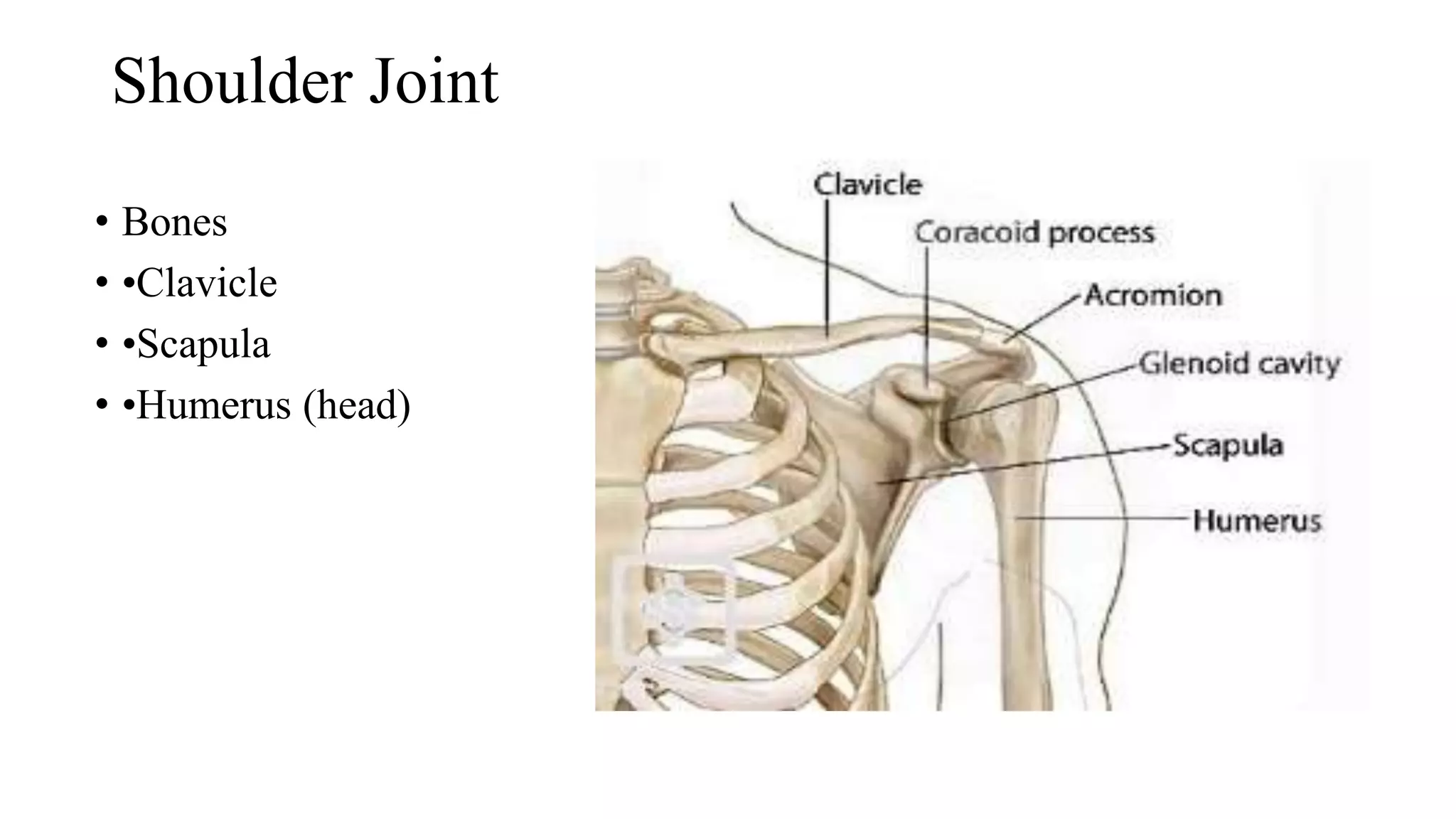
