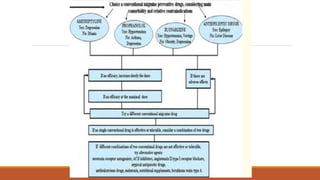
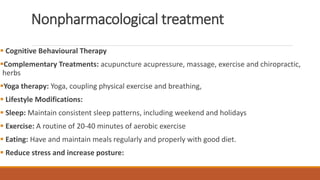
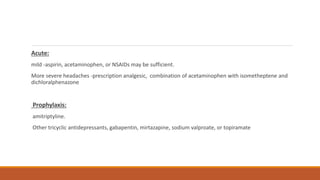
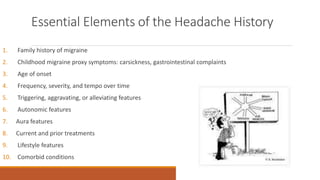
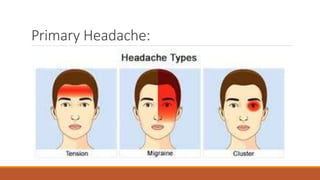
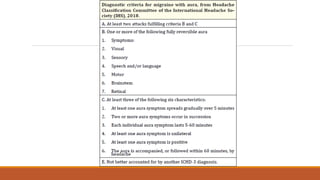
This document discusses headaches, including red flags that indicate the need for evaluation of headaches, essential elements of a headache history, characteristics of migraine headaches, and cluster headaches. It provides details on the signs and symptoms, pathogenesis, diagnosis, and treatment of migraine headaches, including preventative and acute treatment options. It also covers potential complications of migraines and medication overuse headaches.




















![Treatment and Management
Reassurance.
A normal head CT or MRI scan may offer considerable reassurance.
Medication use should be reviewed and modified if necessary. The use of drugs known to cause headaches (e.g.,
reserpine, nifedipine, theophylline derivatives, caffeine, vasodilators [including long-acting nitrates], alcohol)
should be discontinued, or substituted to other agents if possible.
Exercise programs to promote well-being, correction of dietary excesses, and avoidance of prolonged fasts and
irregular sleeping habits can be helpful
Long-term stress management may require the help of a psychologist or other appropriately trained professional.
Useful self-management techniques include biofeedback, relaxation .training, hypnosis, and cognitive behavioral
training](https://image.slidesharecdn.com/primaryheadache-200605144452/85/Primary-headache-32-320.jpg)