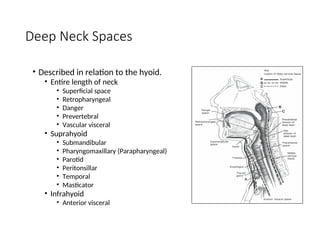
The document extensively discusses deep neck space infections, covering anatomical aspects of cervical fascia, the classification of deep neck spaces, common pathogens, clinical features, and management strategies. It details specific infections such as peritonsillar abscess, parapharyngeal abscess, and Ludwig's angina, outlining their causes, symptoms, and treatment approaches. Additionally, it highlights the importance of imaging studies for diagnosis and therapeutic interventions, including both medical and surgical treatments.