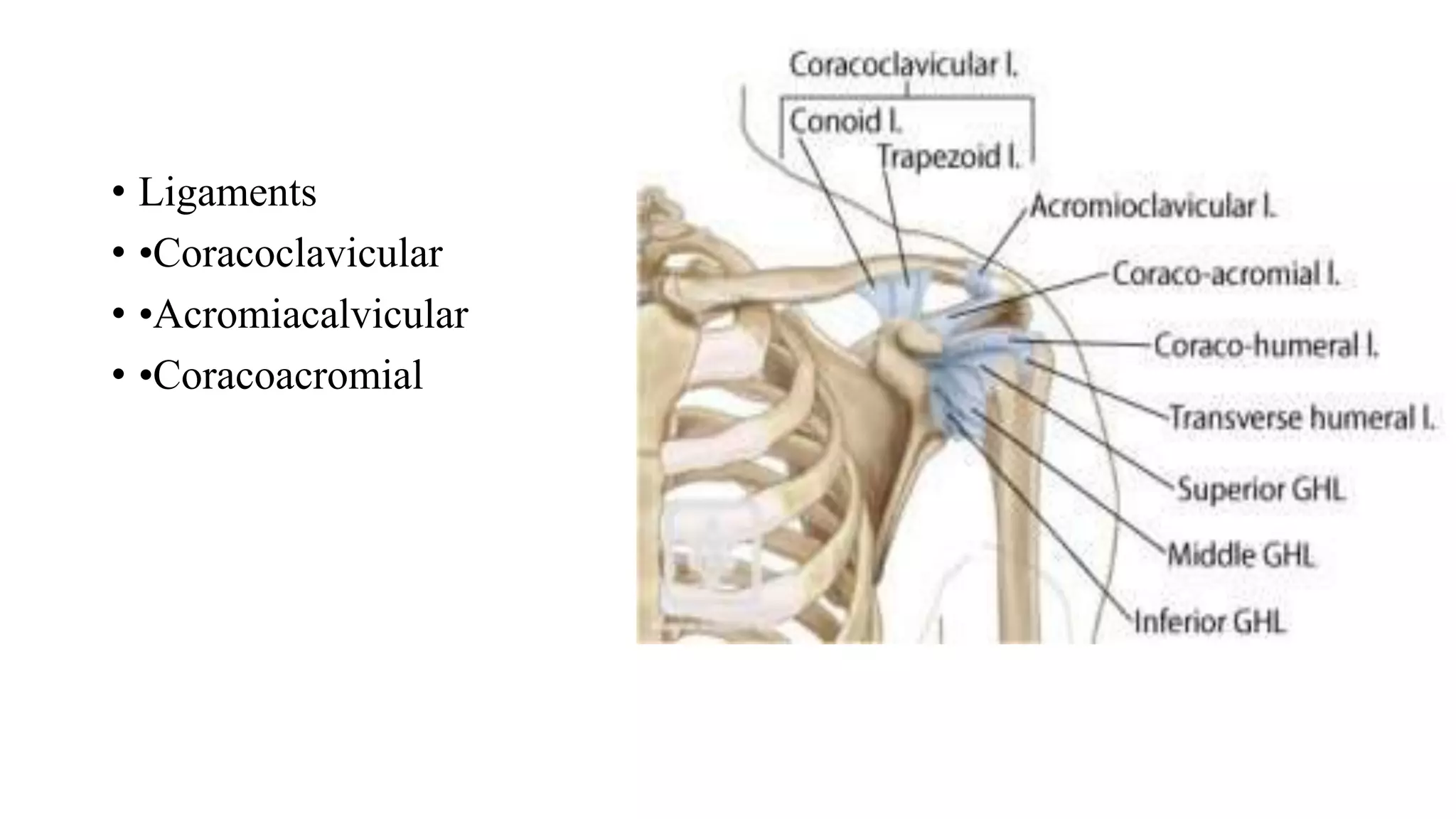
