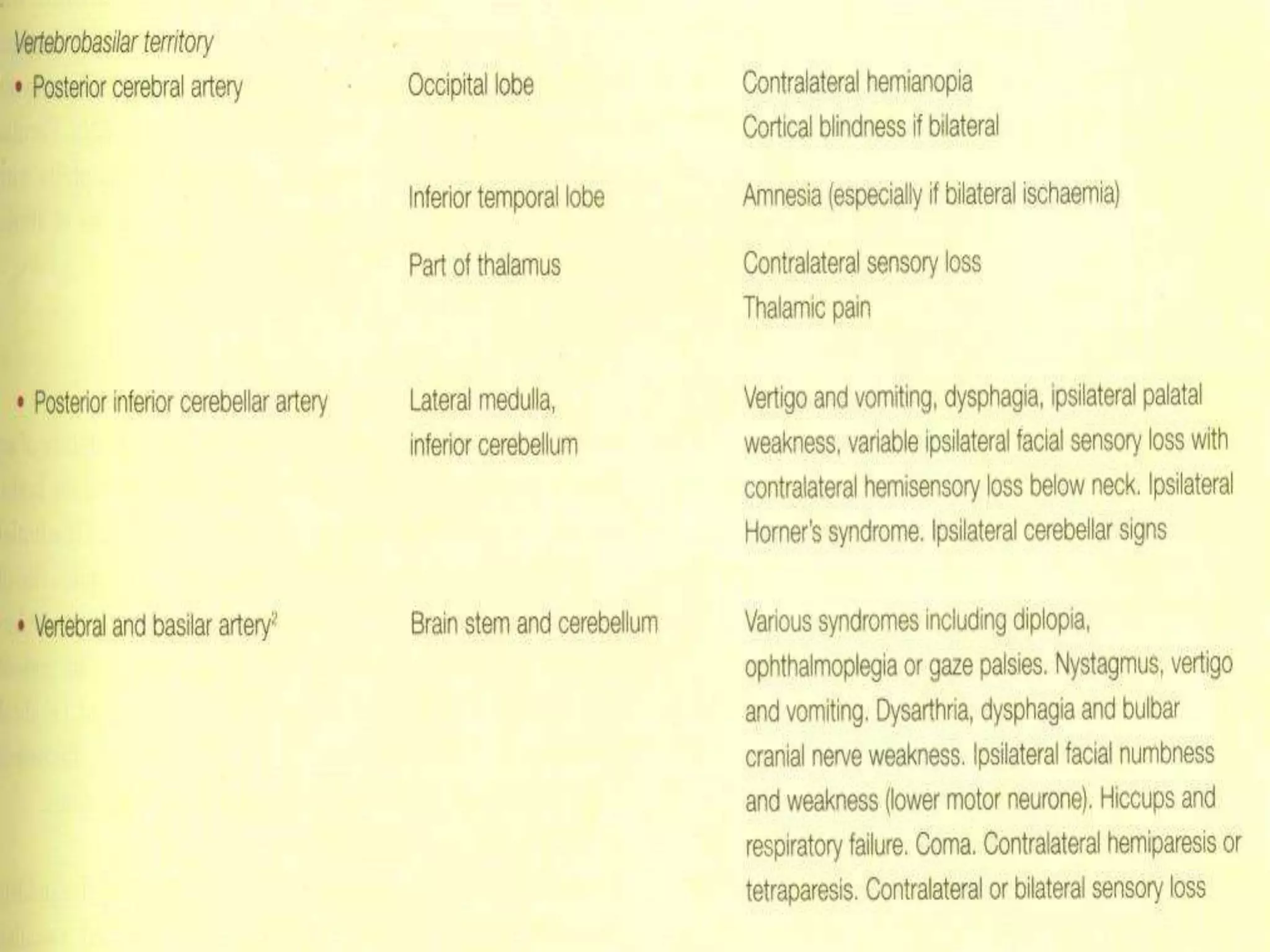
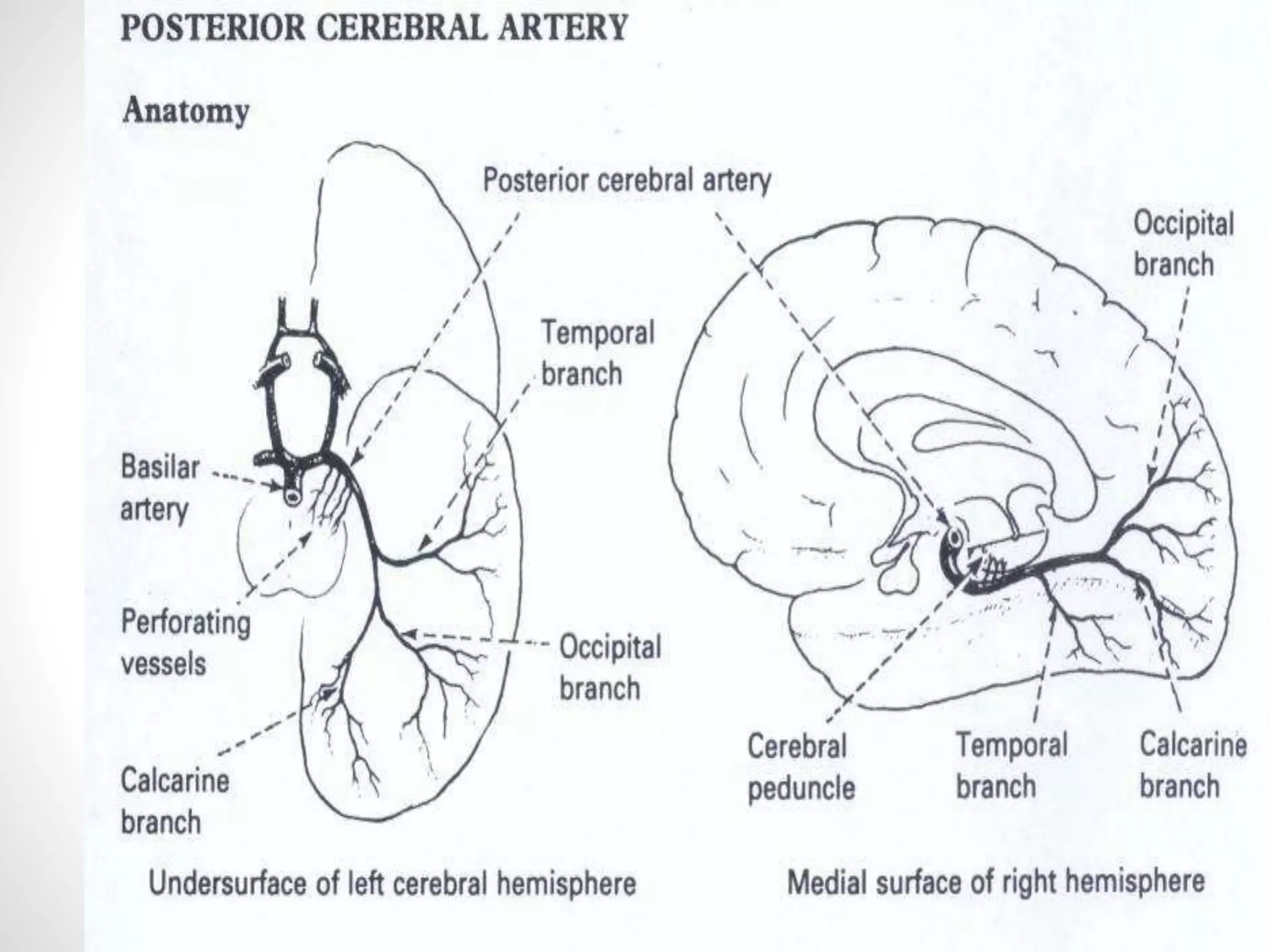
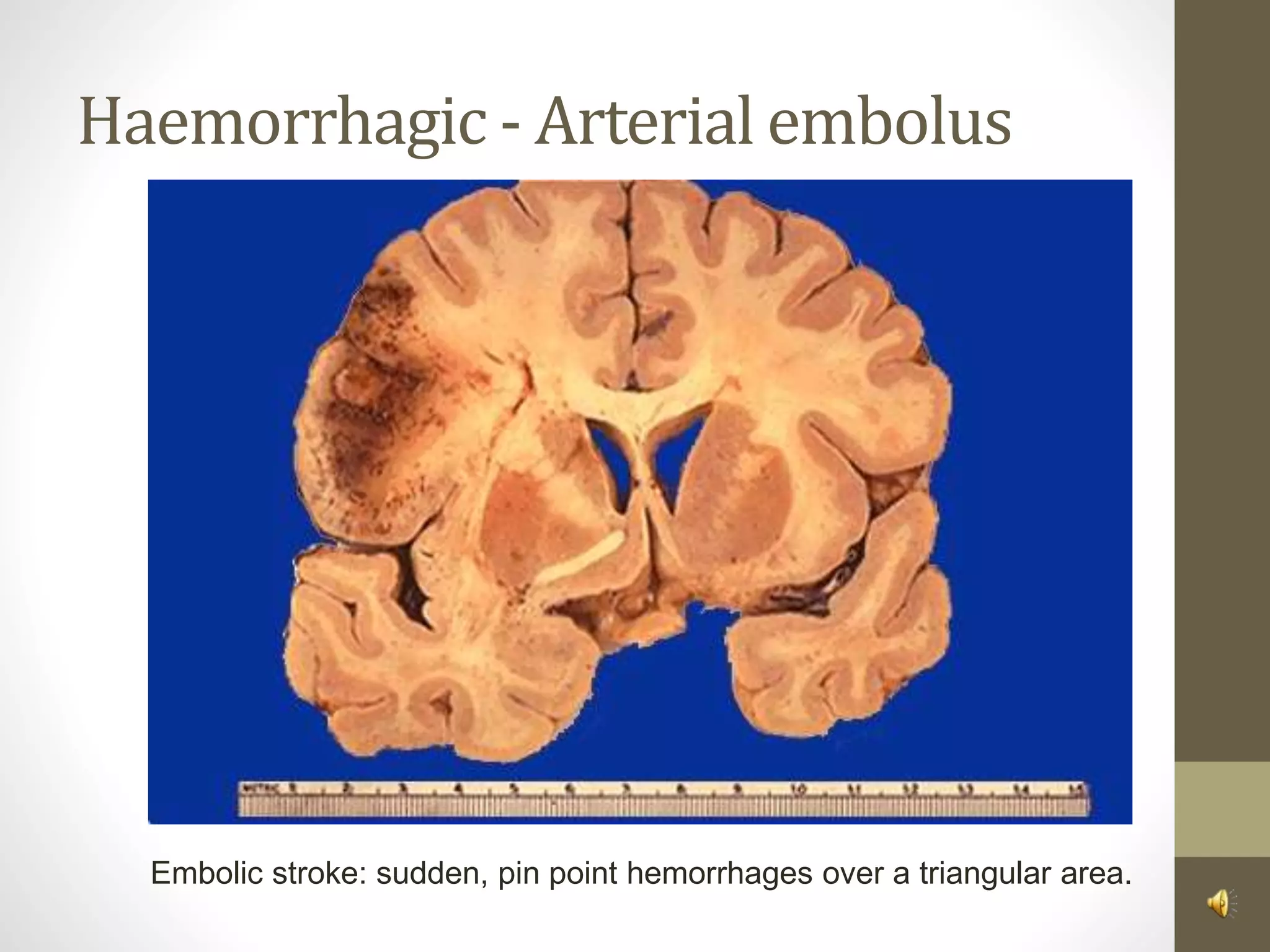
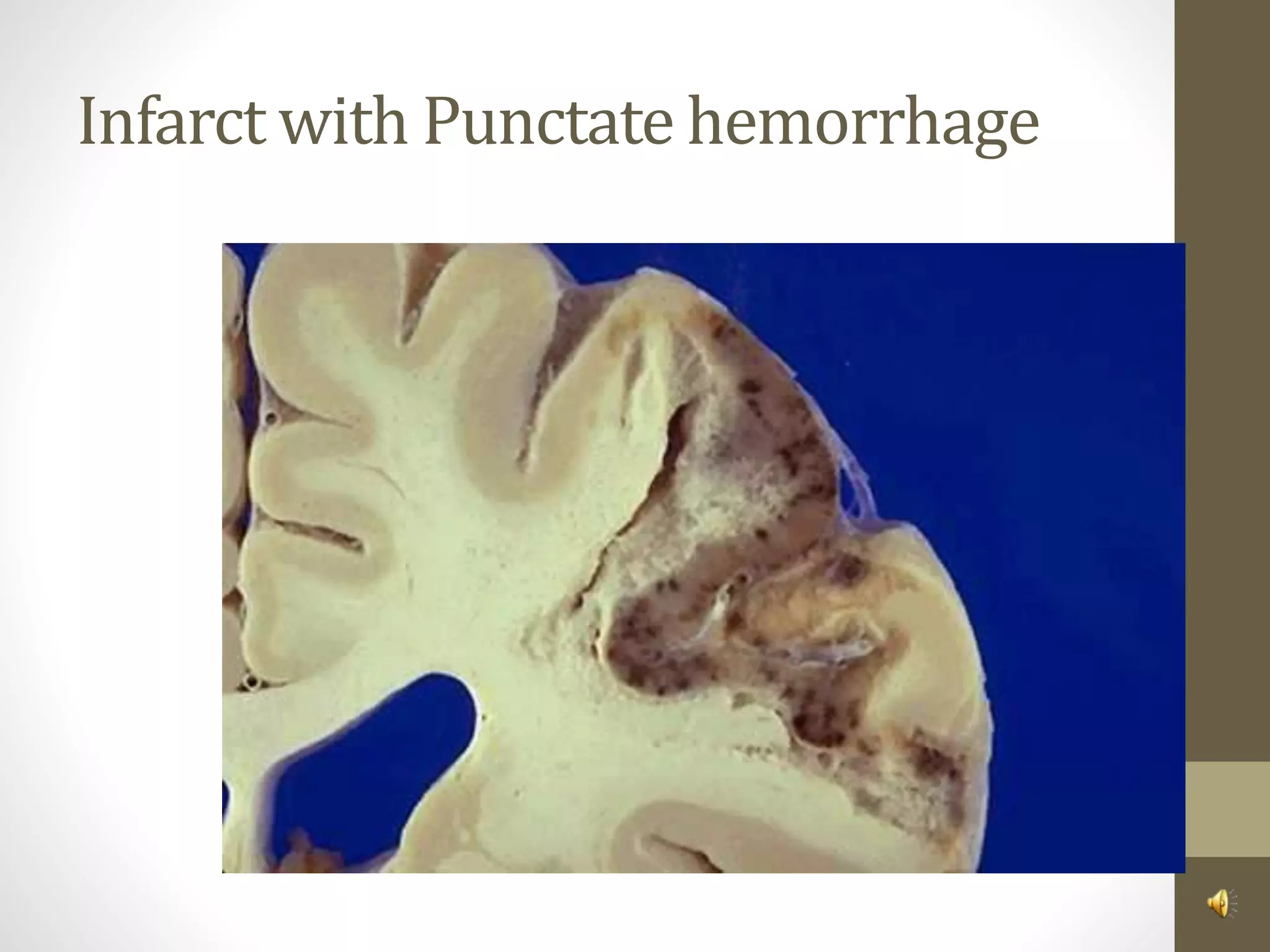
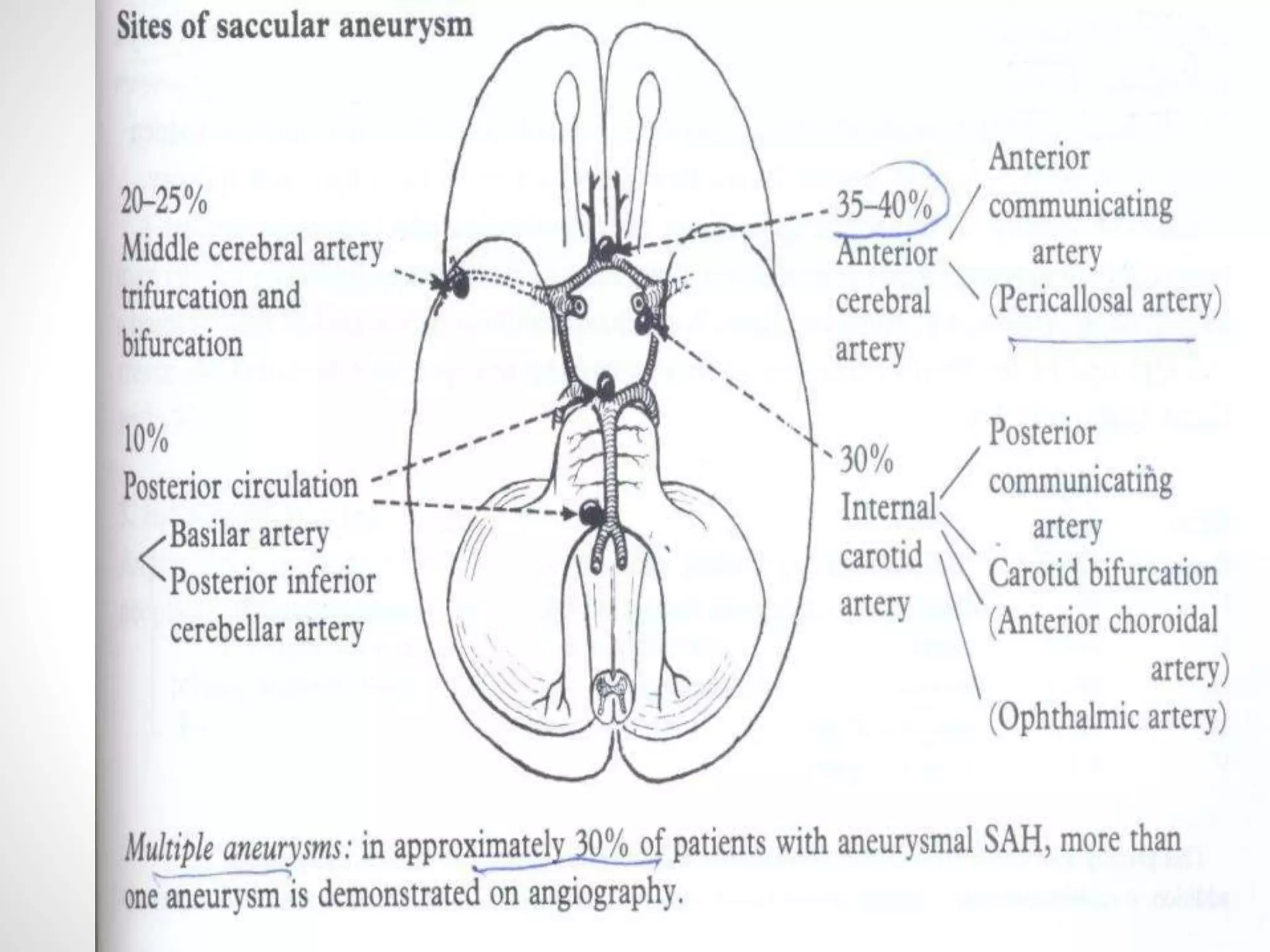
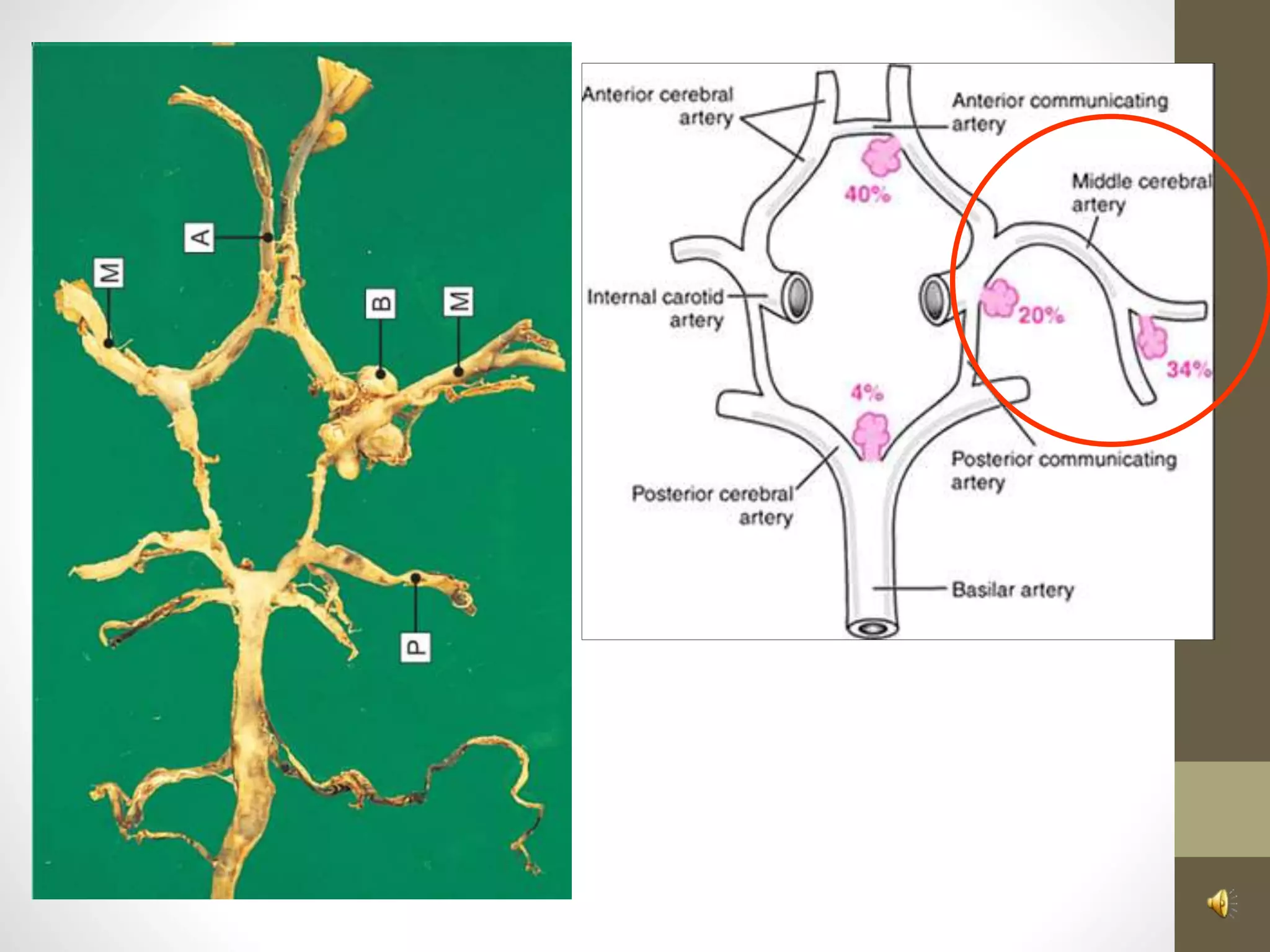
