Dr. Mahak Jain presented on spondylolisthesis. Key points include:
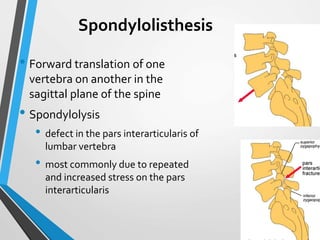
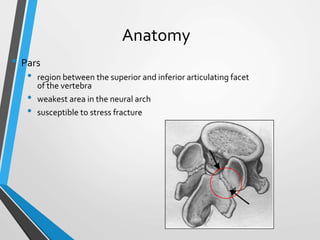
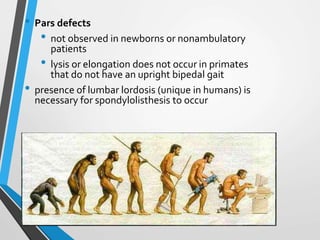
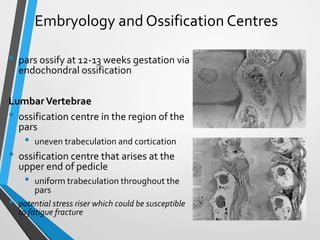
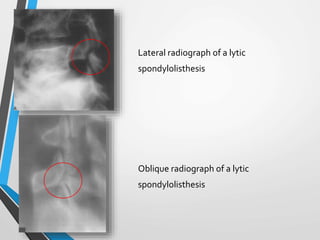
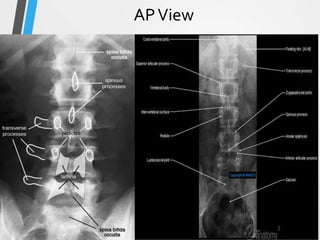
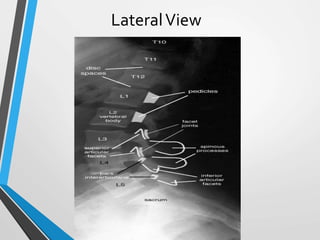
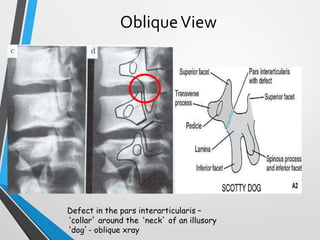
1) Spondylolisthesis is the forward translation of one vertebra on another, commonly caused by defects in the pars interarticularis known as spondylolysis.
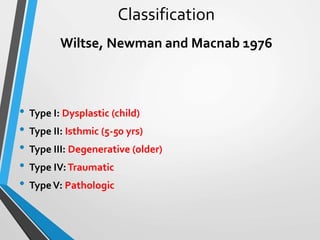
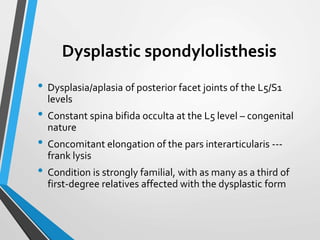
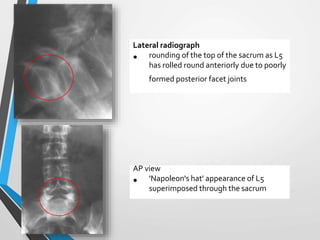
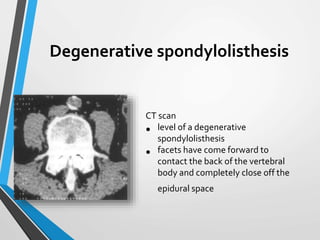
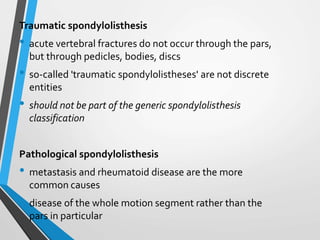
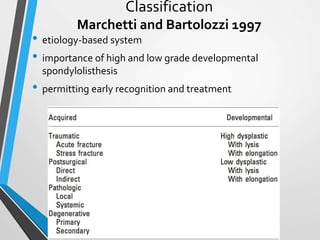
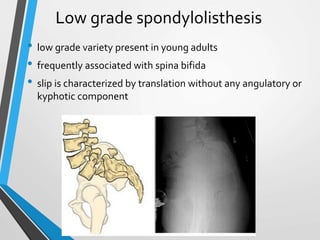
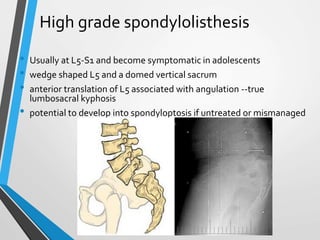
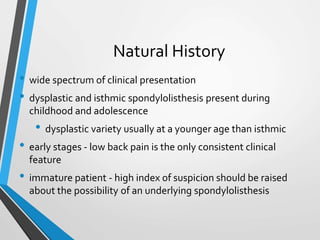
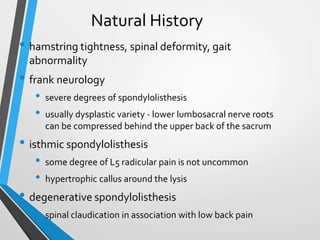
2) It is classified based on etiology, with dysplastic, isthmic, degenerative, traumatic, and pathological types.