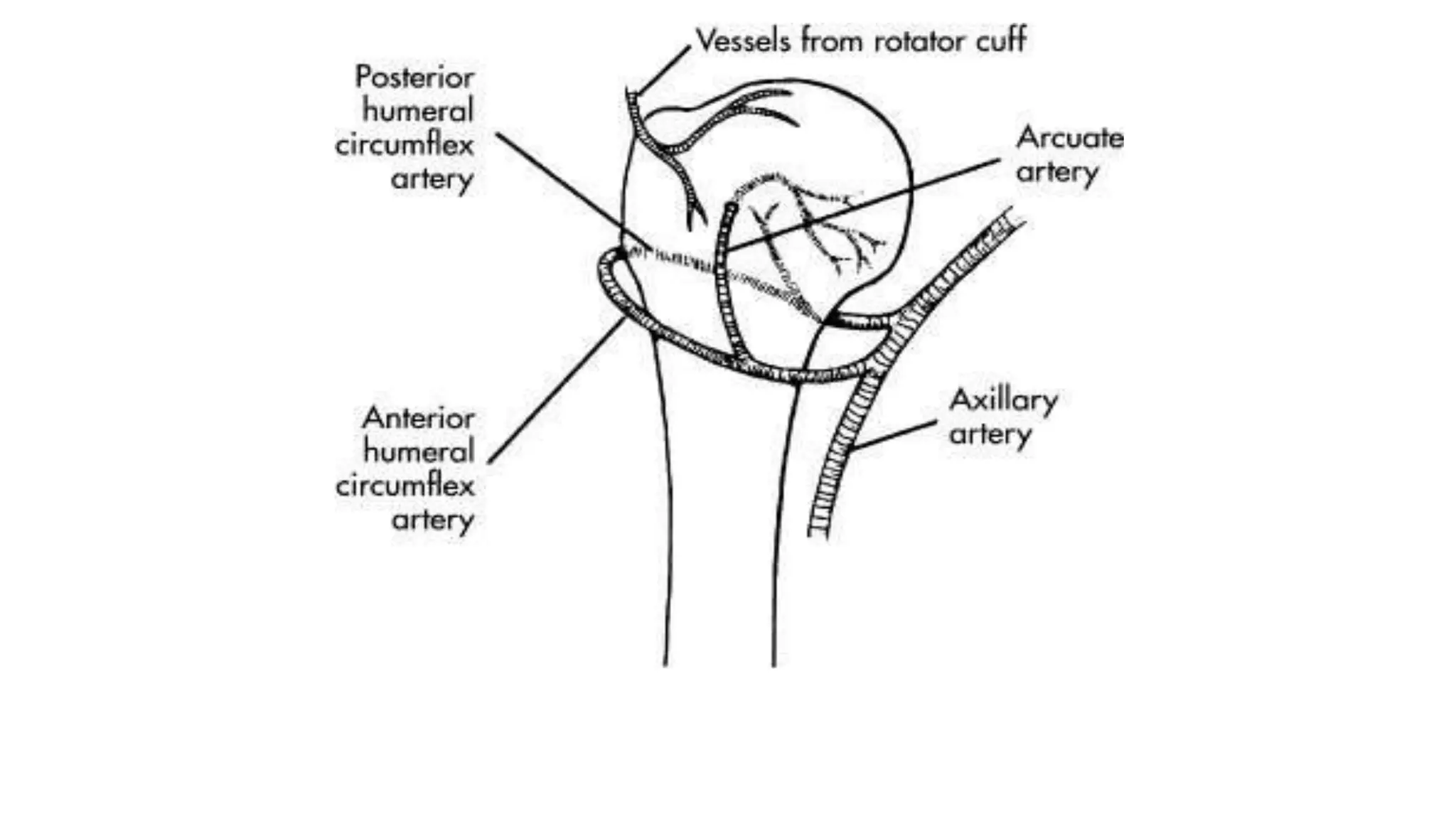