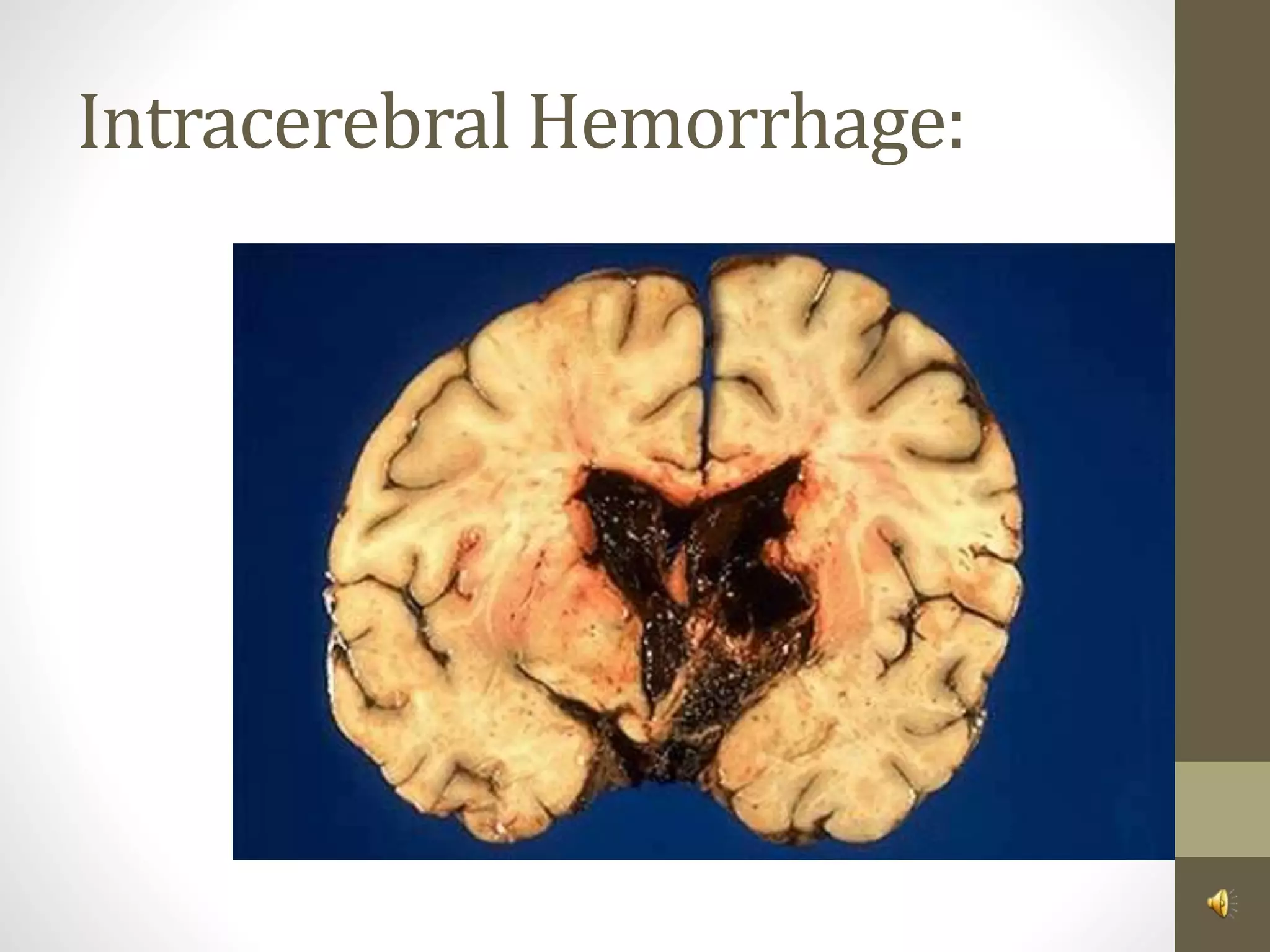
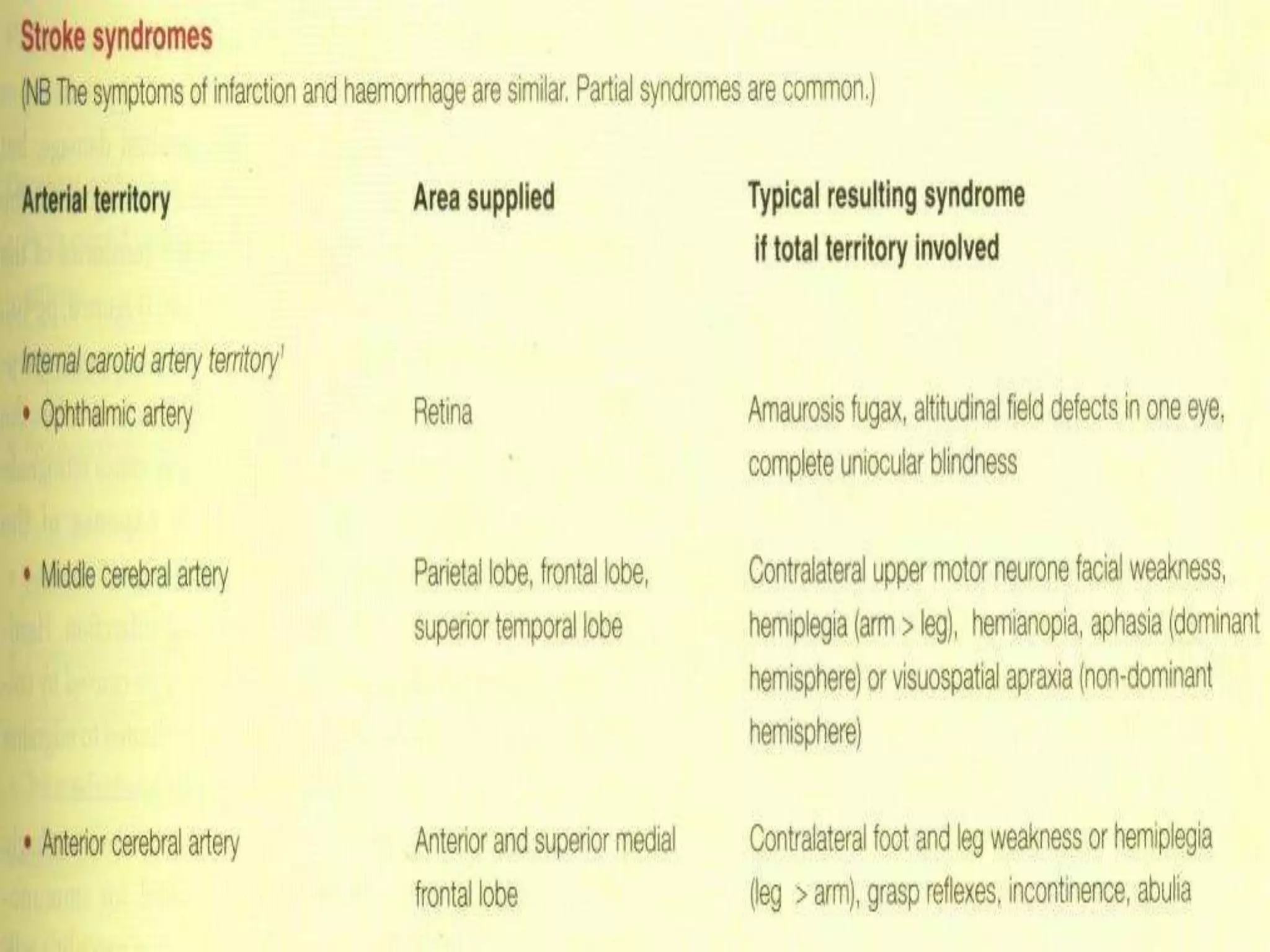
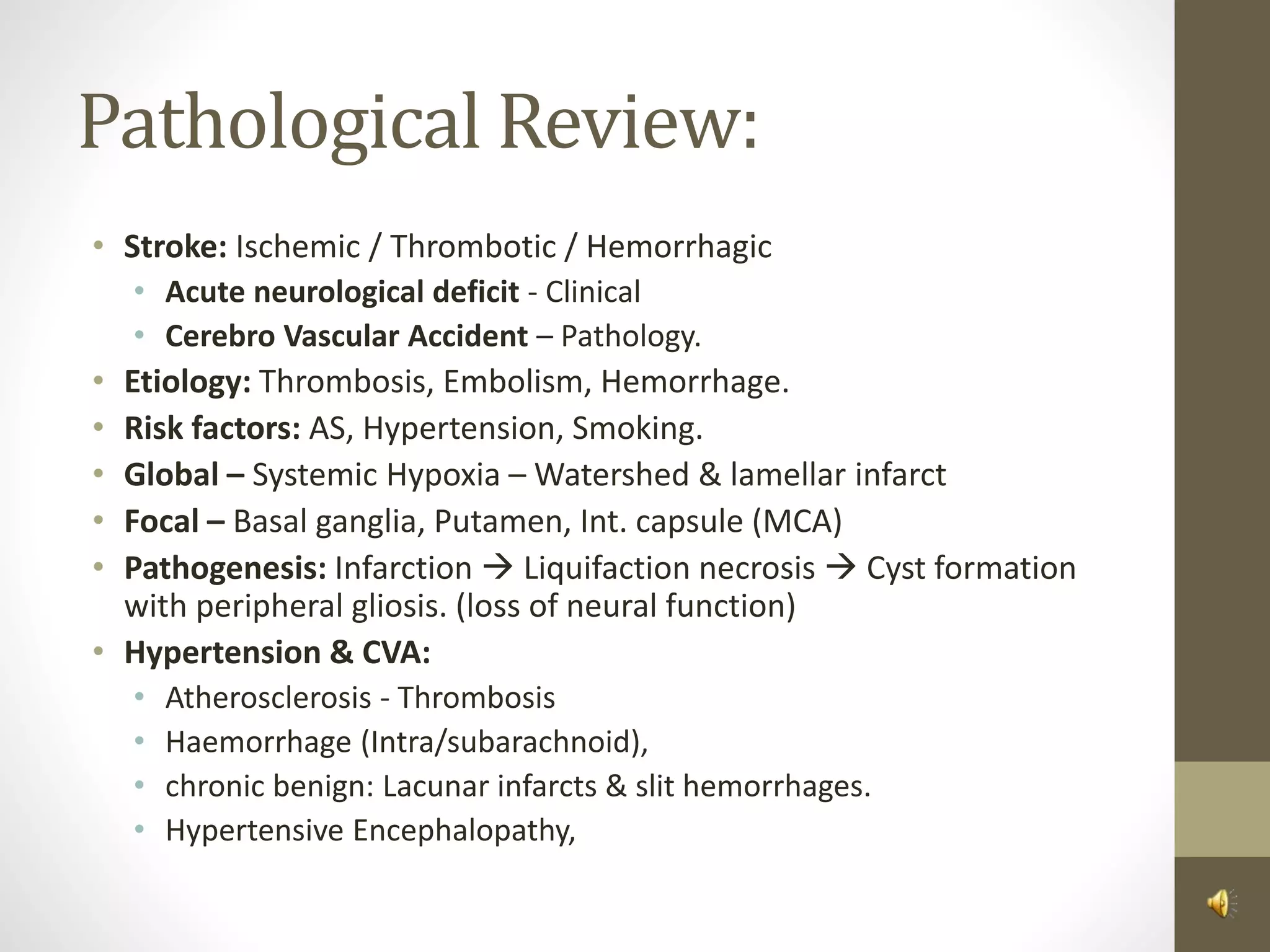
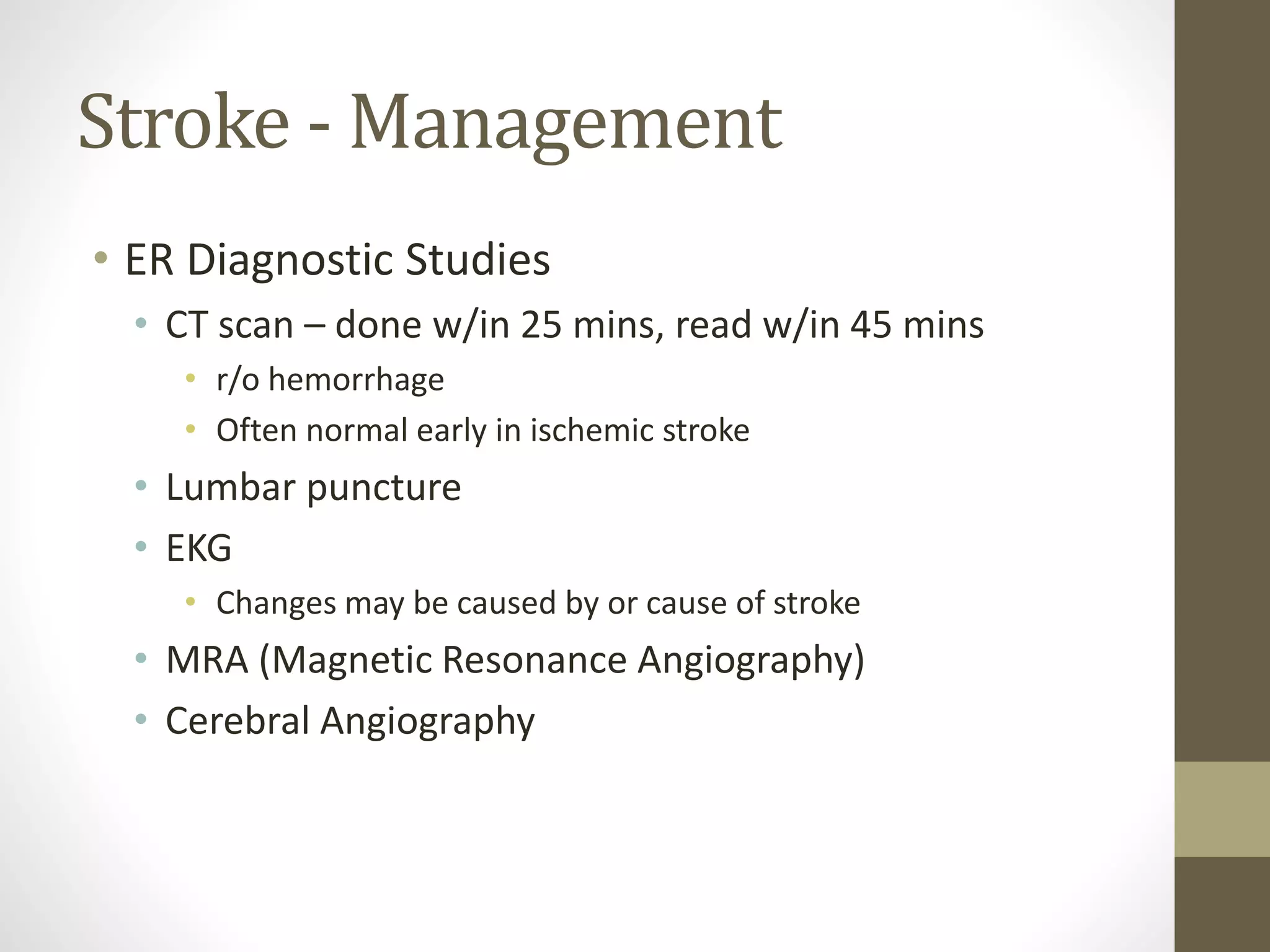
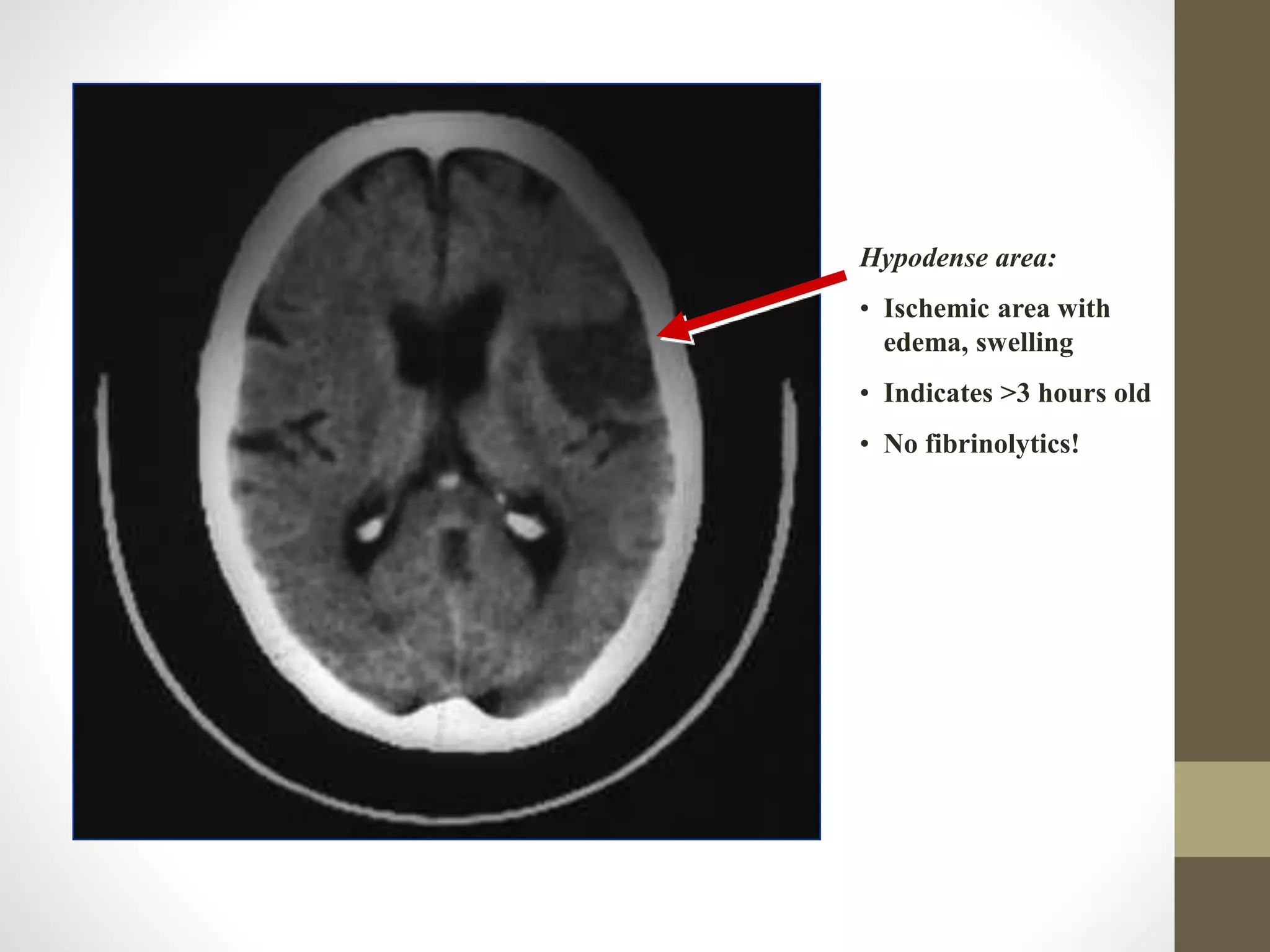
