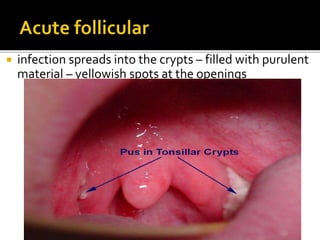
The tonsils are collections of lymphatic tissue located in the throat. They include the palatine tonsils located in the lateral walls of the throat. The tonsils have a medial epithelial surface with crypts and a lateral fibrous capsule. They receive blood supply from facial and lingual arteries and drain into deep cervical lymph nodes. Acute tonsillitis is usually a viral infection causing sore throat while chronic tonsillitis results from recurrent infections. Complications include peritonsillar abscess. Treatment involves pain relief, antibiotics for acute infections, and tonsillectomy for recurrent cases.