusses several deep neck space infections including Ludwig's angina, retropharyngeal abscess, and parapharyngeal abscess. Ludwig's angina is a rapidly progressing cellulitis of the submandibular space that can compromise the airway. Retropharyngeal abscess is a collection of pus in the retropharyngeal space, often caused by upper respiratory infections in children, and treated with antibiotics and incision and drainage. Parapharyngeal abscess has multiple potential causes and requires systemic antibiotics as well as intraoral or external incision and drainage.