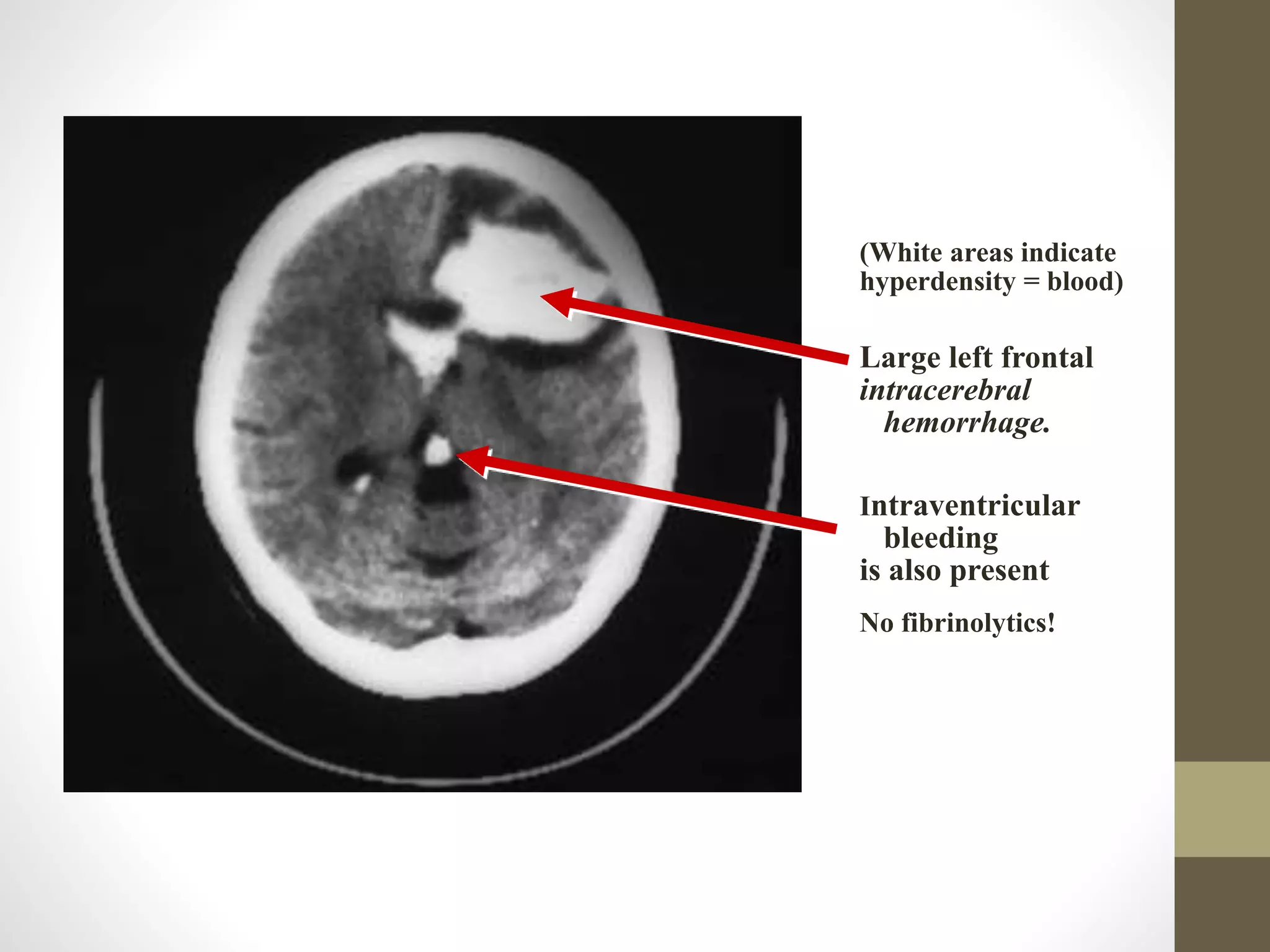
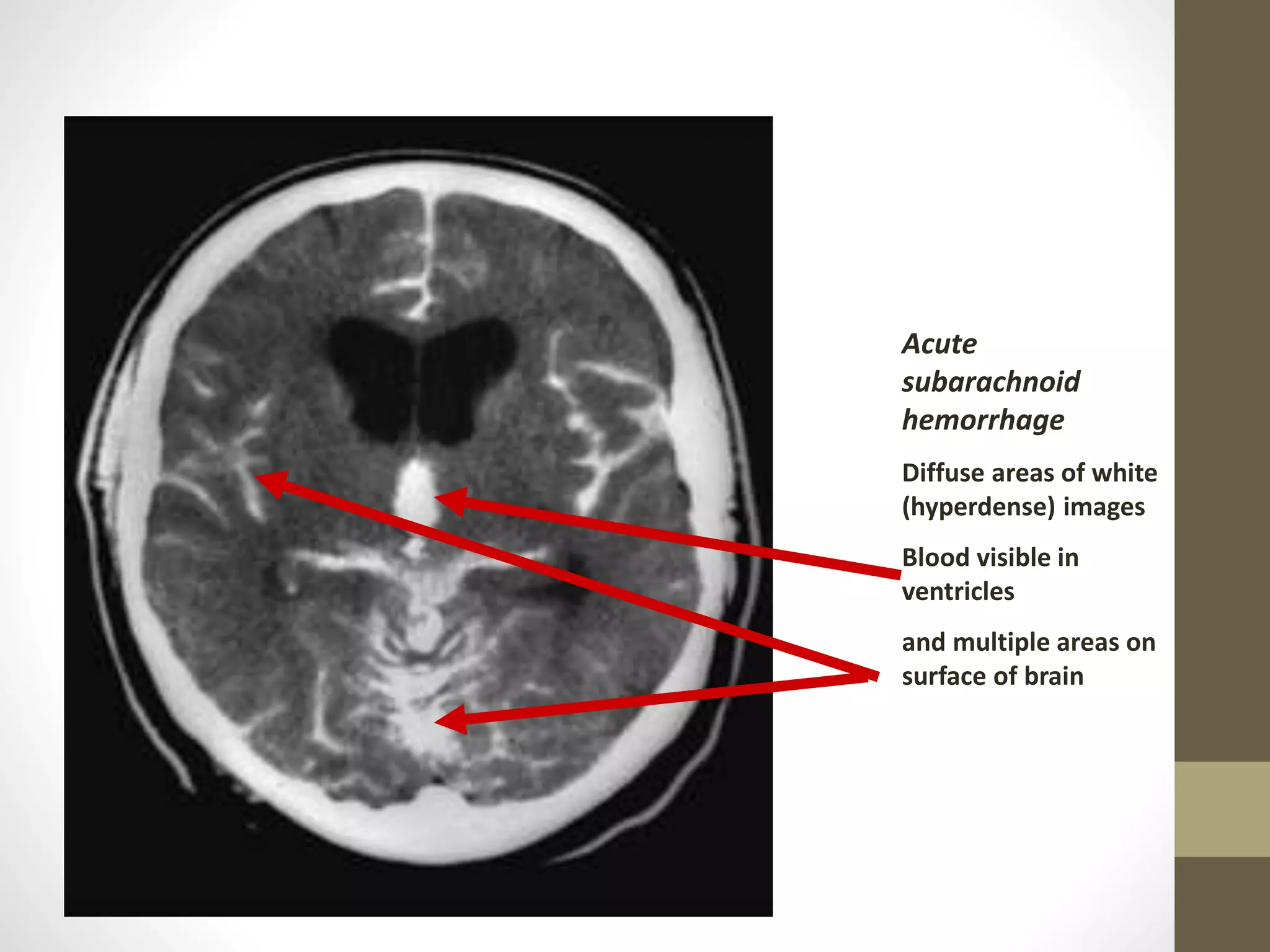
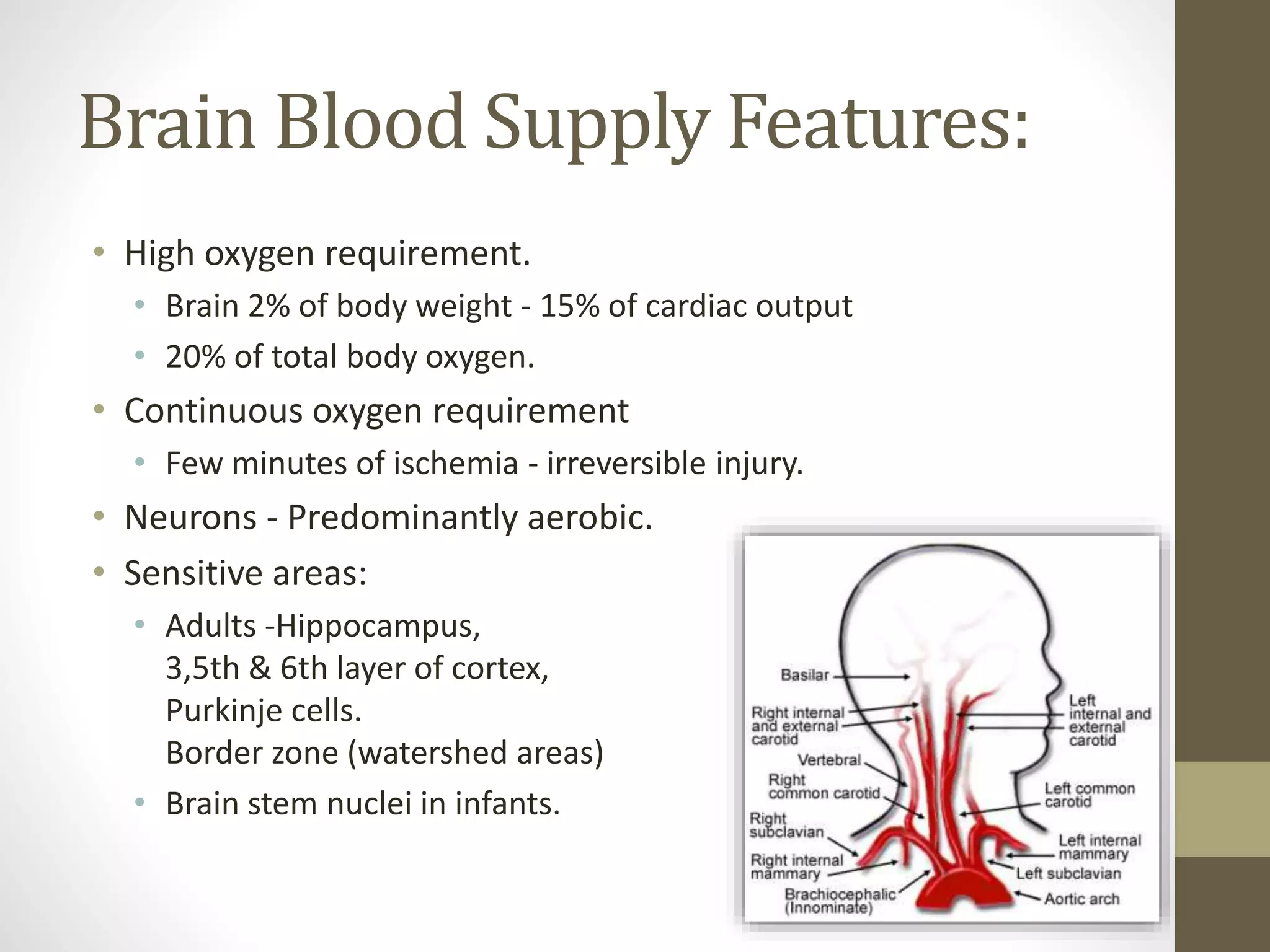
This document provides information on stroke and cerebrovascular accidents. It defines different types of strokes including transient ischemic attack (TIA), reversible ischemic neurological deficit (RIND), and completed stroke. It describes how to diagnose a stroke by determining the neurological deficit, lesion location, type of lesion, and cause. Risk factors, signs and symptoms, and methods of examination are discussed. The anatomy and blood supply of the brain are outlined. Common sites and types of infarction and hemorrhage are also summarized.
