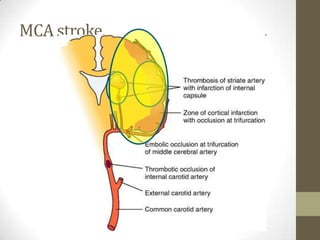
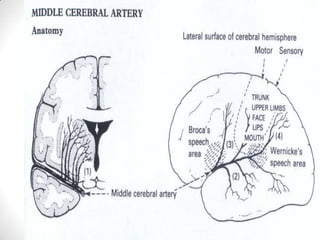
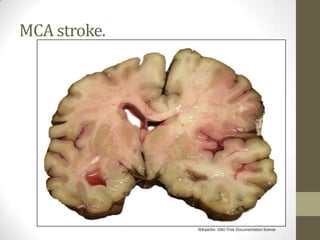
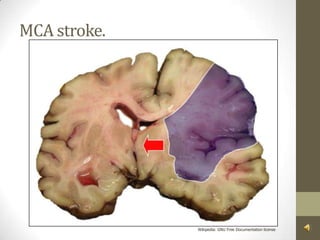
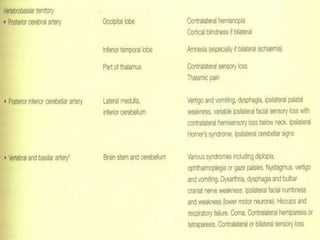
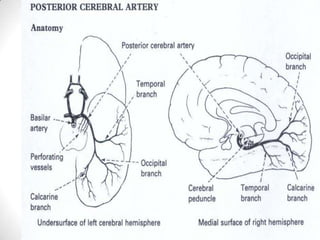
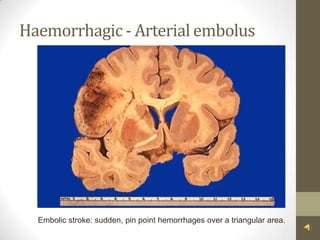
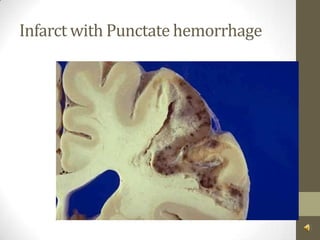
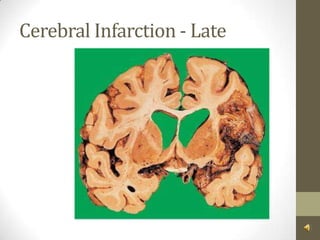
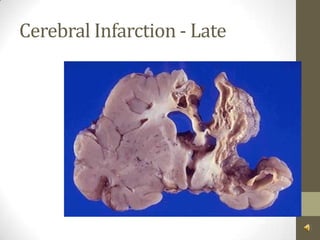
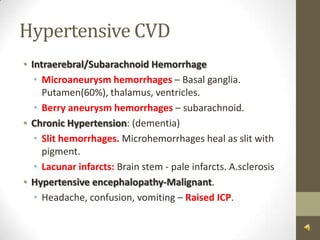
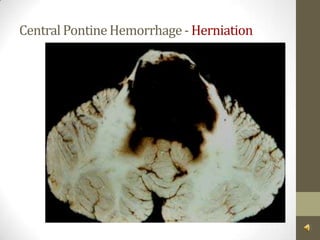
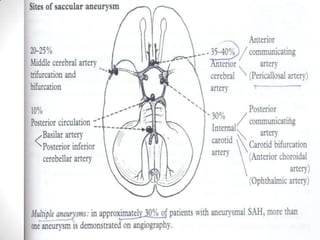
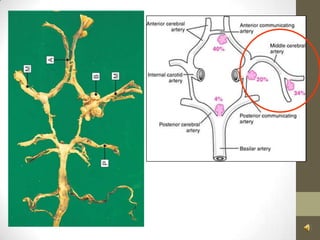
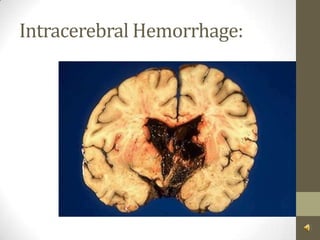
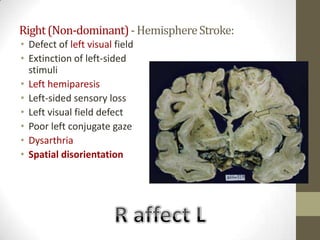
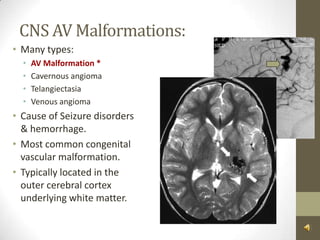
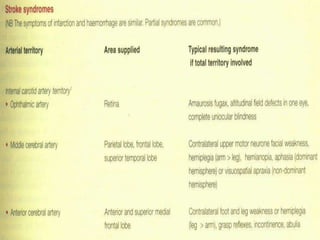
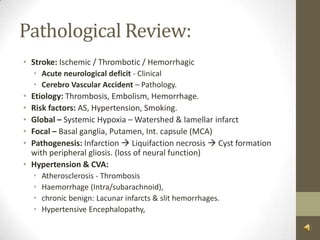
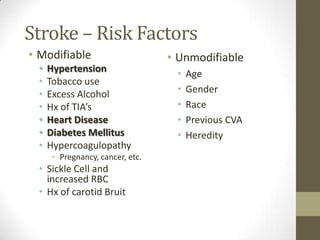
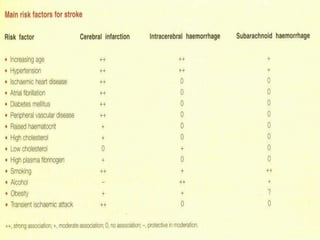
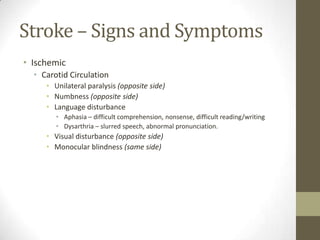
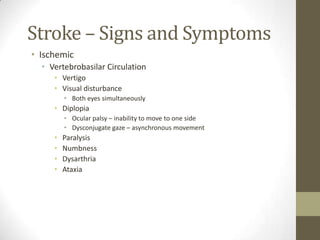
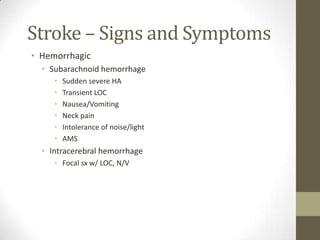
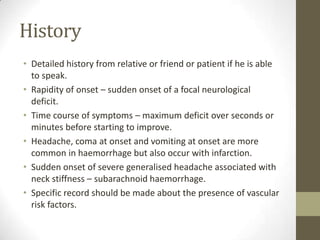
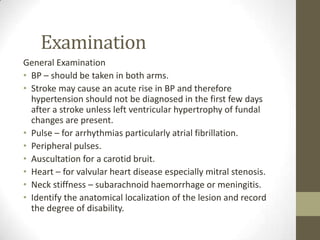
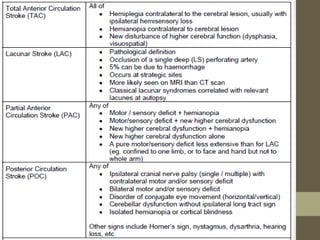
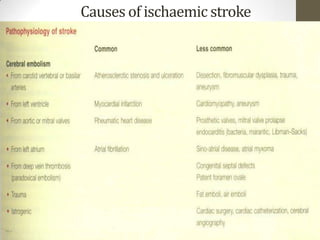
