This document provides an overview of upper gastrointestinal bleeding, including:
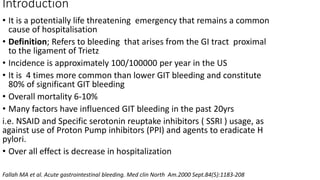
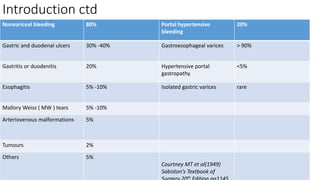
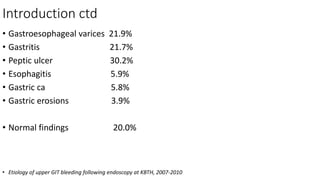
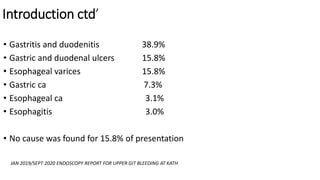
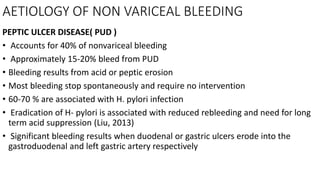
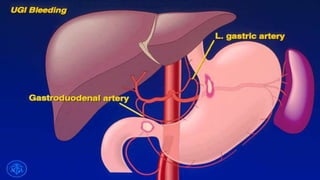
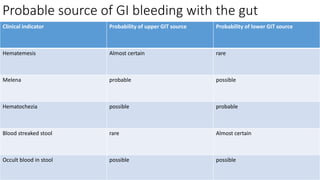
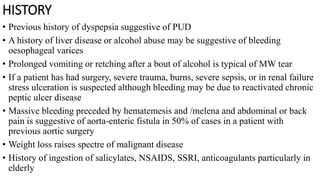
- The definition, incidence, mortality, and common causes of upper GI bleeding. The most common causes are gastric and duodenal ulcers, esophagitis, and esophageal varices.
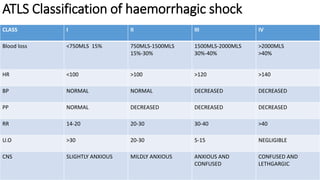
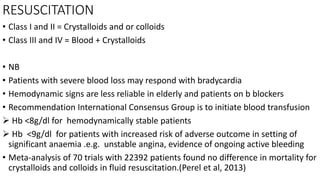
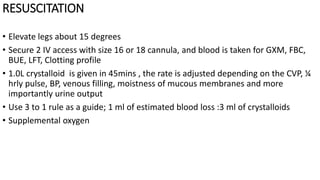
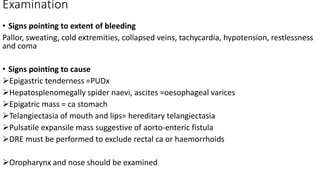
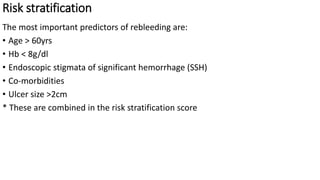
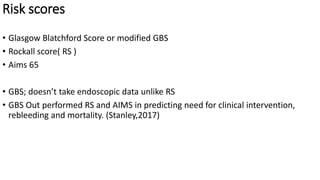
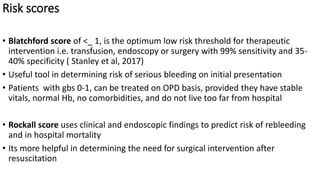
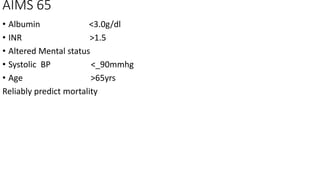
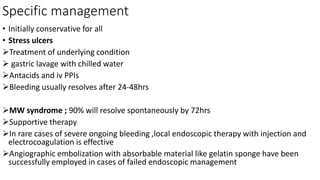
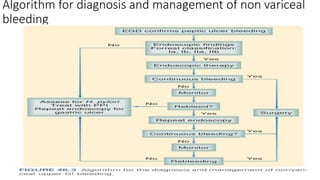
- Principles of management including initial assessment, resuscitation, localization of bleeding site usually through endoscopy, and risk stratification to determine need for inpatient care or intervention.
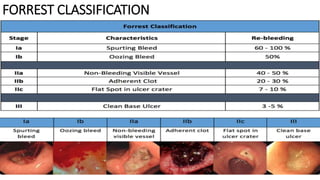
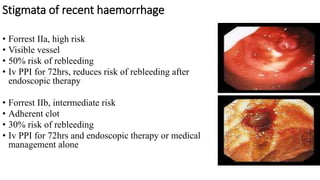
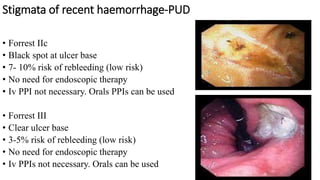
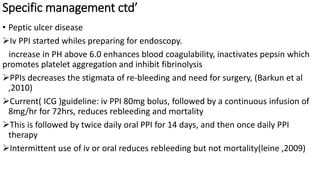
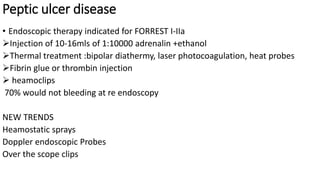
- Endoscopy is the gold standard for diagnosis and treatment. The Forrest classification guides prognosis and need for endoscopic therapy based on stigmata of recent hemorrhage seen. Proton pump inhibitors are commonly used for prevention of rebleeding.