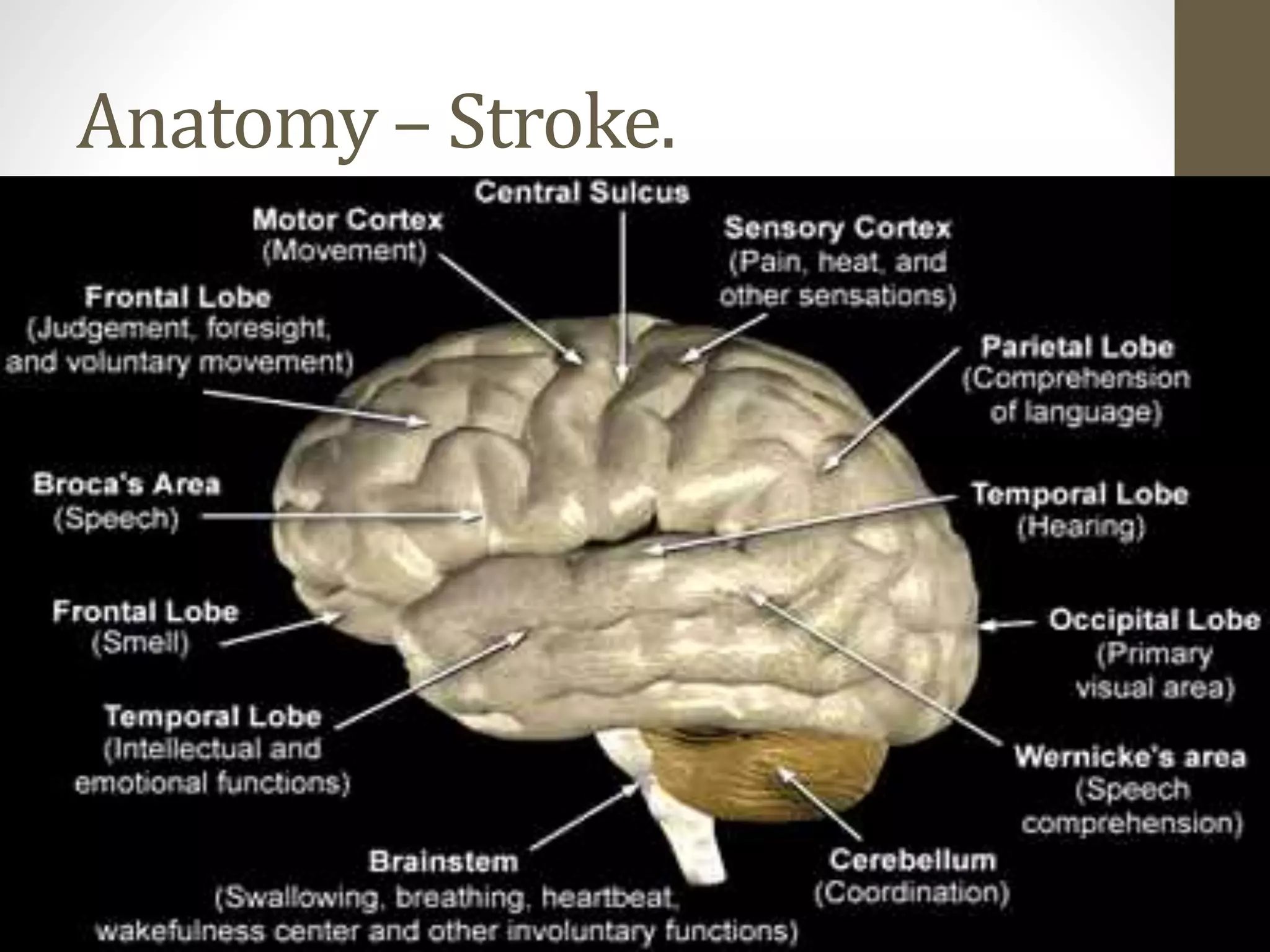
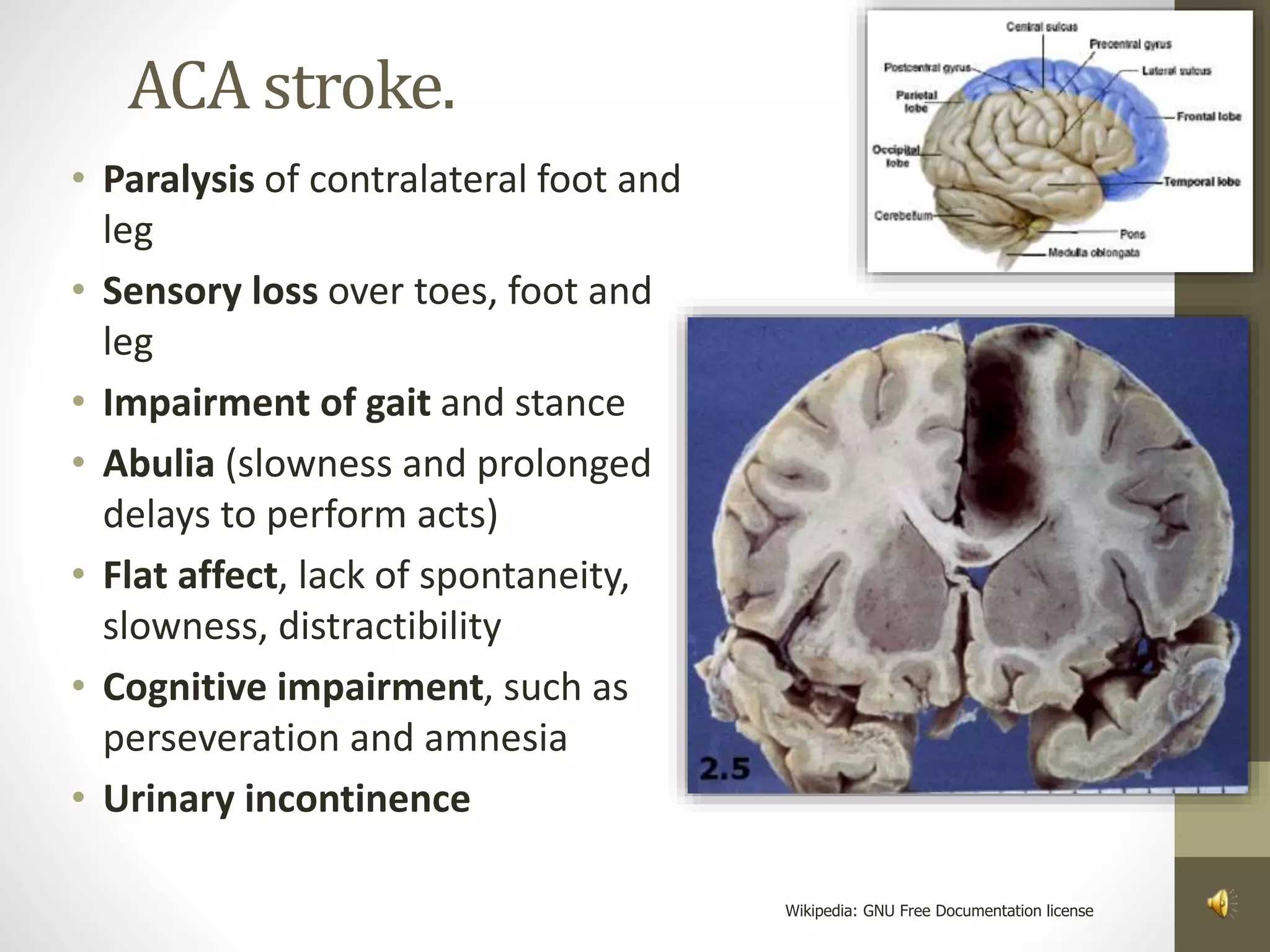
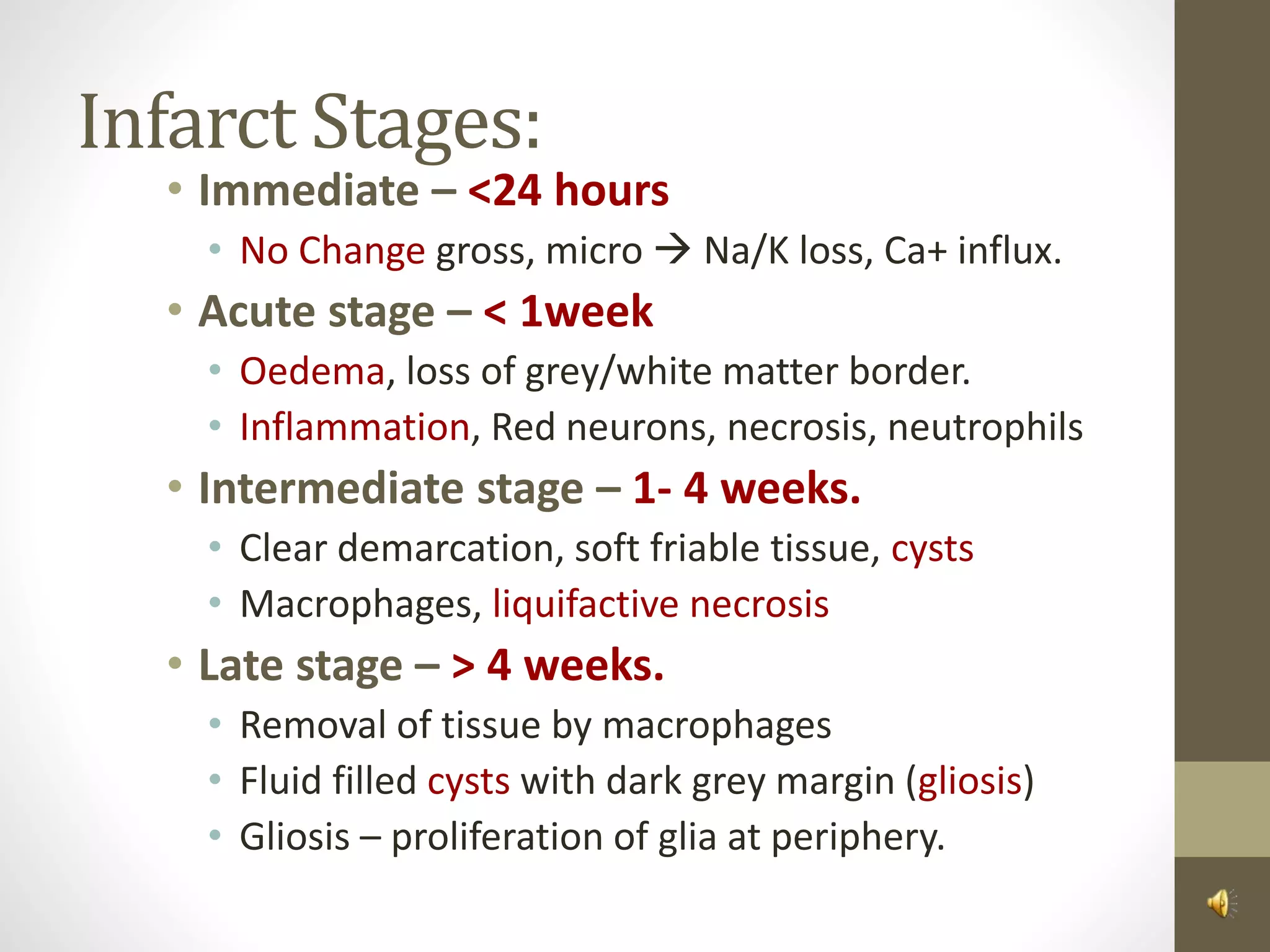
![Frontal[f*ck–motor]Lobe Functions:
• High level cognitive functions. i.e reasoning, abstraction,
concentration
• Storage of information – memory
• Control of voluntary eye movement
• Motor control of speech in the dominant hemisphere.
• Motor Cortex – Motor control of the contralateral side of
the body
• Urinary continence
• Emotion and personality](https://image.slidesharecdn.com/mhr4-stroke-101129110104-phpapp01/75/Stroke-uncensored-by-MHR-Corporation-11-2048.jpg)
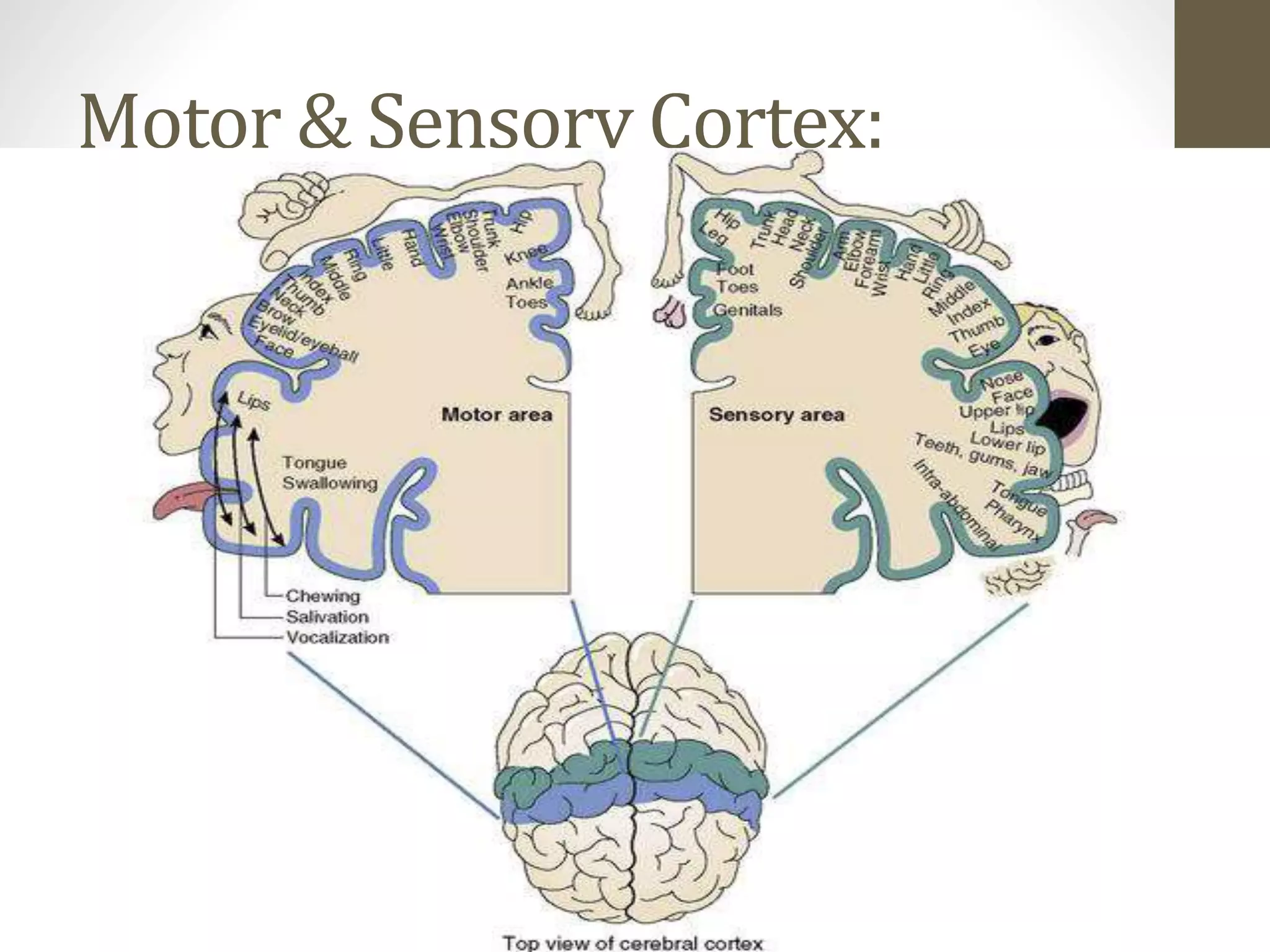
![Parietal[p-sx–sensory]Lobe Functions:
• Sensory cortex – sensory input is interpreted to define
size, weight, texture and consistency (contralateral)
• Sensation is localised, and modalities of touch, pressure
and position are identified.
