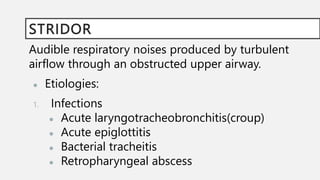
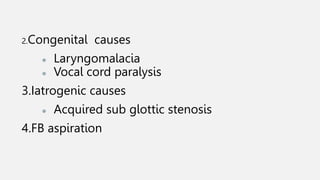
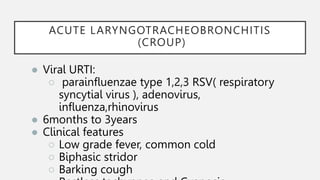
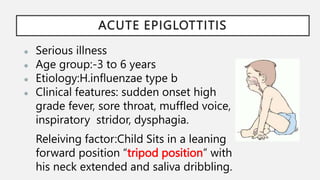
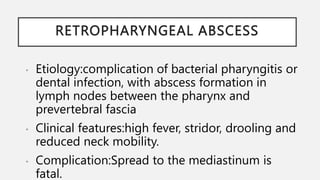
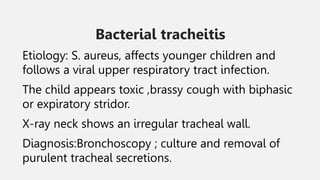
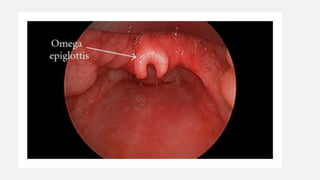
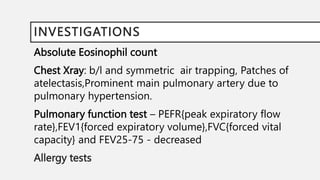
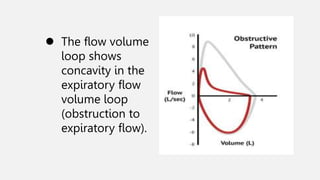
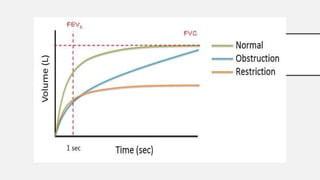
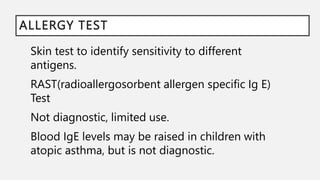
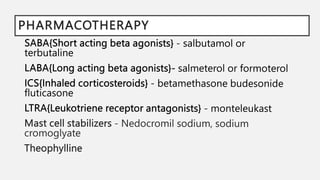
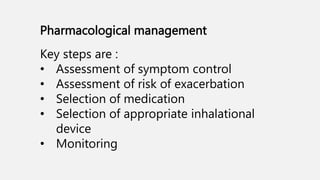
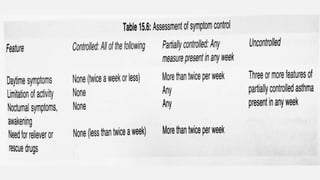
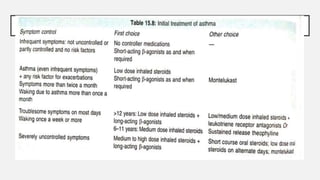
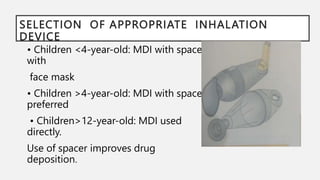
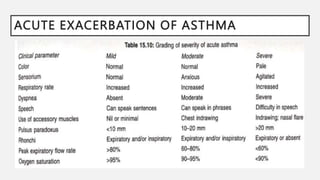
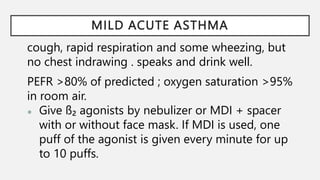
This document provides information on wheezing and stridor in children, including the causes, clinical features, diagnosis, and management of various conditions. It discusses stridor resulting from infections like croup and epiglottitis. It also covers stridor from congenital causes such as laryngomalacia and vocal cord paralysis. Wheezing can be caused by asthma, infections, cystic fibrosis, and other conditions. The diagnosis and treatment of asthma is discussed in detail, including identifying triggers, clinical assessment, pulmonary function tests, and the goals and components of long-term pharmacological management and education.