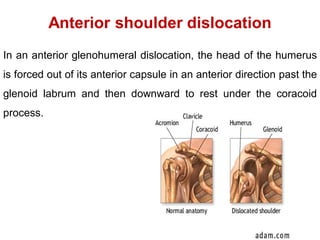
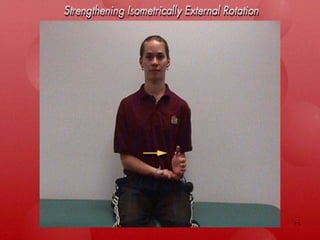
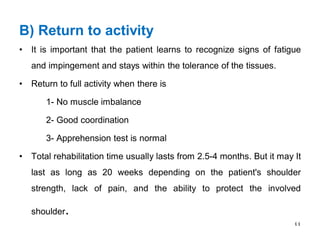
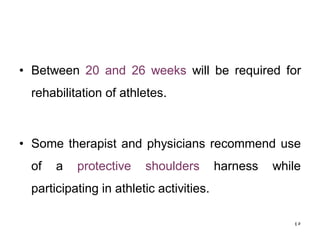
Shoulder dislocations can be anterior, posterior, or inferior. Anterior dislocations are the most common type, often resulting from sports injuries. Treatment involves reducing the dislocation followed by immobilization or physical therapy. The goal of rehabilitation is to restore range of motion, strengthen stabilizing muscles like rotator cuffs, and allow a gradual return to normal activities over 2-4 months. Recurrence rates remain high, especially in young active patients.