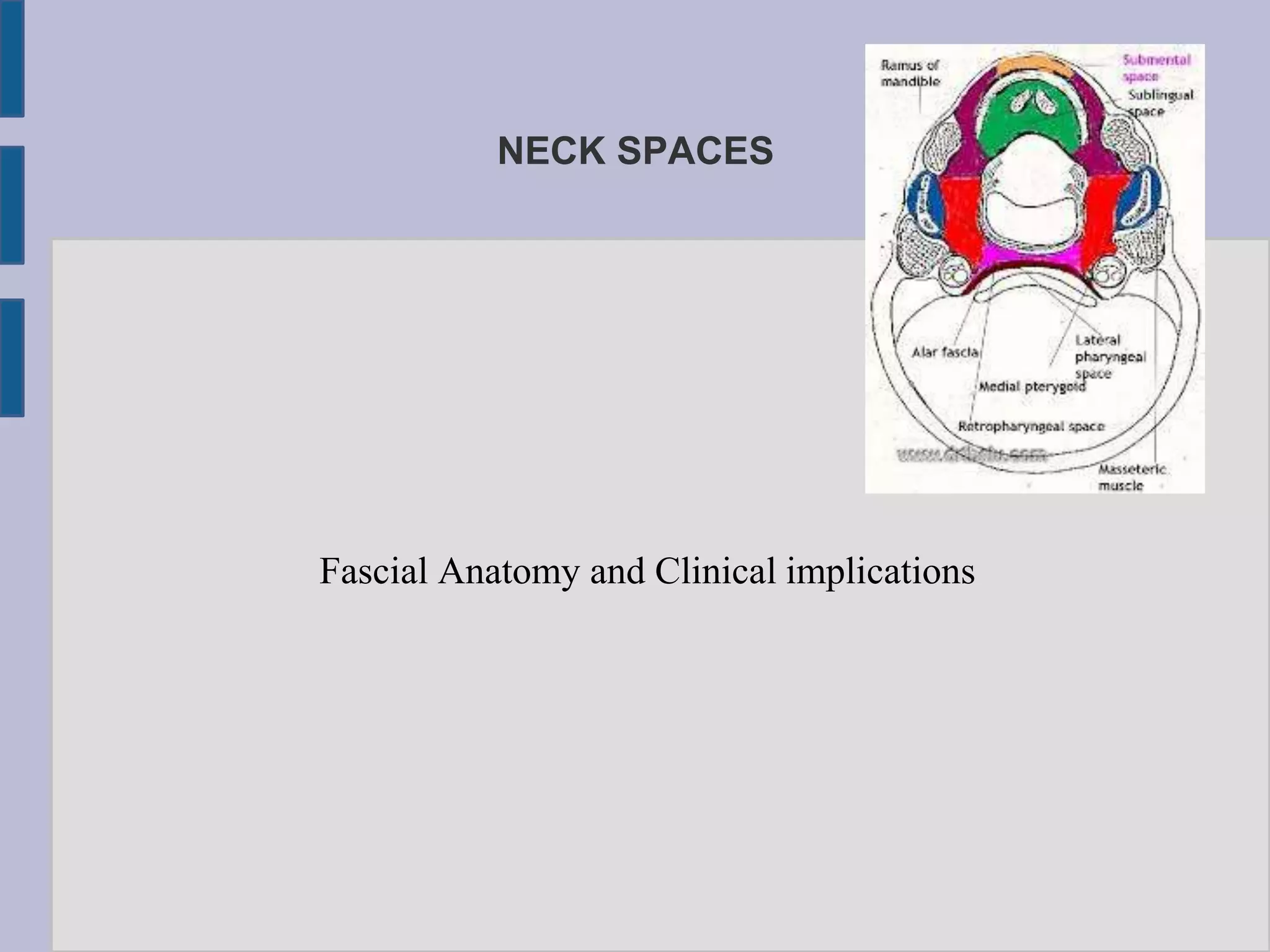
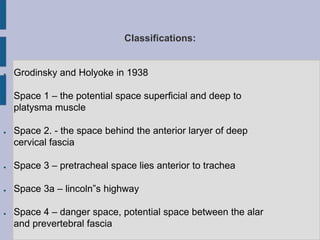
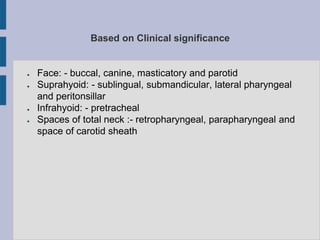
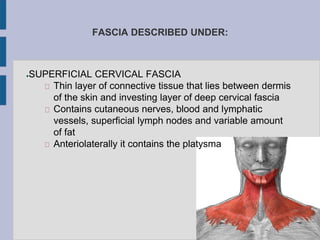
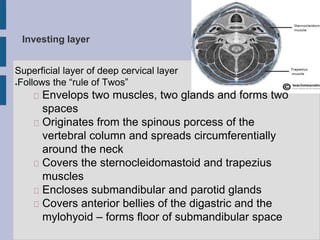
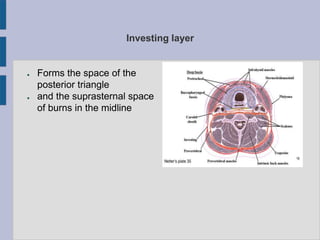
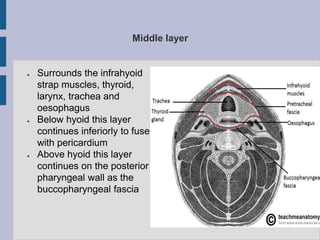
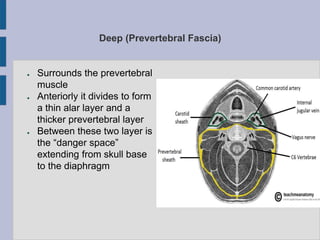
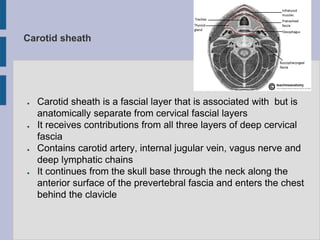
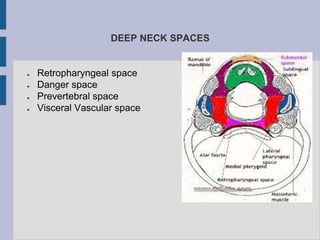
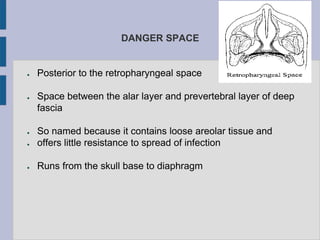
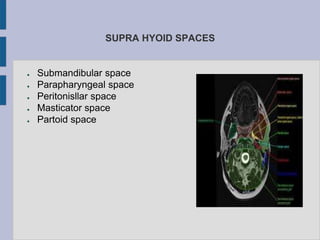
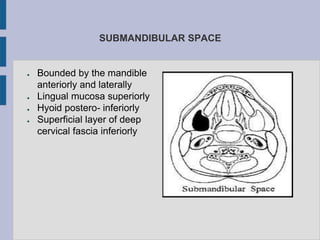
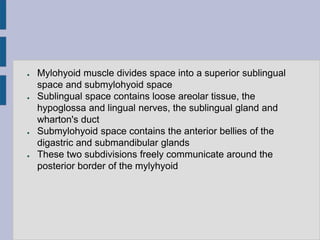
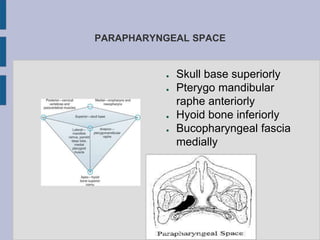
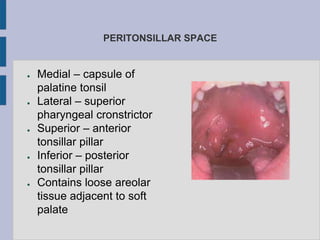
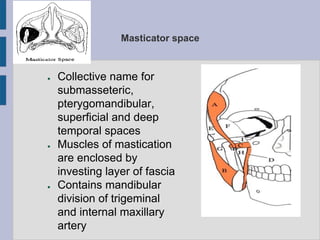
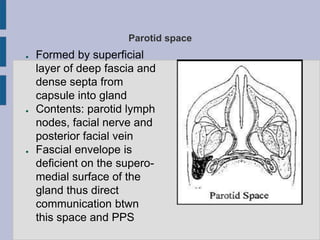
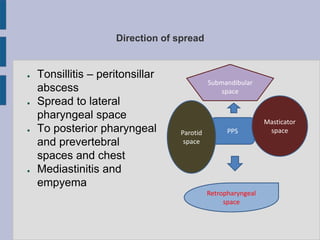
