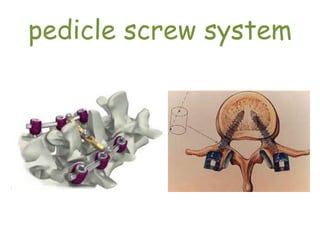
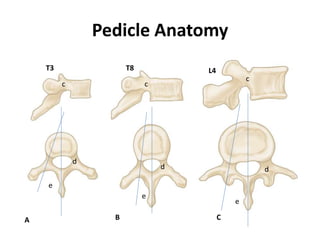
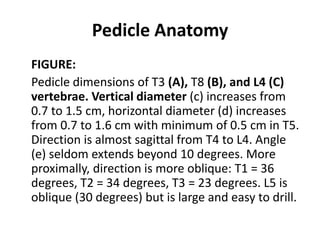
The document outlines the pedicle screw fixation technique for spinal stabilization, detailing its indications and contraindications. It describes the anatomy of pedicles, including their varying dimensions and angles throughout the spine, and discusses techniques for localizing pedicle entry points. The emphasis is on the importance of preoperative planning and proper screw trajectory to minimize potential complications.