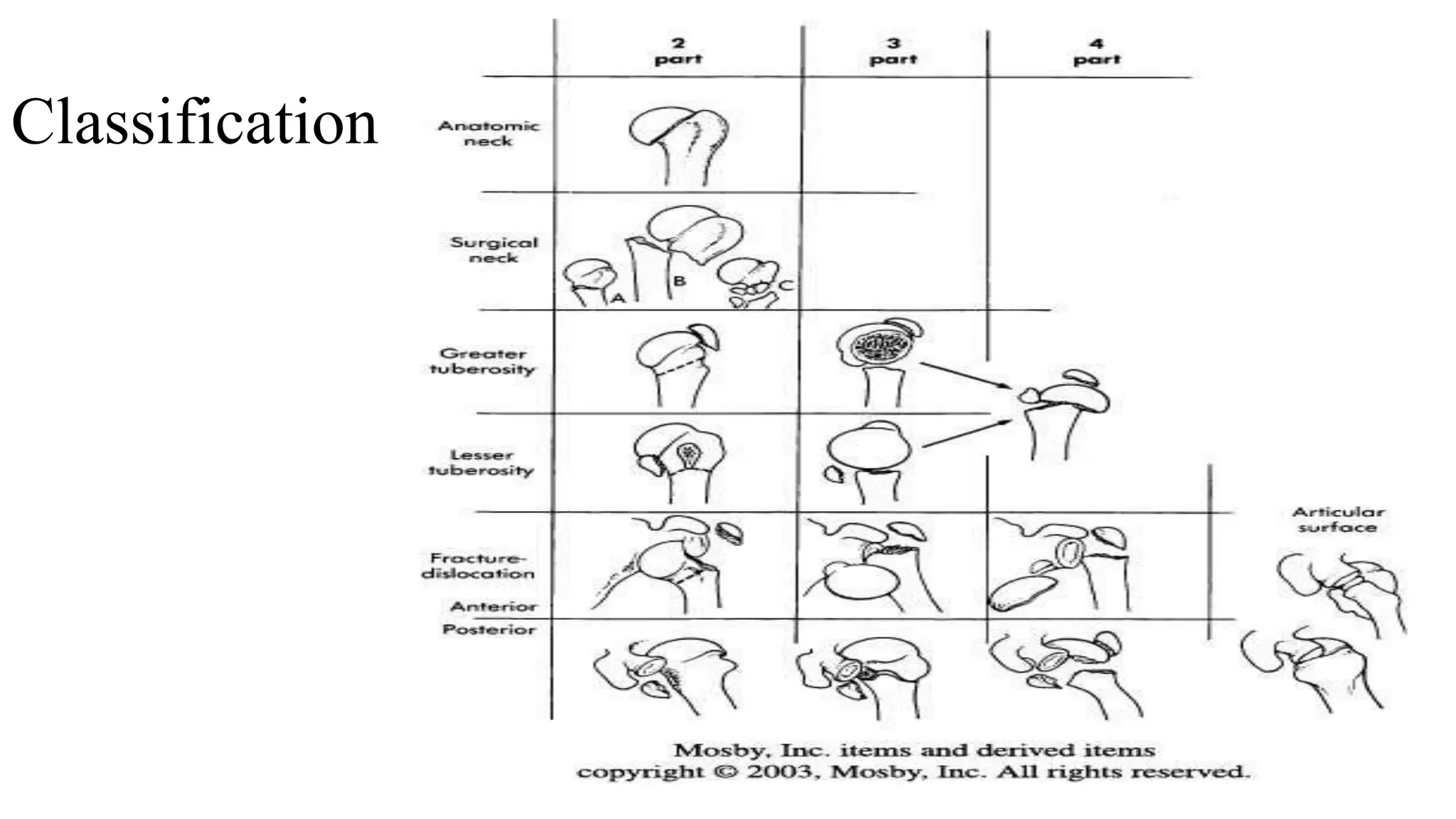