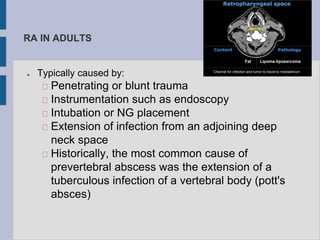
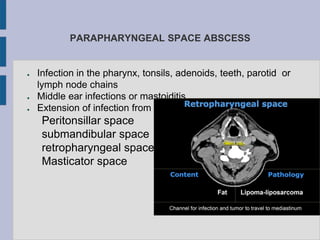
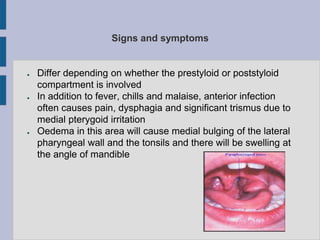
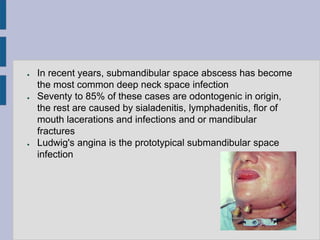
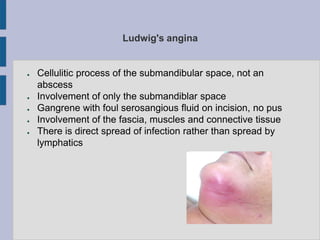
The document discusses the fascial anatomy and clinical implications of infections in the orofacial region, detailing how infections spread through potential spaces around the head and neck. It classifies various fascial spaces, describes their anatomical relationships, and outlines management principles for deep neck infections, emphasizing the importance of early recognition and appropriate therapy. The document highlights the significance of understanding facial anatomy to effectively predict infection spread and facilitate adequate drainage.