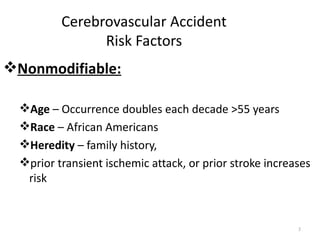
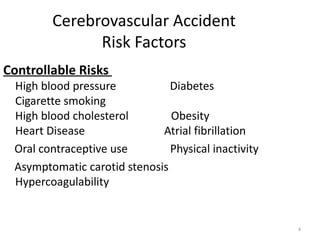
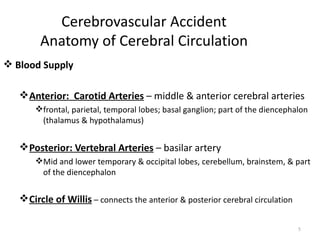
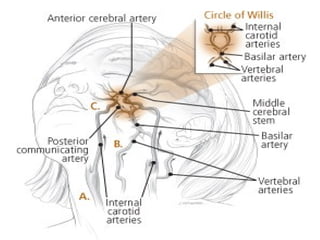
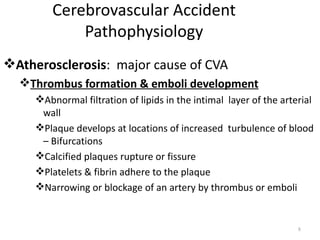
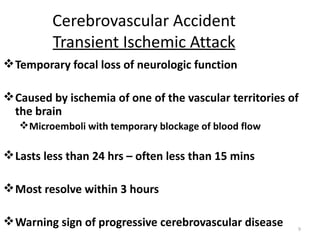
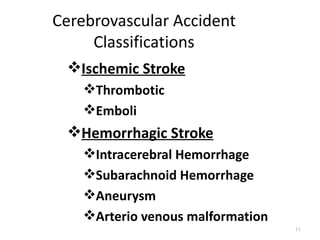
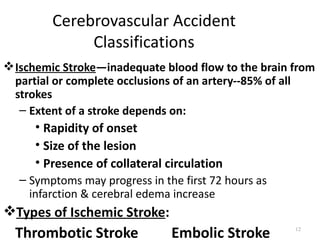
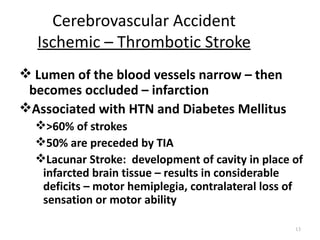
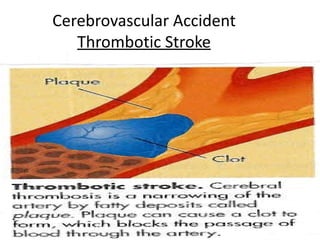
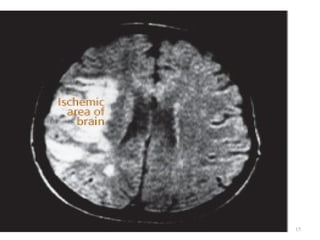
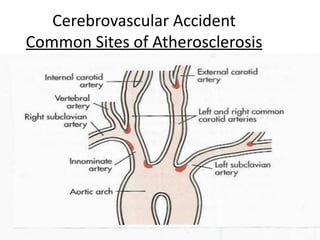
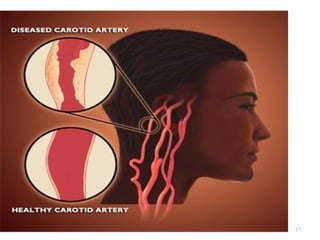
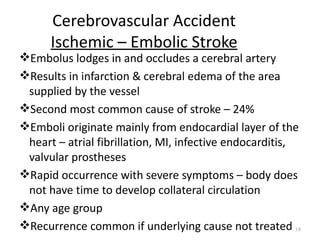
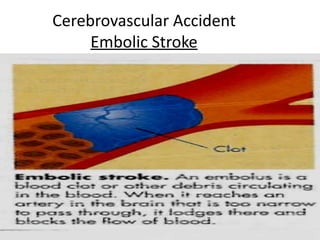
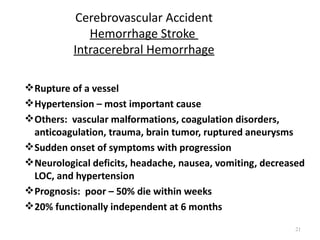
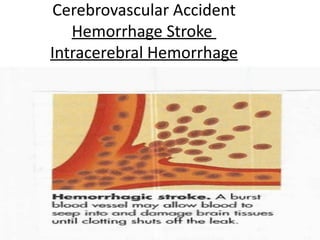
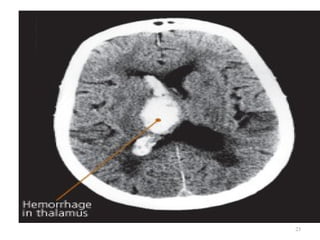
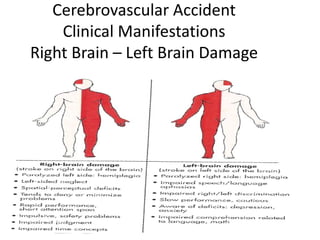
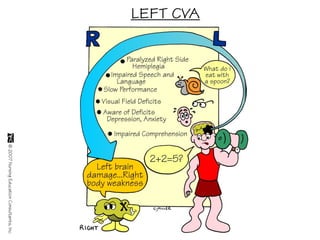
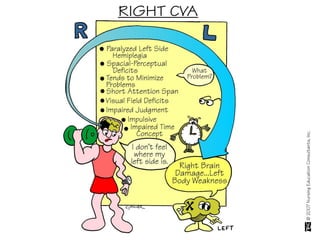
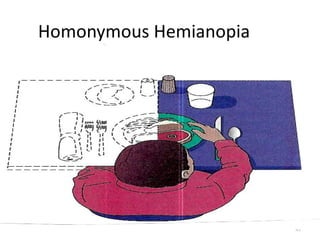
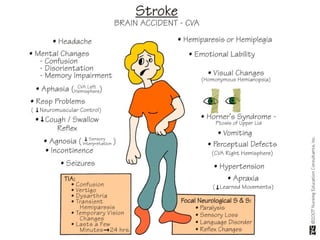
