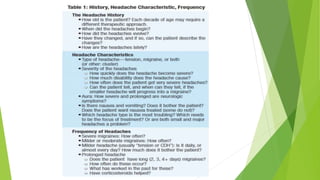
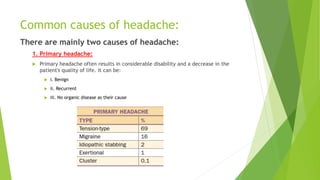
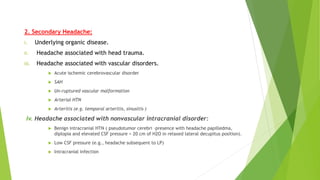
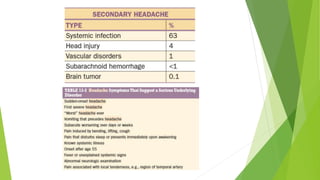
This document provides an overview of approaches to headache by Dr. Shivaom Chaurasia. It begins by defining headache and discussing common causes, which include primary headaches that often result in disability without an underlying organic disease, and secondary headaches that have a specific underlying cause like head trauma, vascular disorders, or nonvascular intracranial disorders. The document then examines the pathophysiology of headache, important aspects to cover in a headache history, potential investigations, management strategies for different headache types including migraine, tension, and cluster headaches, and indicators for referral to a neurologist.
![Classification:
Primary headache syndromes include migraines with (classic) or without
(common) aura, the hemicranias and indomethacin-responsive headaches,
tension headaches, chronic daily headaches, and cluster headaches.
Secondary headaches have specific etiologies, and symptomatic features
vary depending on the underlying pathology (i.e., SAH, tumor, hypertension,
posterior reversible encephalopathy syndrome [PRES], analgesic overuse,
iatrogenic).
Migraine without aura (common): At least five attacks that last 4 to 72
hours.Symptomsshouldincludeatleasttwoofthefollowing:unilaterallocation,puls
atingorthrobbing,moderatetosevereinintensity,aggravatedbyactivity,andatleas
tone of these associated features: nausea/vomiting, photophobia, and/or
phonophobia.
Migraine with aura (classic): Same as the aforementioned, except at least
two attacks with an associated aura that lasts from 4 minutes to 1 hour
(longer than 60 minutes is a red flag). The aura should have a gradual onset,
be fully reversible, and can occur before, with, or after headache onset](https://image.slidesharecdn.com/approachtoheadachefinalshivaom-200622121712/85/Approach-to-headache-final-shivaom-6-320.jpg)