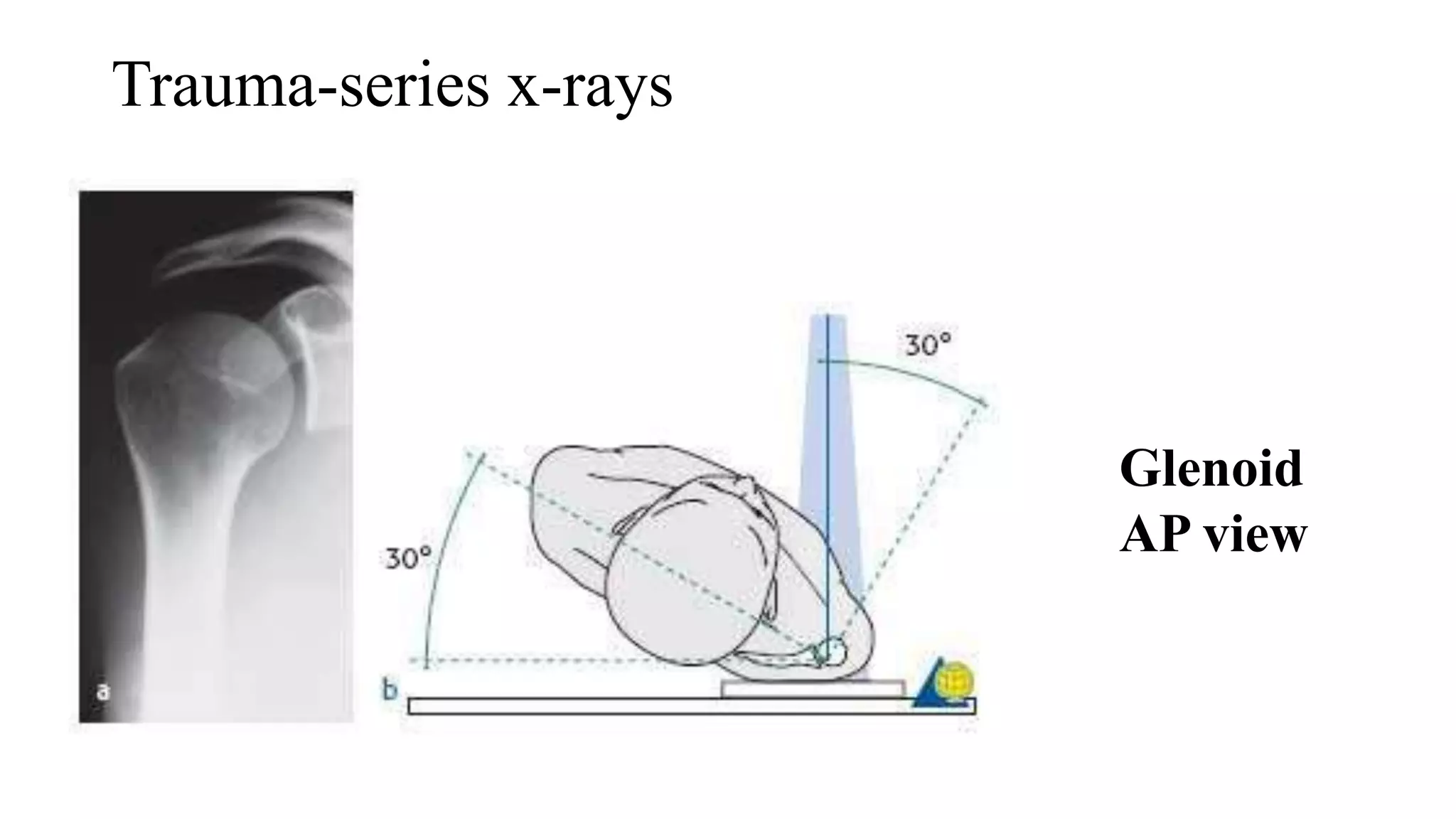
