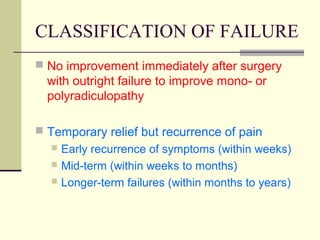
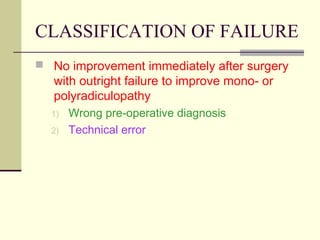
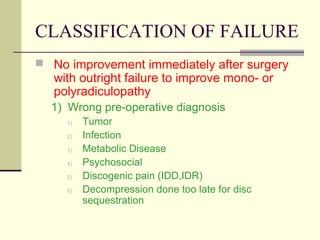
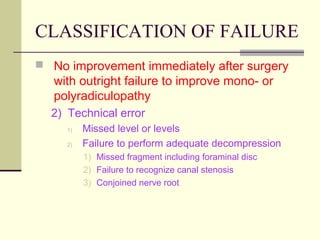
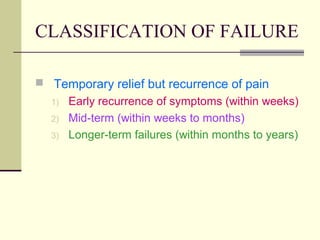
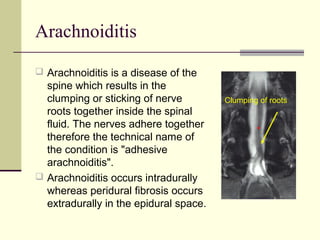
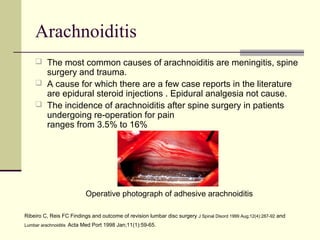
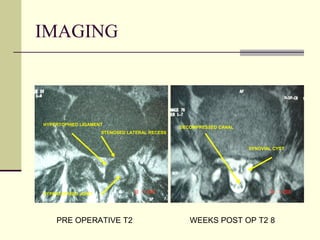
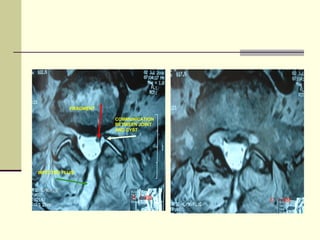
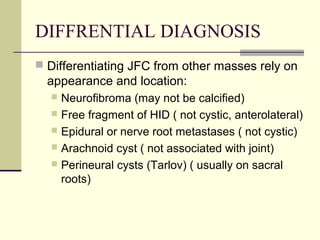
This document discusses failed back syndrome, specifically defining it as any condition where there is failure to improve satisfactorily following back surgery. It then classifies failures into those with no immediate improvement and temporary relief but recurrence of pain within weeks, months, or years. Causes of failures include wrong diagnosis, technical errors during surgery, infection, arachnoiditis, and recurrent stenosis. The document also discusses juxtafacet cysts near facet joints.