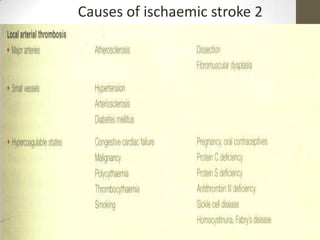
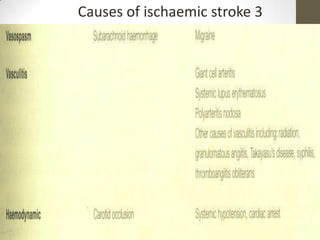
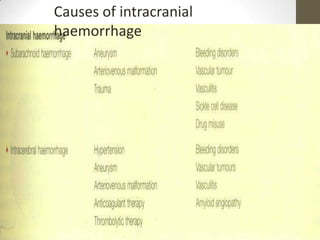
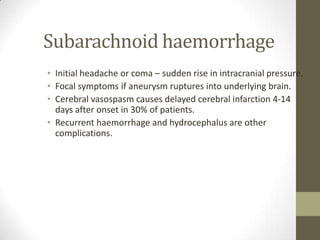
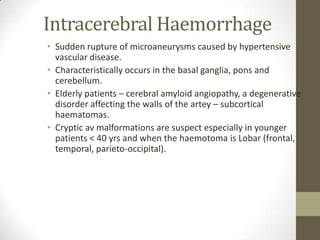
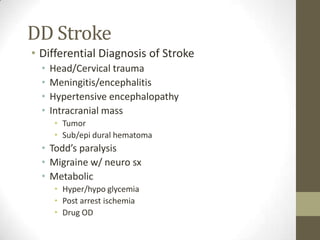
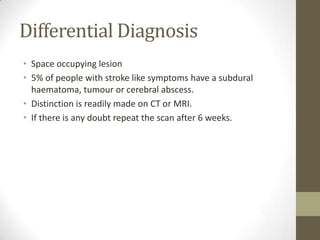
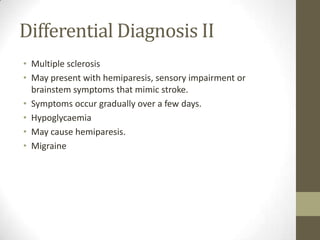
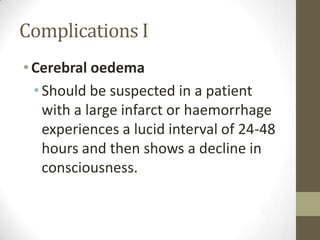
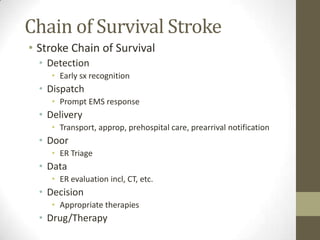
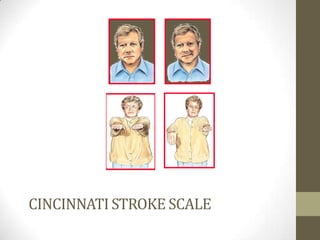
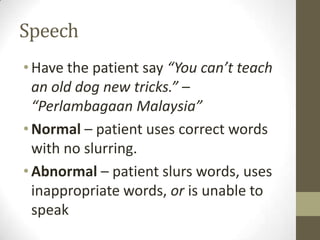
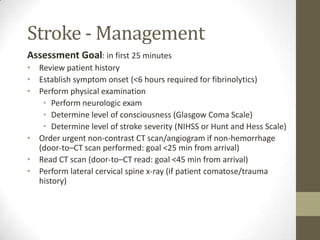
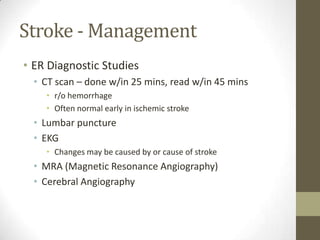
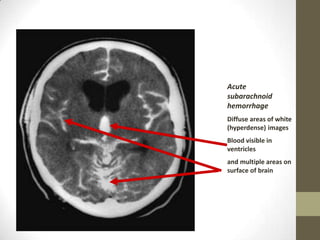
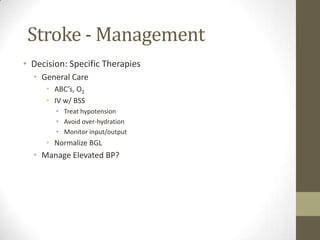
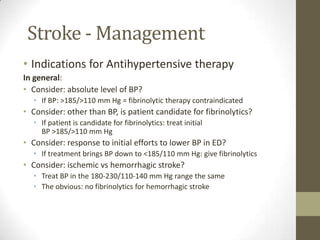
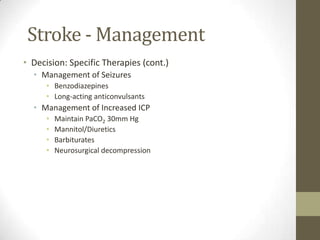
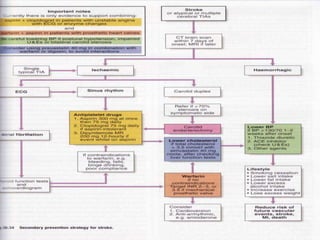
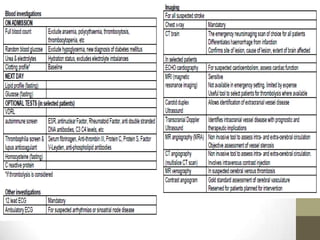
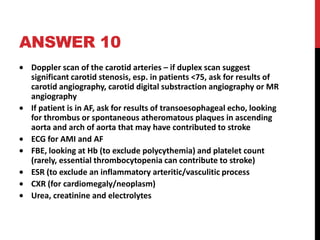
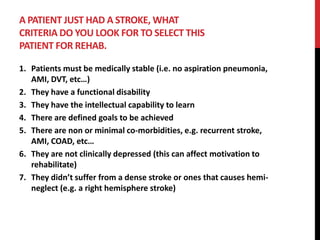
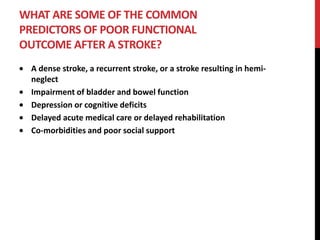
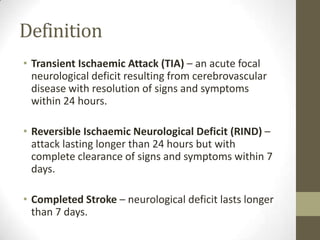
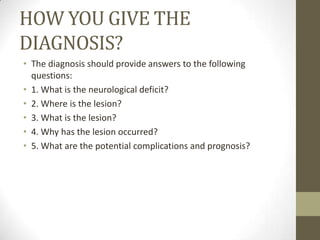
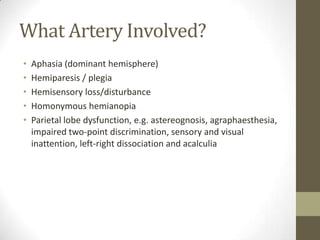
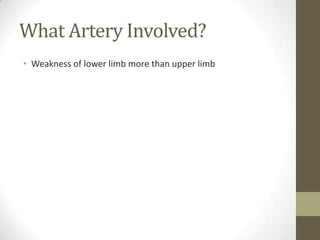