• Awareness of the parts of body
• Non-dominant – processes visuospatial information and
• controls spatial orientation
• Dominant is involved in ideomotor praxis (ability to
perform learned motor tasks](https://image.slidesharecdn.com/mhr4-stroke-101129110104-phpapp01/75/Stroke-uncensored-by-MHR-Corporation-12-2048.jpg)
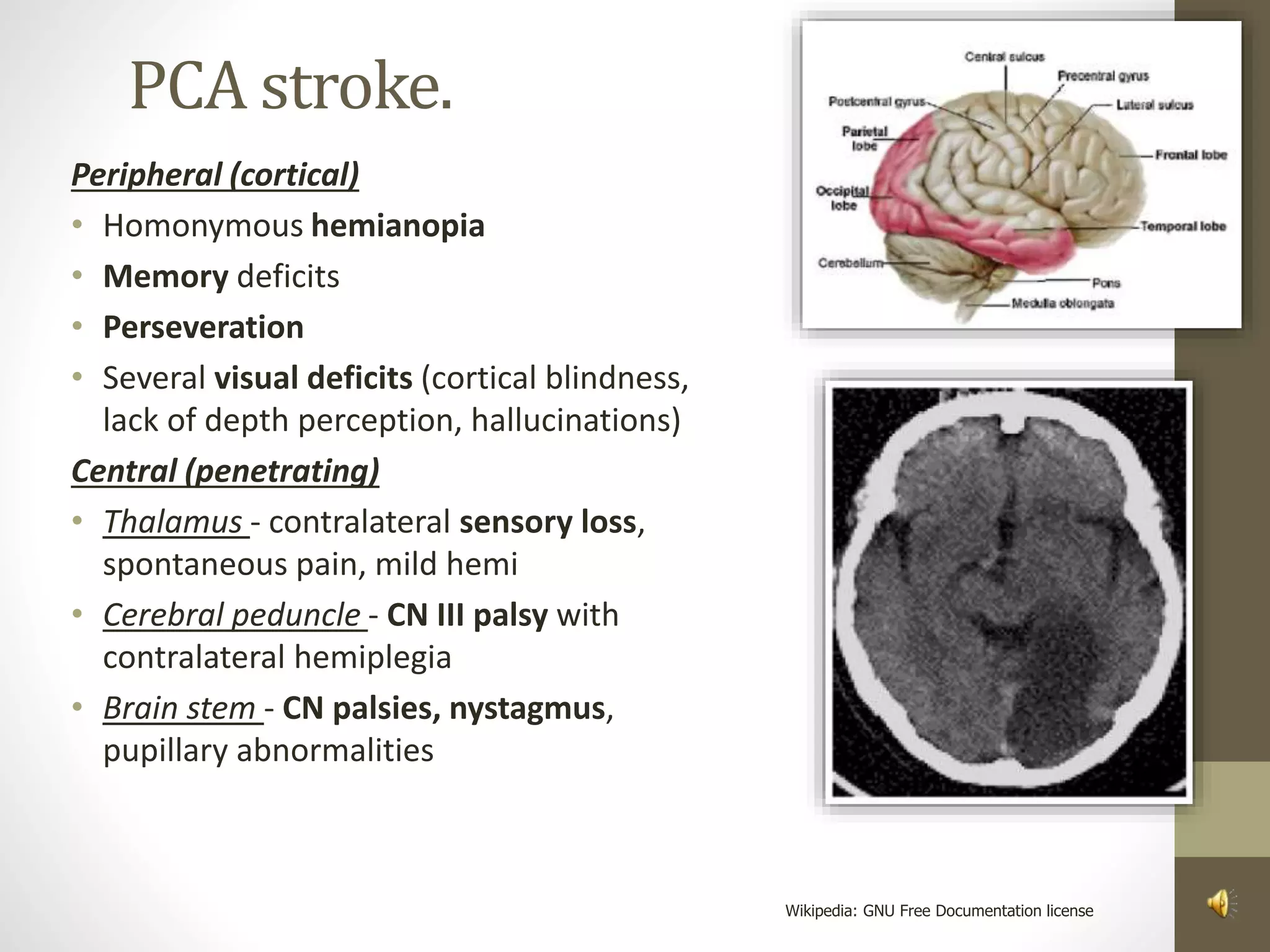
![Temporal[t-telinga]Lobe Functions:
• Primary auditory receptive areas
• In dominant ability to comprehend speech
(wernicke’s) – reception
• Interpretive area – area at the junction of the
temporal, parietal and occipital lobes.
• Plays an important role in visual, auditory and
olfactory perception
• Important role in learning; memory and
emotional affect.](https://image.slidesharecdn.com/mhr4-stroke-101129110104-phpapp01/75/Stroke-uncensored-by-MHR-Corporation-13-2048.jpg)
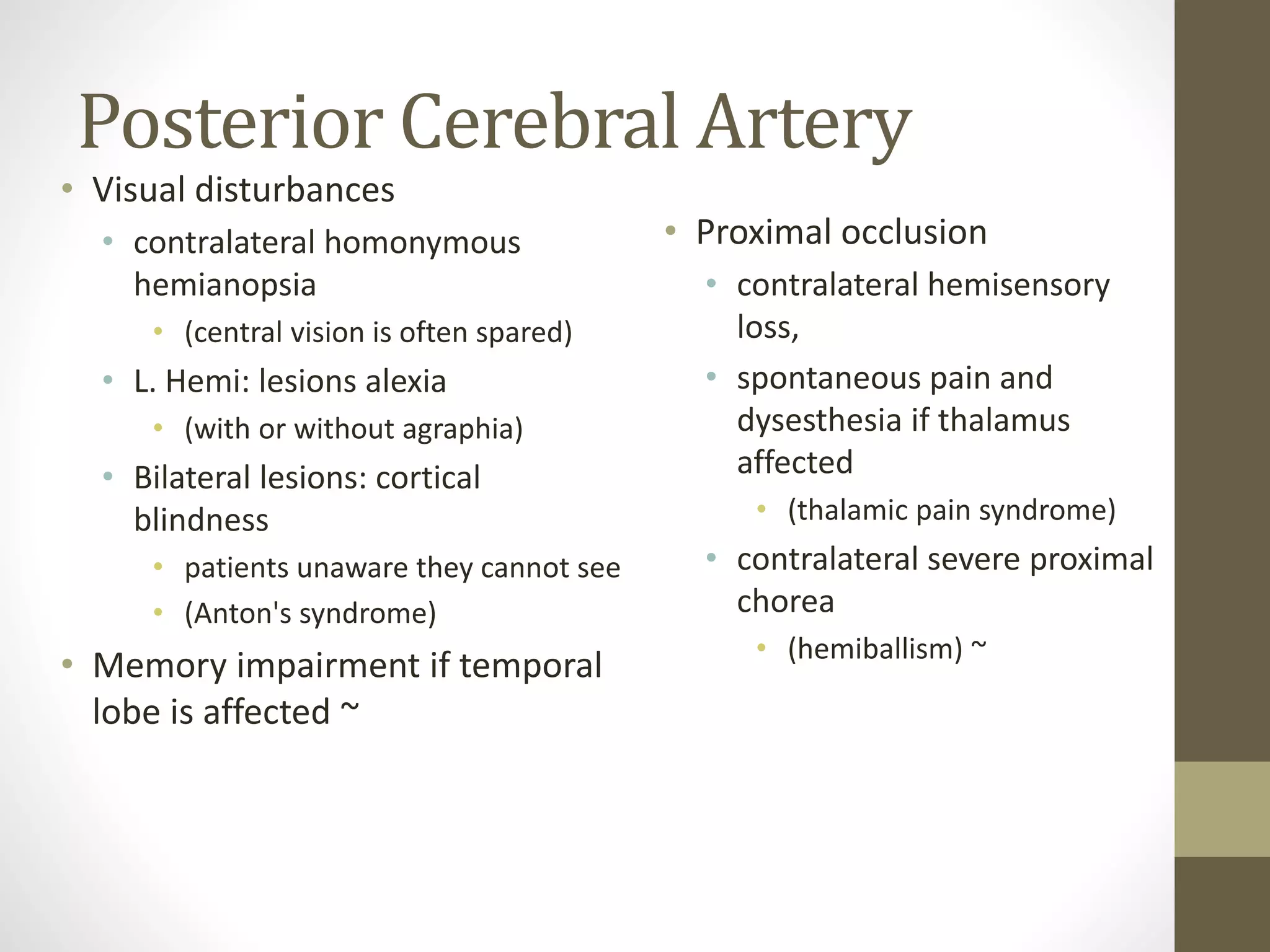
