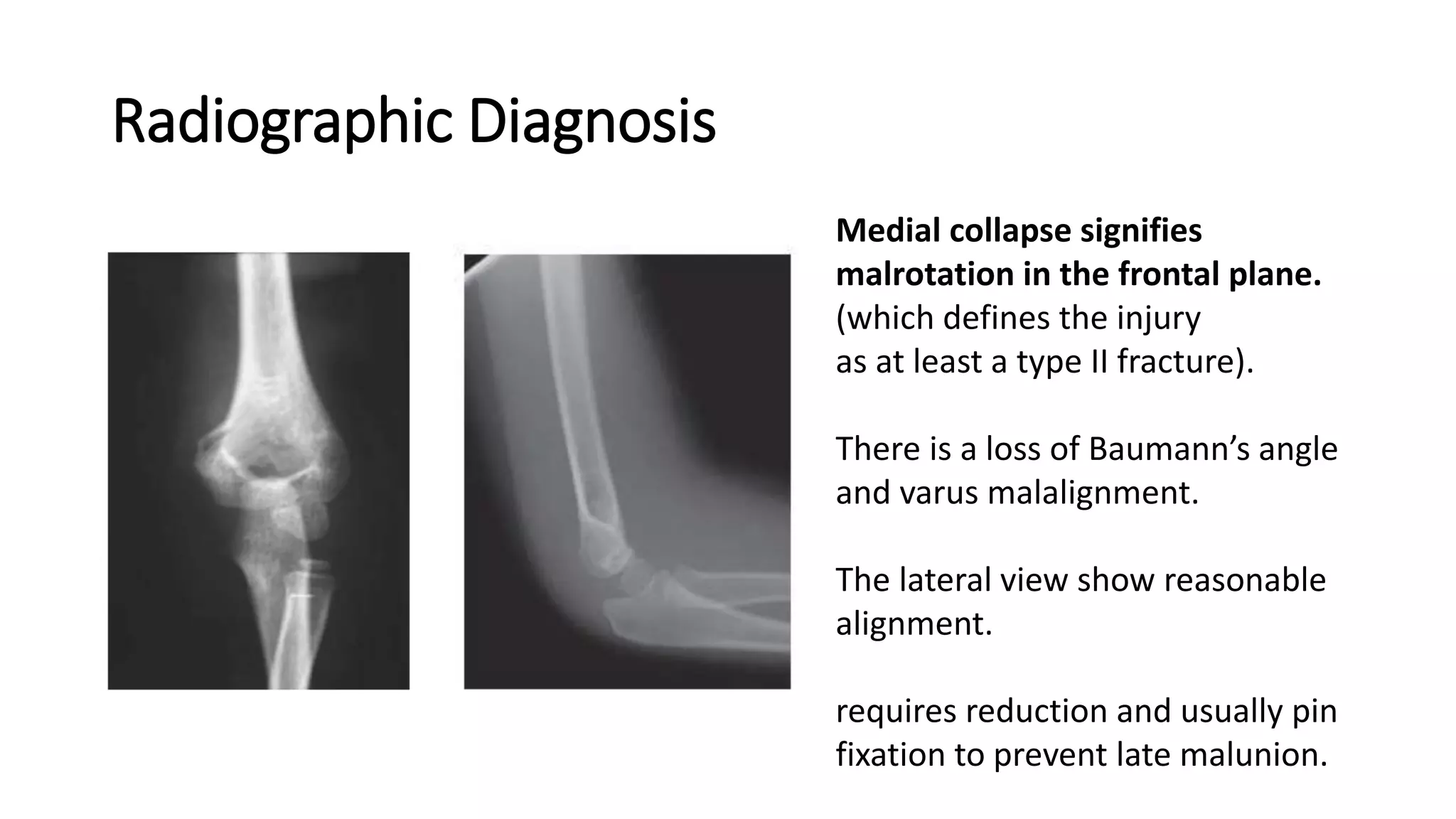
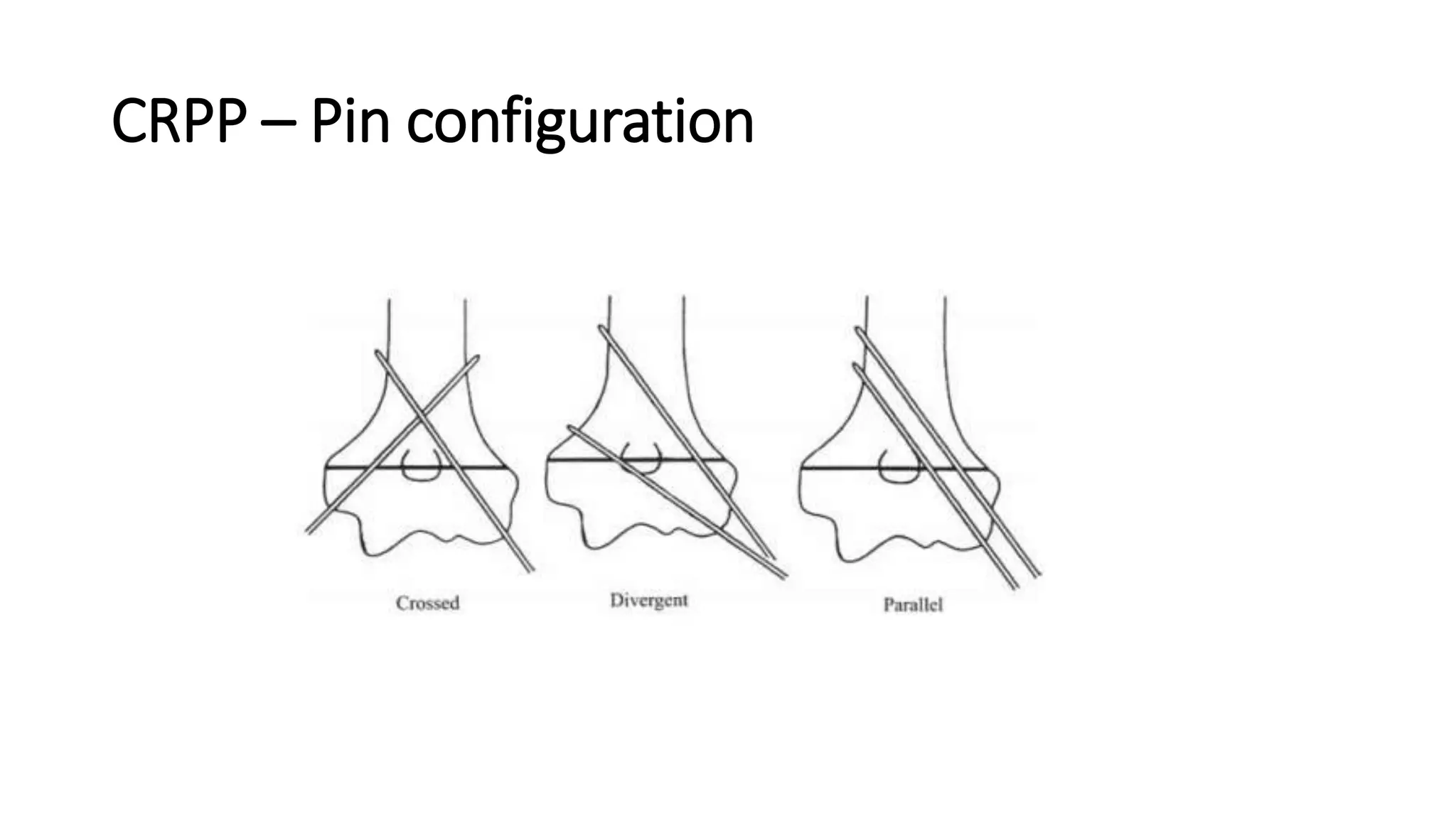
The document discusses supracondylar fractures of the distal humerus, emphasizing their prevalence in children aged 5-7 and the mechanisms of injury, which are predominantly extension-type fractures. It outlines Gartland classification for these fractures, emphasizing the importance of accurate radiographic diagnosis, initial management strategies, and various treatment options ranging from casting to surgical interventions. Additionally, it addresses potential complications and the significance of ongoing monitoring for neurological and vascular injuries during and after treatment.