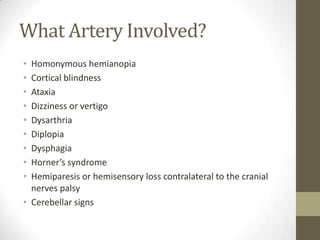
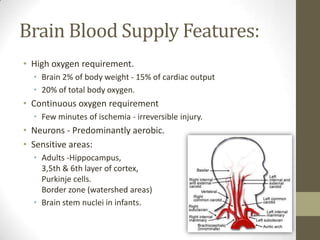
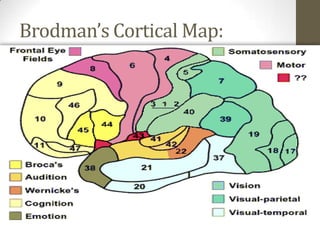
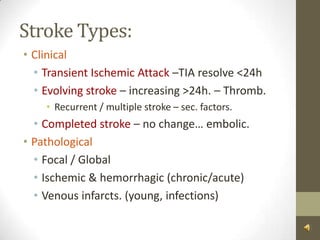
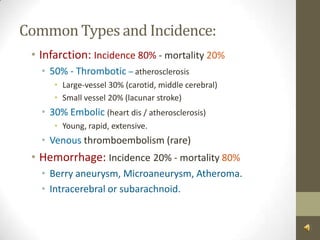
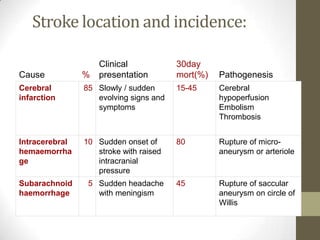
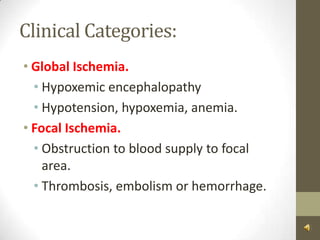
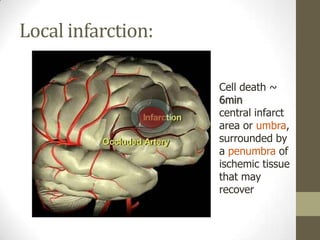
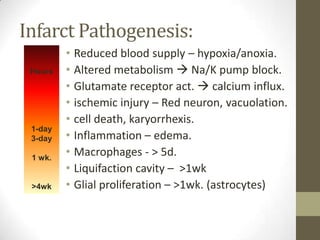
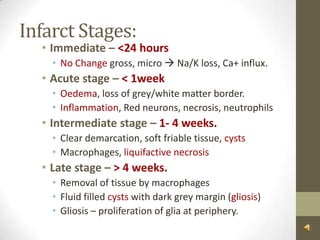
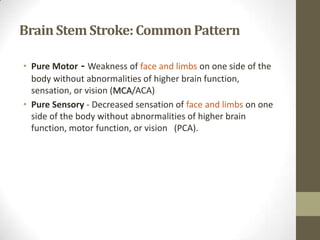
The document provides information about strokes and cerebrovascular accidents. It defines different types of strokes including transient ischemic attack (TIA), reversible ischemic neurological deficit (RIND), and completed stroke. It discusses how to diagnose strokes by determining the neurological deficit, lesion location, type of lesion, and cause. The document also covers stroke risk factors, common locations for strokes including the middle cerebral artery (MCA), anatomy of the brain and blood supply, and types of strokes such as infarction and hemorrhage.
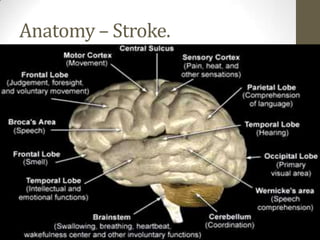