![Occipital[O-optic]Lobe Functions:
• Primary visual cortex
• Visual association areas
• Visual perception
• Some visual reflexes (i.e. visual
fixation)
• Involuntary smooth eye movement](https://image.slidesharecdn.com/mhr4-stroke-101129110104-phpapp01/75/Stroke-uncensored-by-MHR-Corporation-14-2048.jpg)

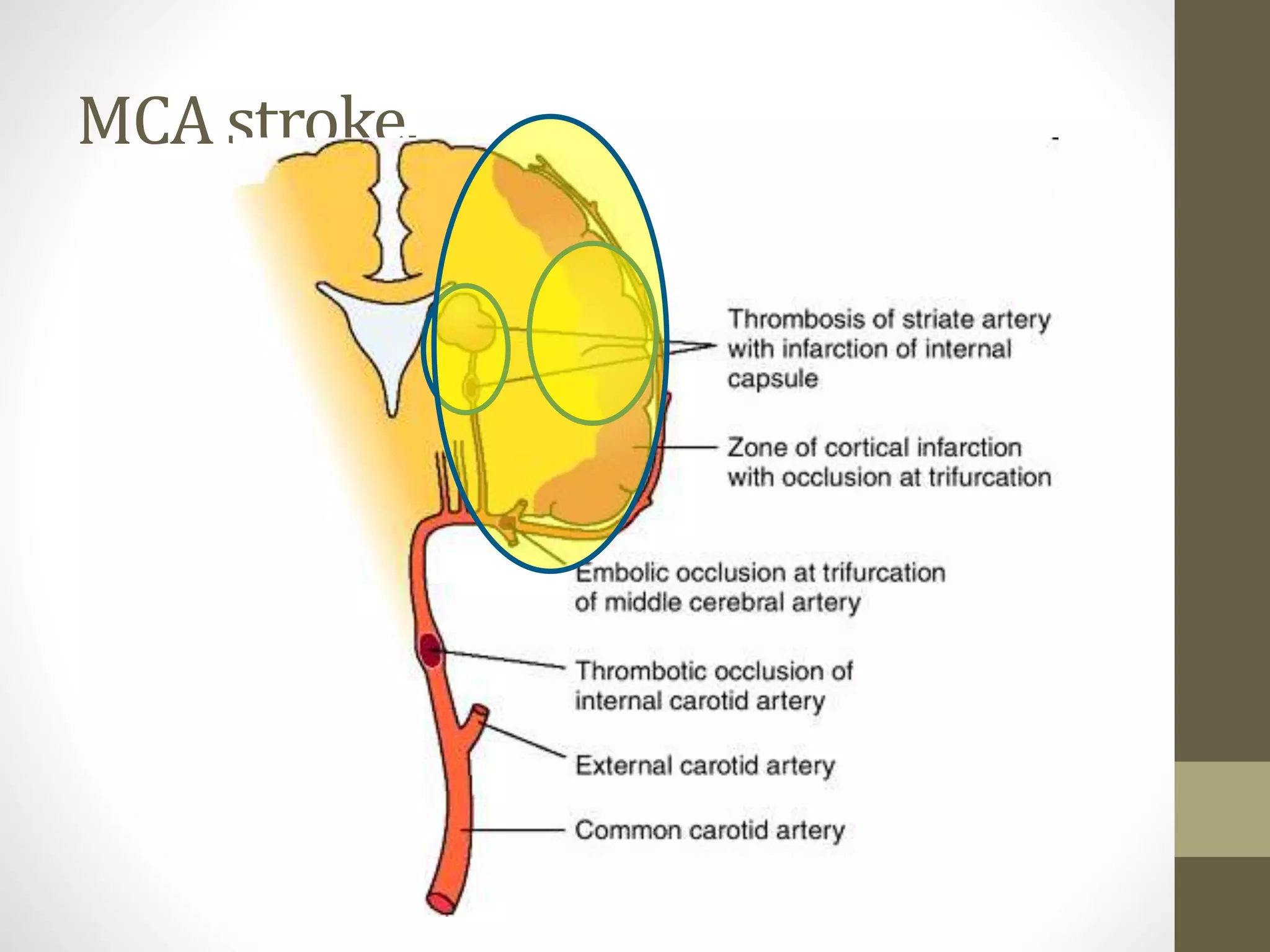
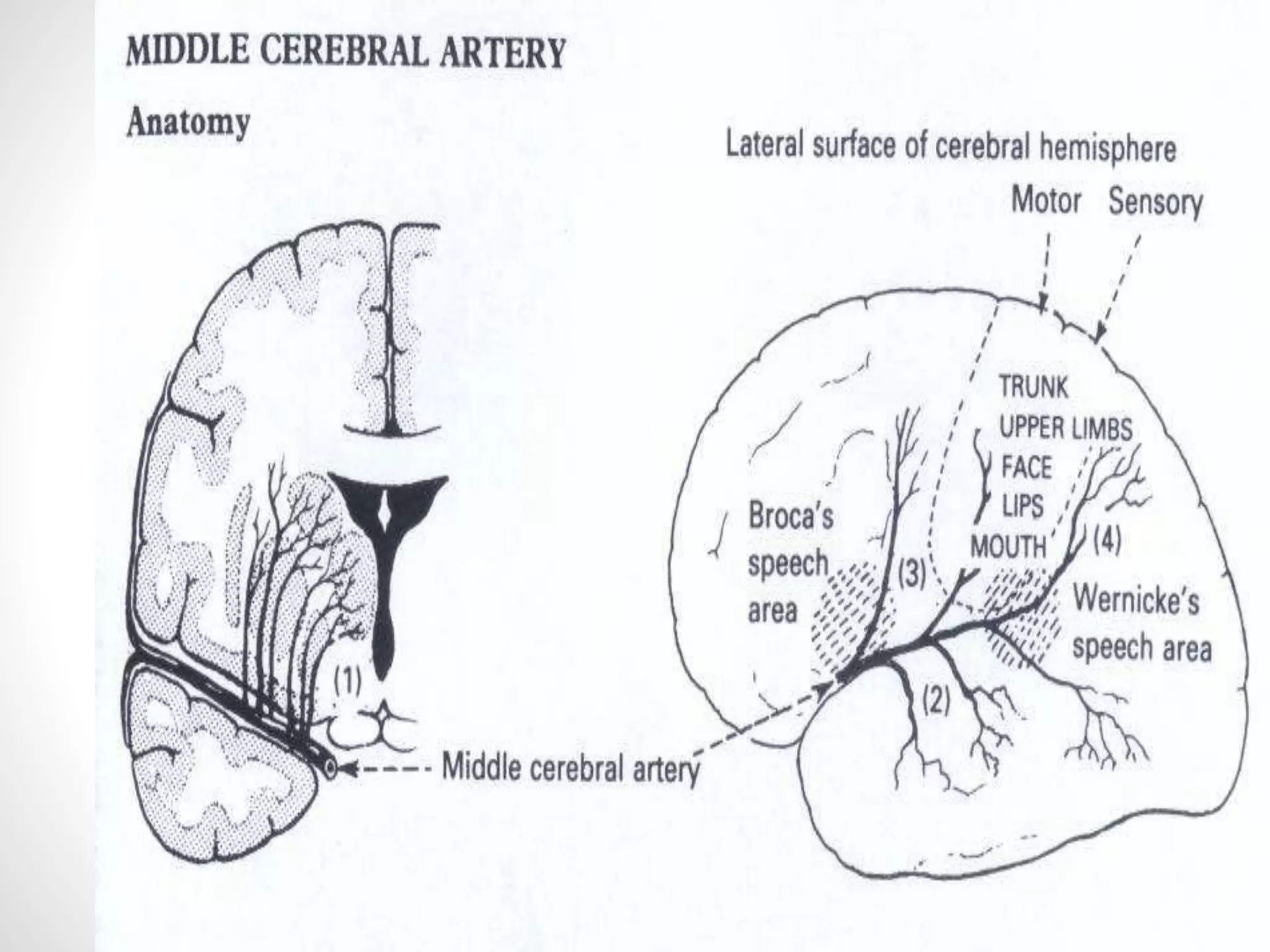
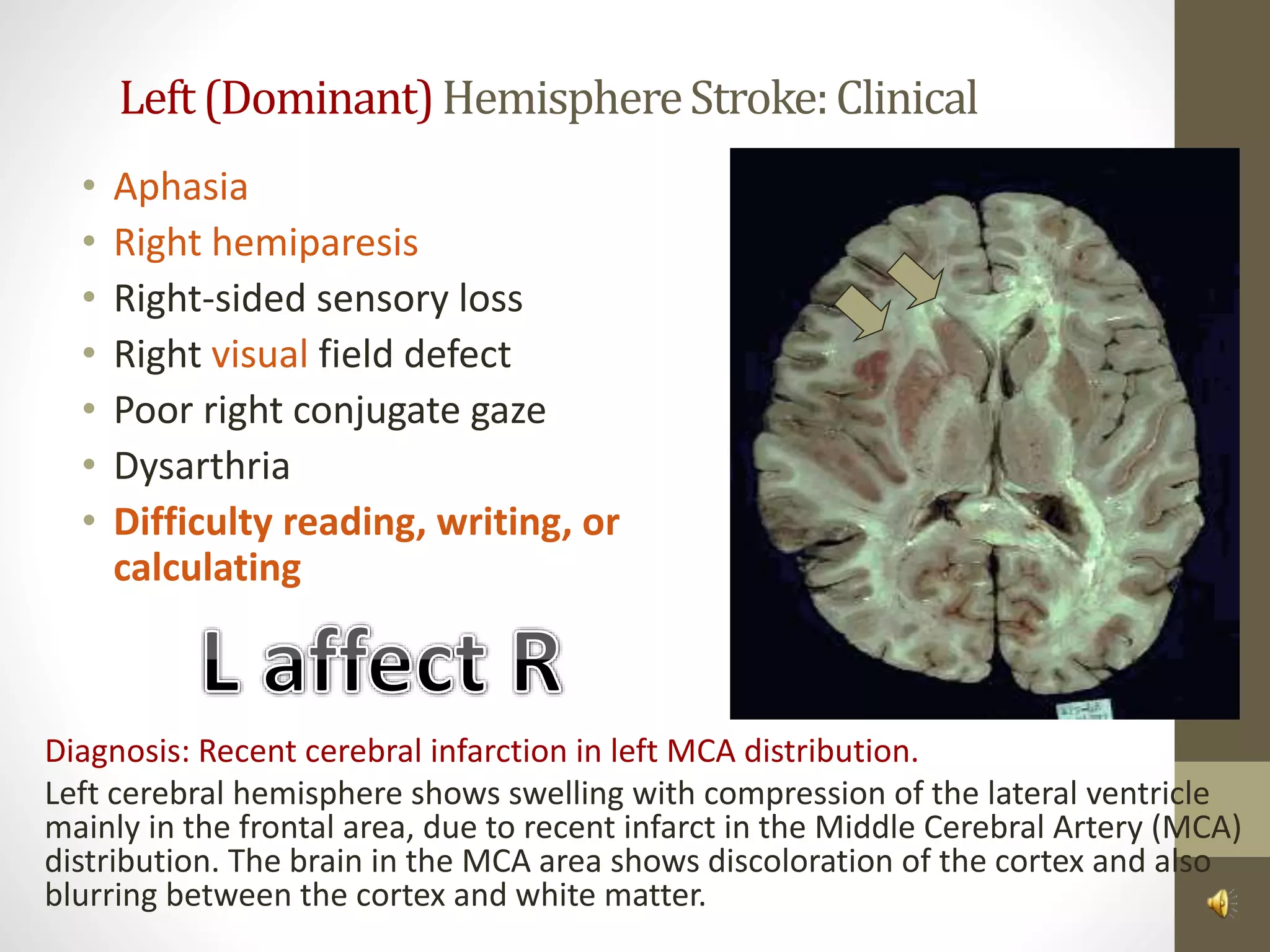
![MCA [mostcommon]Features:
• Paralysis of the contralateral
face, arm and leg
• Sensory impairment over the
contralateral face, arm & leg
• Homonymous hemi or
quadrantonopia
• Paralysis of gaze to the
opposite side
• Aphasia (dominant) and
dysarthria [broca/wernicke]
• Penetrating - contralateral
hemiplegia/paresis, slurred
speech.
• Impaired spatial perception](https://image.slidesharecdn.com/mhr4-stroke-101129110104-phpapp01/75/Stroke-uncensored-by-MHR-Corporation-34-2048.jpg)