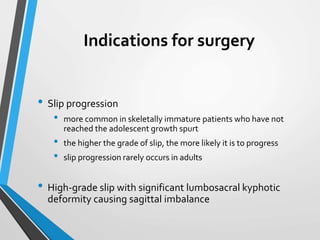
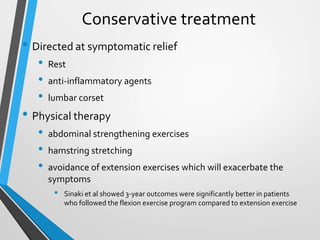
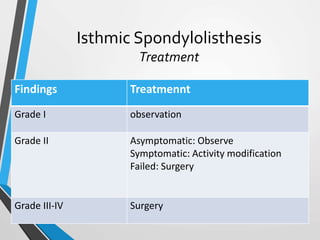
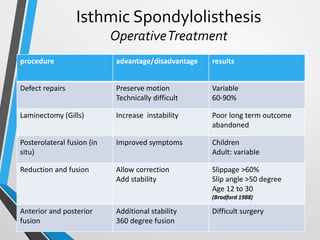
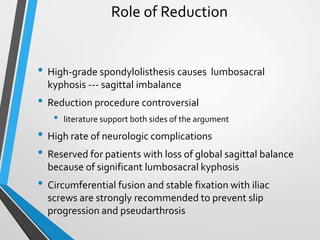
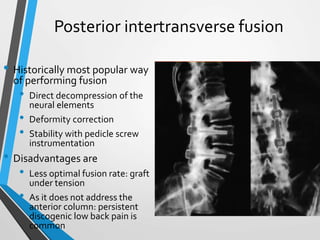
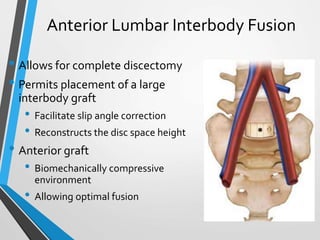
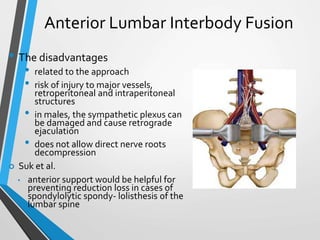
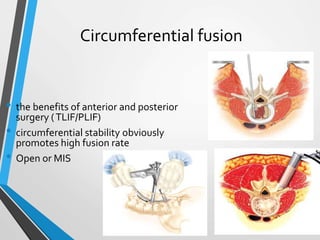
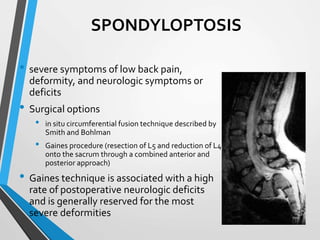
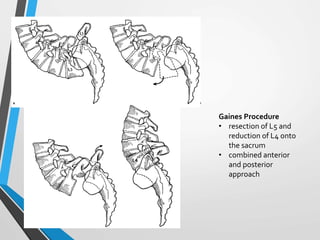
3) Treatment depends on factors like grade, symptoms, and etiology, ranging from conservative care to surgical options like decompression, fusion, and instrumentation.
4) Studies show surgery with fusion has better outcomes for pain and function than nonsurgical treatment or decompression alone for degenerative