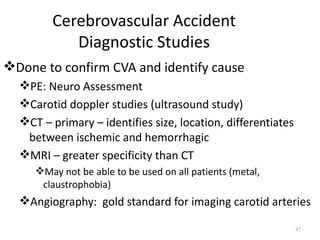
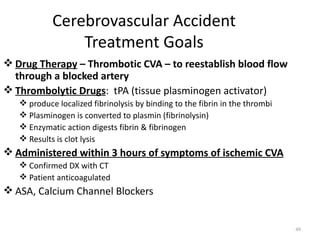
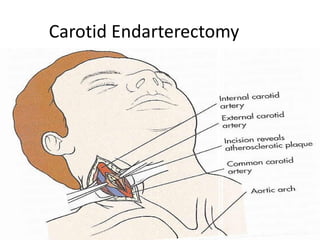
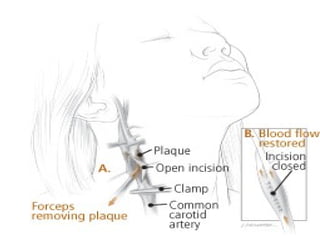
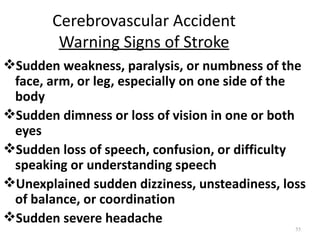
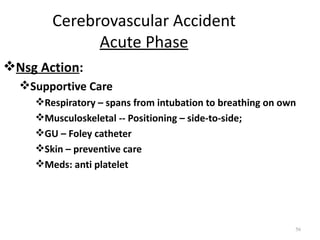
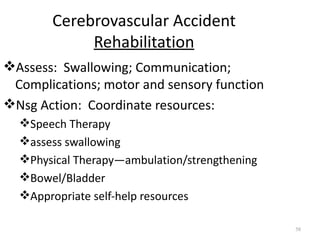
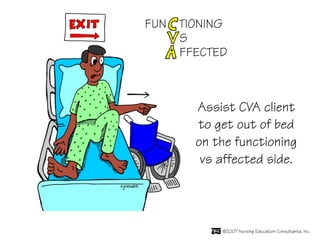
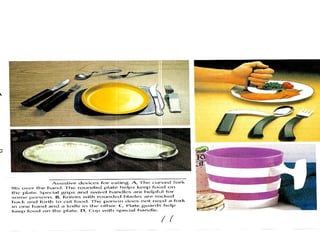
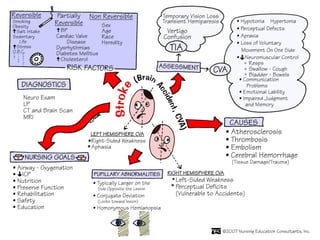
A cerebrovascular accident (CVA), also known as a stroke, is caused by the loss of blood flow to an area of the brain resulting in cell death. It is a leading cause of death and disability. The majority of strokes are ischemic and caused by blockage of an artery by a clot or debris. Hemorrhagic strokes occur when a blood vessel ruptures, causing bleeding into or around the brain. Treatment focuses on prevention through risk factor control as well as acute interventions like clot-busting drugs. Rehabilitation aims to maximize recovery of function and independence.