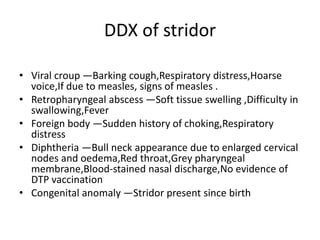
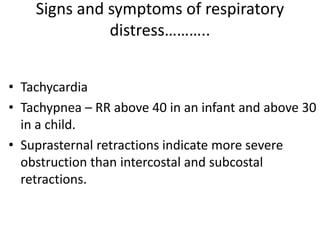
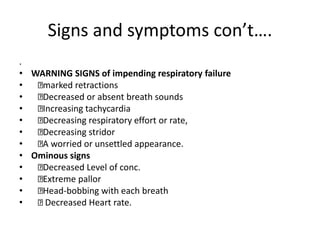
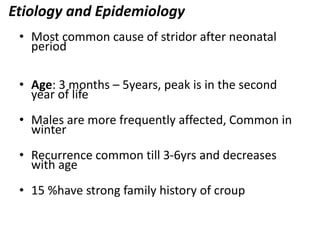
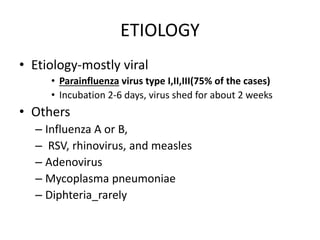
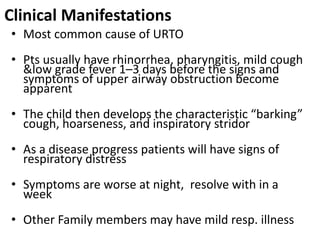
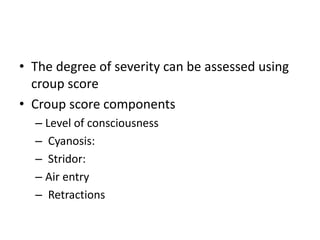
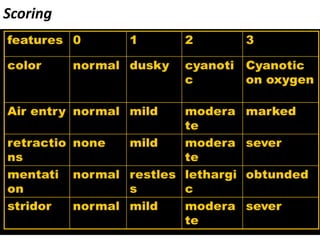
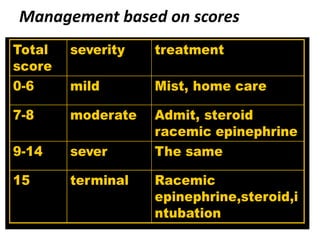
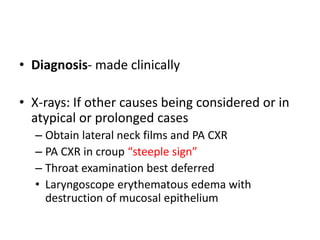
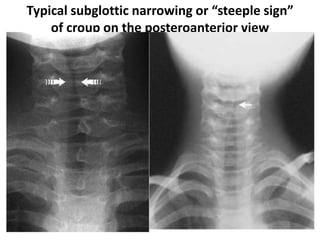
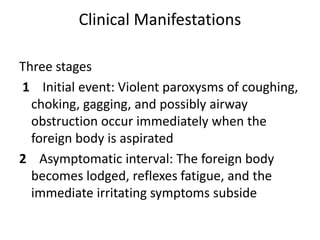
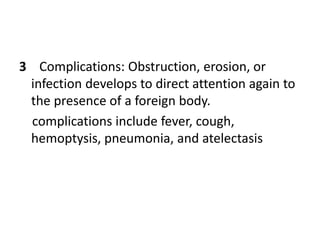
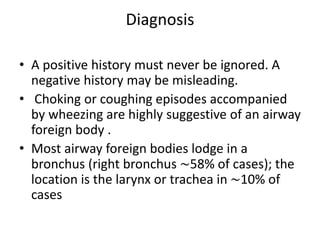
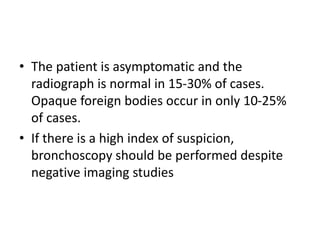
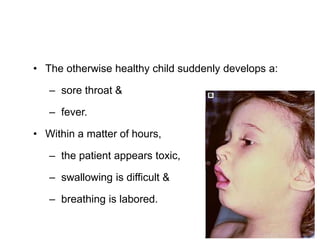
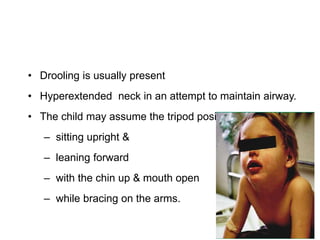
This document summarizes a seminar on upper airway obstruction. It discusses various causes of upper airway obstruction in children including croup, foreign body aspiration, and other conditions. It provides details on the signs, symptoms, diagnosis, and management of croup as the most common cause. For croup, it describes the characteristic barking cough and inspiratory stridor. It outlines criteria for discharge after croup episodes and complications. The document also briefly discusses approaches to examining patients with upper airway obstruction and foreign body aspiration.