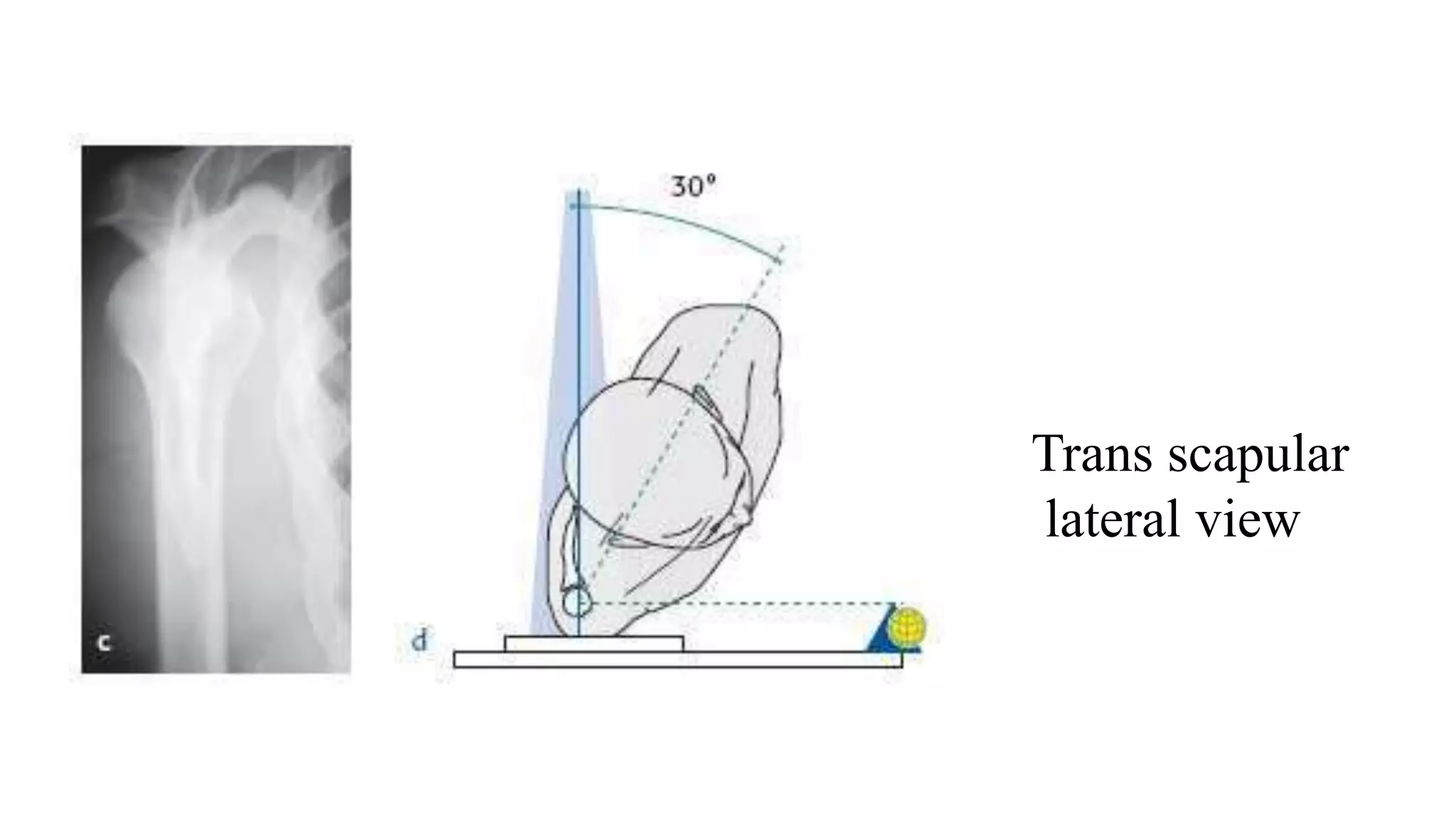
