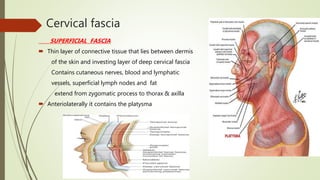
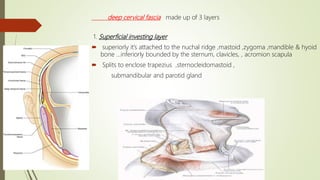
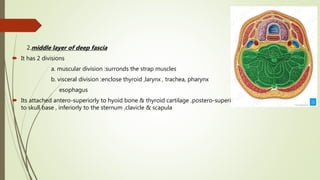
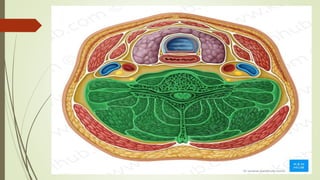
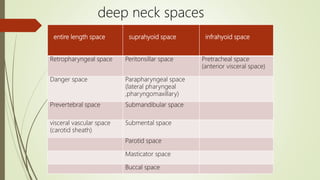
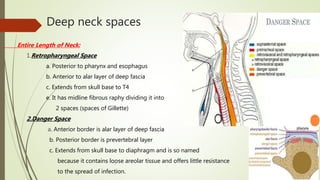
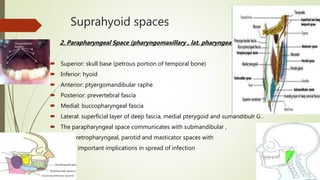
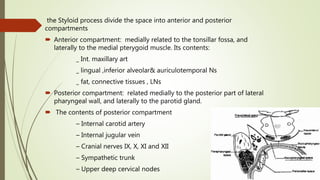
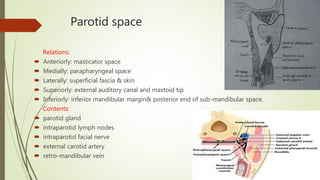
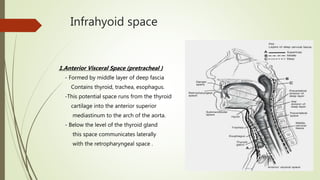
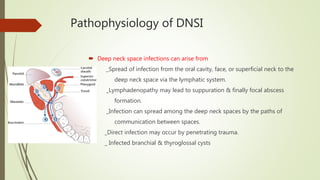
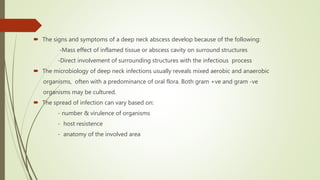
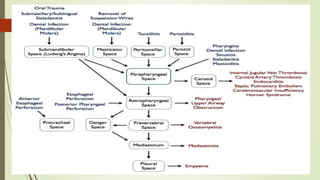
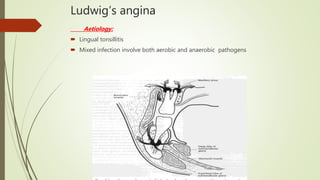
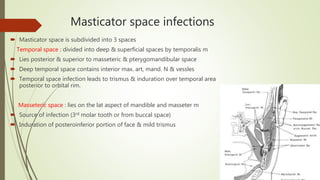
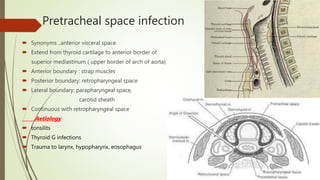
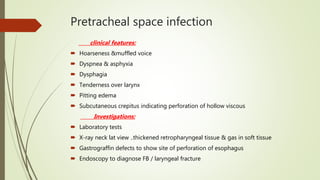
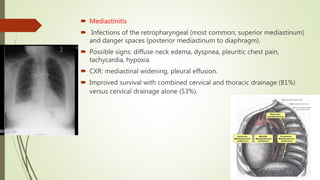
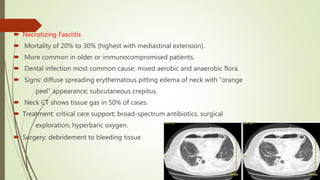
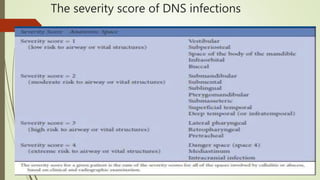
This document discusses deep neck space infections, including anatomy of the cervical fascia and deep neck spaces. It covers the pathophysiology, clinical evaluation, and treatment of deep neck space infections. The key points are:
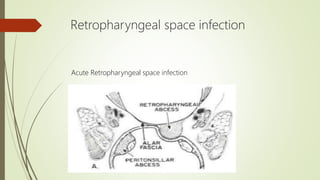
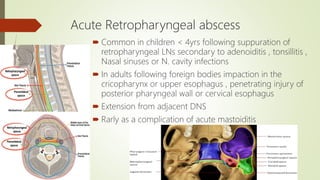
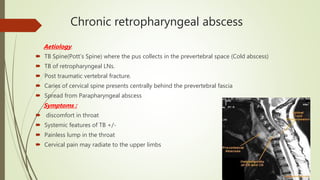
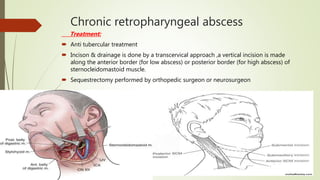
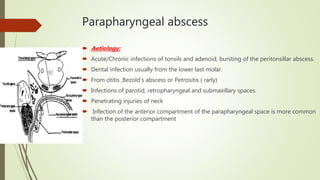
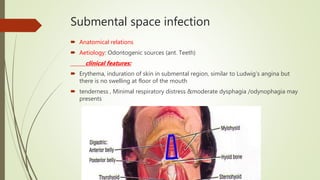
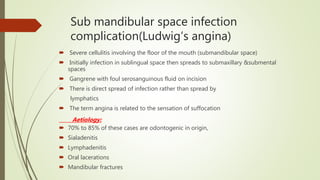
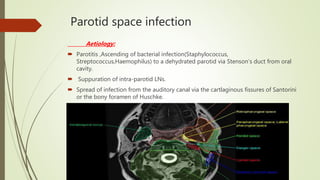
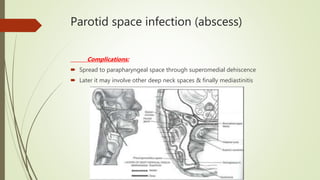
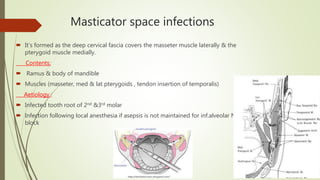
1. Deep neck space infections can arise from spread of infection from oral cavity/face or lymphadenopathy and spread between neck spaces along paths of communication.
