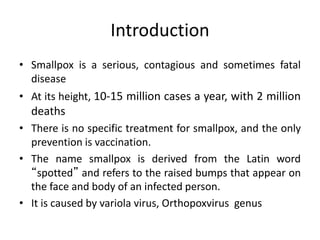
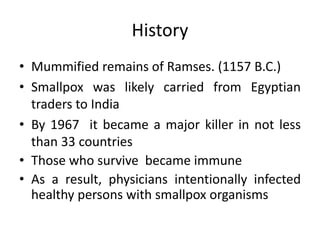
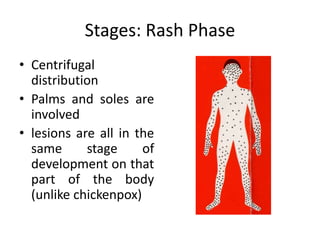
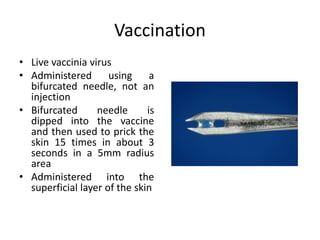
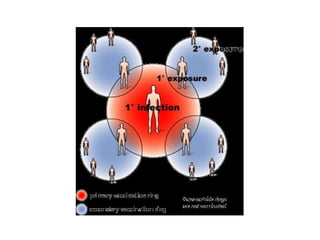
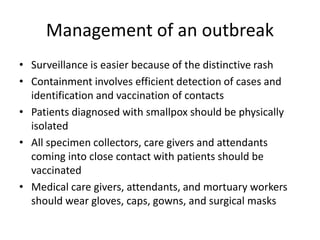
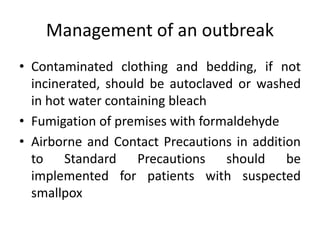
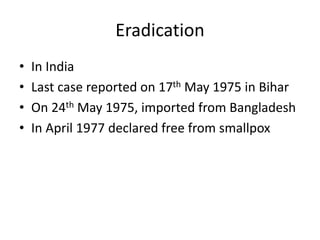
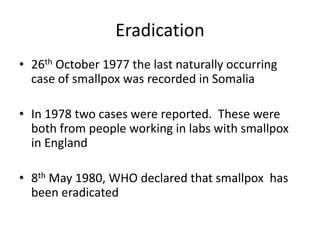
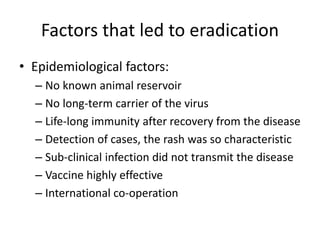
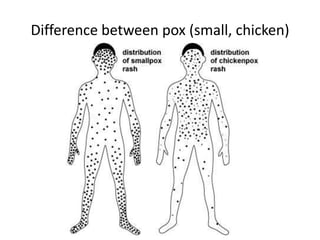
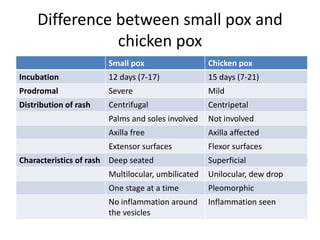
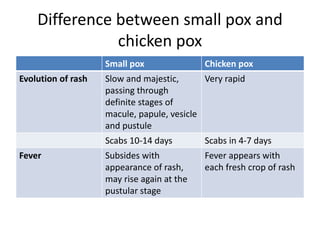
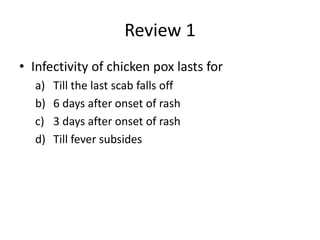
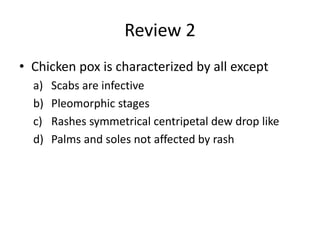
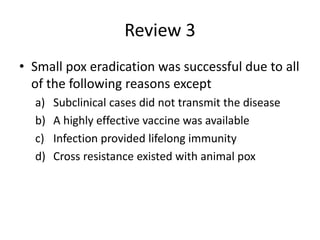
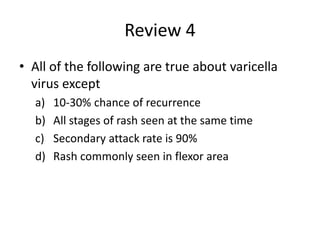
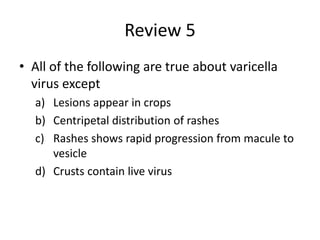
The document provides information on smallpox (variola) and chickenpox (varicella). It describes the epidemiology, clinical features, transmission, prevention and control of both diseases. Key differences between smallpox and chickenpox are enumerated. Smallpox was eradicated through a global vaccination program due to factors like no animal reservoir, effective vaccine, and lifelong immunity after infection. Chickenpox is generally a mild self-limiting disease caused by the varicella zoster virus.