![Frontal[f*ck – motor] Lobe Functions:High level cognitive functions. i.e reasoning, abstraction, concentrationStorage of information – memoryControl of voluntary eye movementMotor control of speech in the dominant hemisphere.Motor Cortex – Motor control of the contralateral side of the bodyUrinary continenceEmotion and personality](https://image.slidesharecdn.com/strokeandcerebrovascularaccident-110401042134-phpapp01/85/Stroke-and-cerebrovascular-accident-11-320.jpg)
![Parietal[p-sx – sensory] Lobe Functions:Sensory cortex – sensory input is interpreted to define size, weight, texture and consistency (contralateral)Sensation is localised, and modalities of touch, pressure and position are identified.Awareness of the parts of bodyNon-dominant – processes visuospatial information andcontrols spatial orientationDominant is involved in ideomotor praxis (ability to perform learned motor tasks](https://image.slidesharecdn.com/strokeandcerebrovascularaccident-110401042134-phpapp01/85/Stroke-and-cerebrovascular-accident-12-320.jpg)
![Temporal[t-telinga] Lobe Functions:Primary auditory receptive areasIn dominant ability to comprehend speech (wernicke’s) – receptionInterpretive area – area at the junction of the temporal, parietal and occipital lobes.Plays an important role in visual, auditory and olfactory perceptionImportant role in learning; memory and emotional affect.](https://image.slidesharecdn.com/strokeandcerebrovascularaccident-110401042134-phpapp01/85/Stroke-and-cerebrovascular-accident-13-320.jpg)
![Occipital[O-optic] Lobe Functions:Primary visual cortexVisual association areasVisual perceptionSome visual reflexes (i.e. visual fixation)Involuntary smooth eye movement](https://image.slidesharecdn.com/strokeandcerebrovascularaccident-110401042134-phpapp01/85/Stroke-and-cerebrovascular-accident-14-320.jpg)


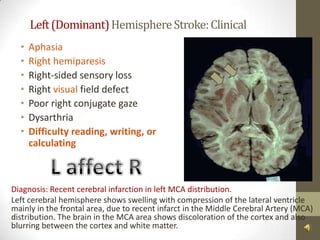
![MCA [most common] Features:Paralysis of the contralateral face, arm and legSensory impairment over the contralateral face, arm & legHomonymous hemi or quadrantonopiaParalysis of gaze to the opposite sideAphasia (dominant) and dysarthria [broca/wernicke]Penetrating - contralateral hemiplegia/paresis, slurred speech.Impaired spatial perception](https://image.slidesharecdn.com/strokeandcerebrovascularaccident-110401042134-phpapp01/85/Stroke-and-cerebrovascular-accident-34-320.jpg)