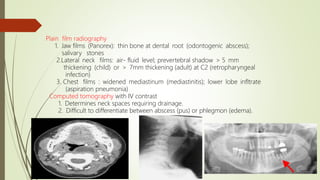
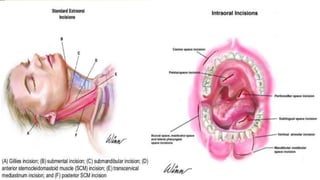
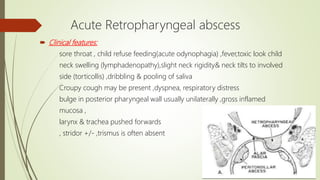
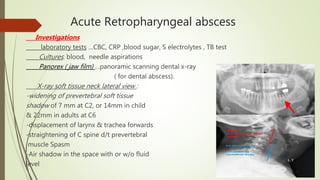
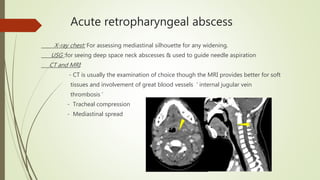
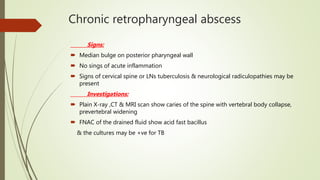
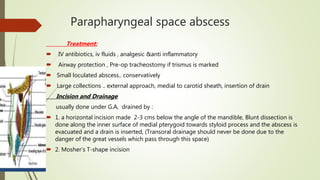
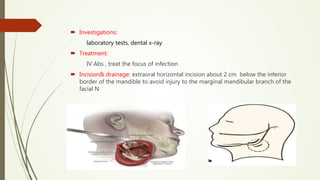
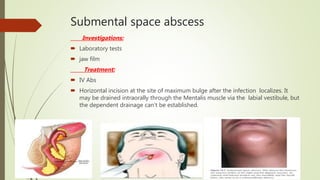
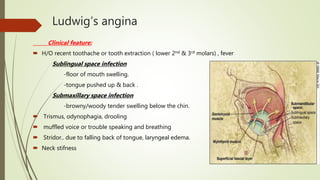
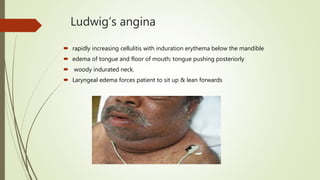
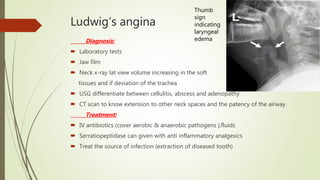
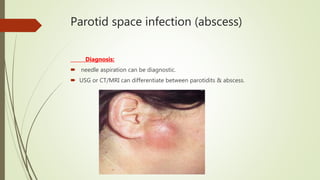
2. Clinical evaluation includes history, physical exam focusing on localizing signs, and imaging studies like CT to determine involved spaces requiring drainage.
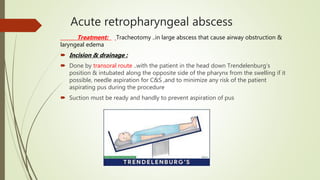
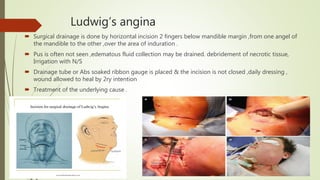
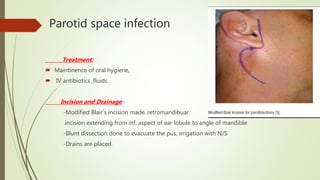
3. Treatment priorities are airway management to prevent mortality and drainage of involved spaces to prevent spread of infection.