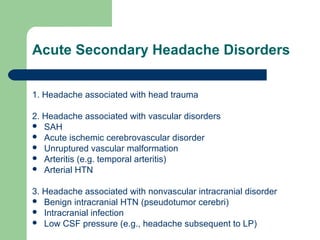
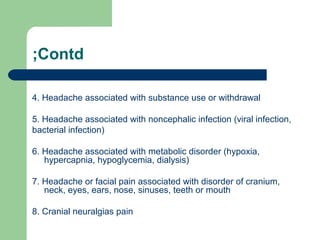
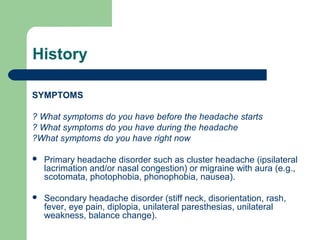
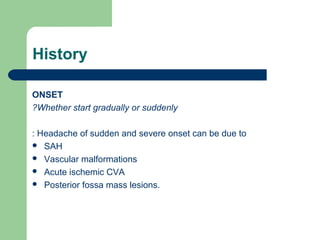
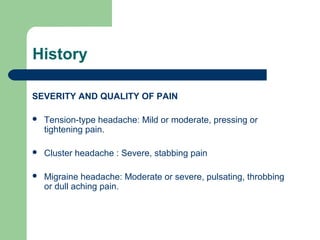
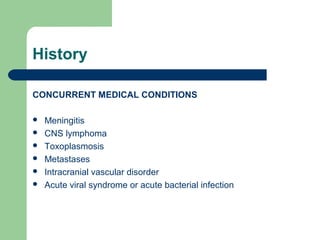
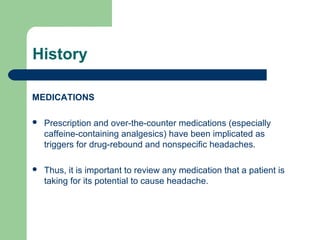
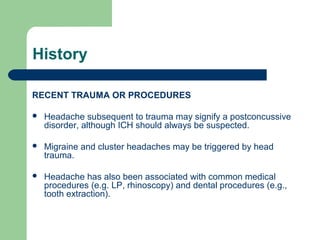
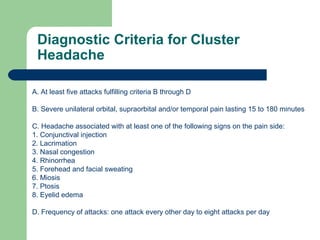
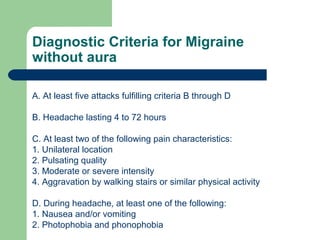
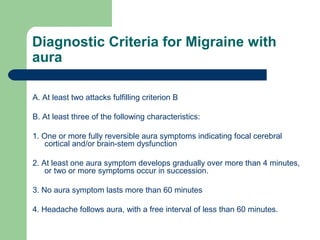
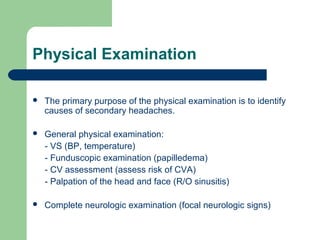
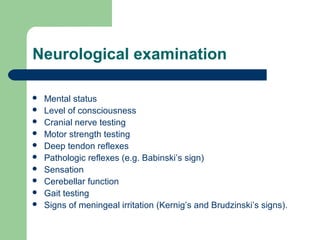
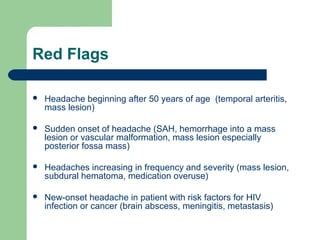
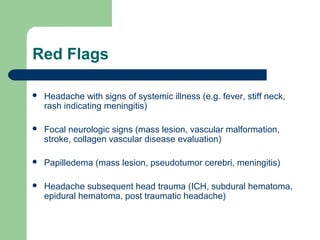
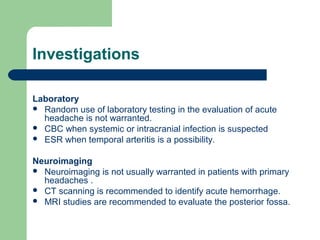
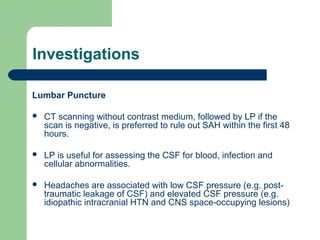
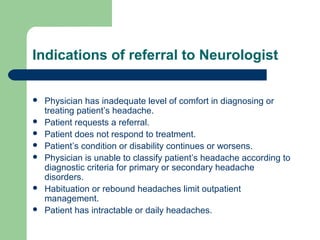
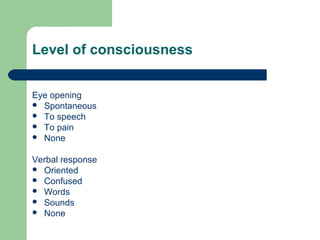
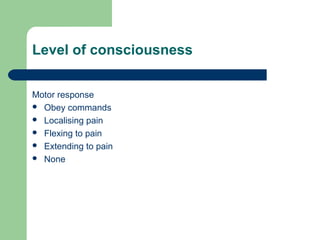
This document provides an overview of Dr. Faisal Al Hadad's approach to evaluating and diagnosing headaches. It begins with definitions of headache and classifications of primary versus secondary headaches. It then discusses taking a thorough history, including onset, location, severity of pain, concurrent conditions, medications, and recent trauma. The physical exam focuses on identifying secondary causes, and red flags requiring further investigation are outlined. Diagnostic criteria for common primary headaches like migraines and cluster headaches are provided. Recommendations are given for imaging, lumbar puncture, and indications for neurology referral. The goal is to distinguish primary from secondary headaches and accurately diagnose the underlying condition.