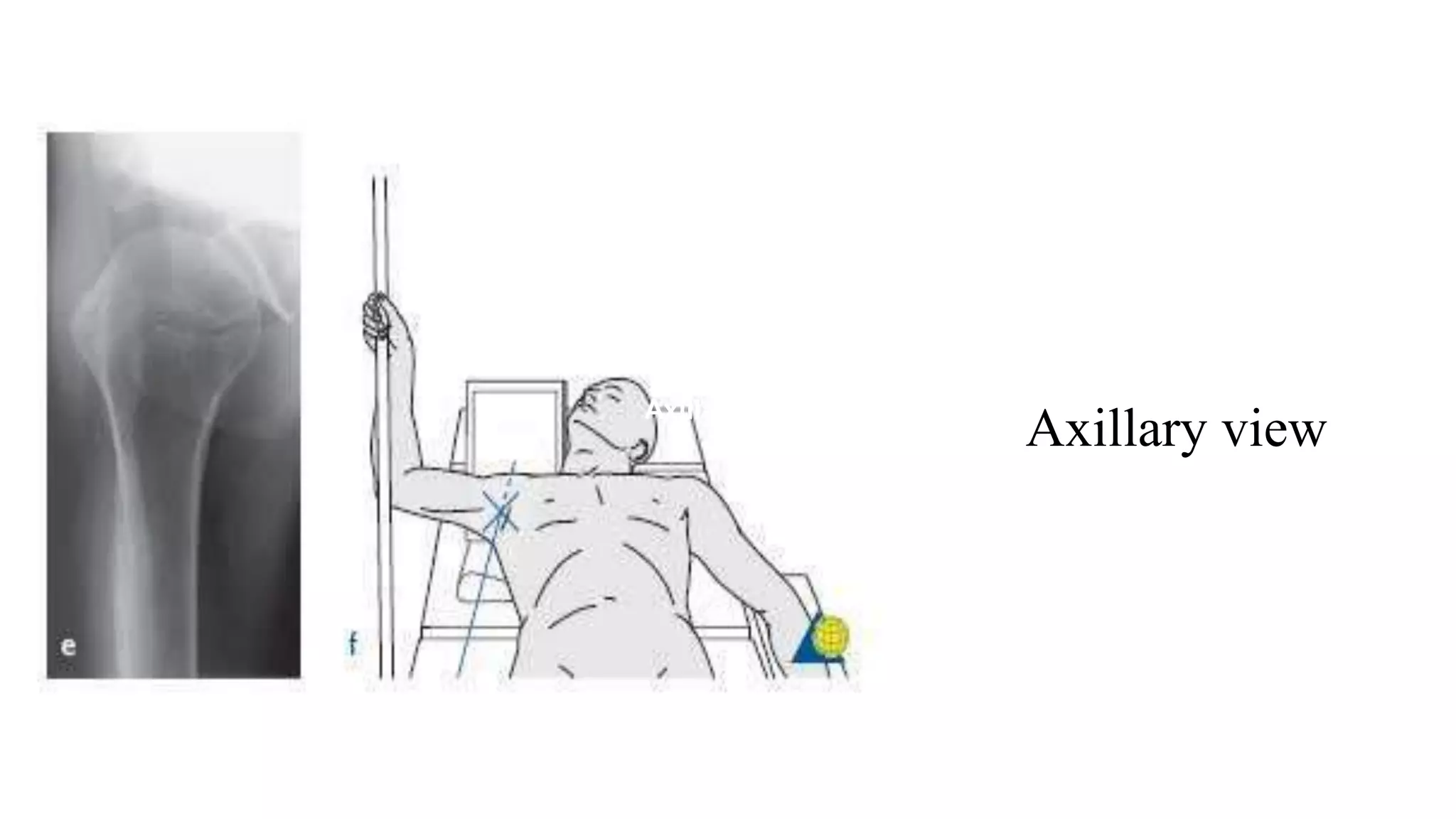
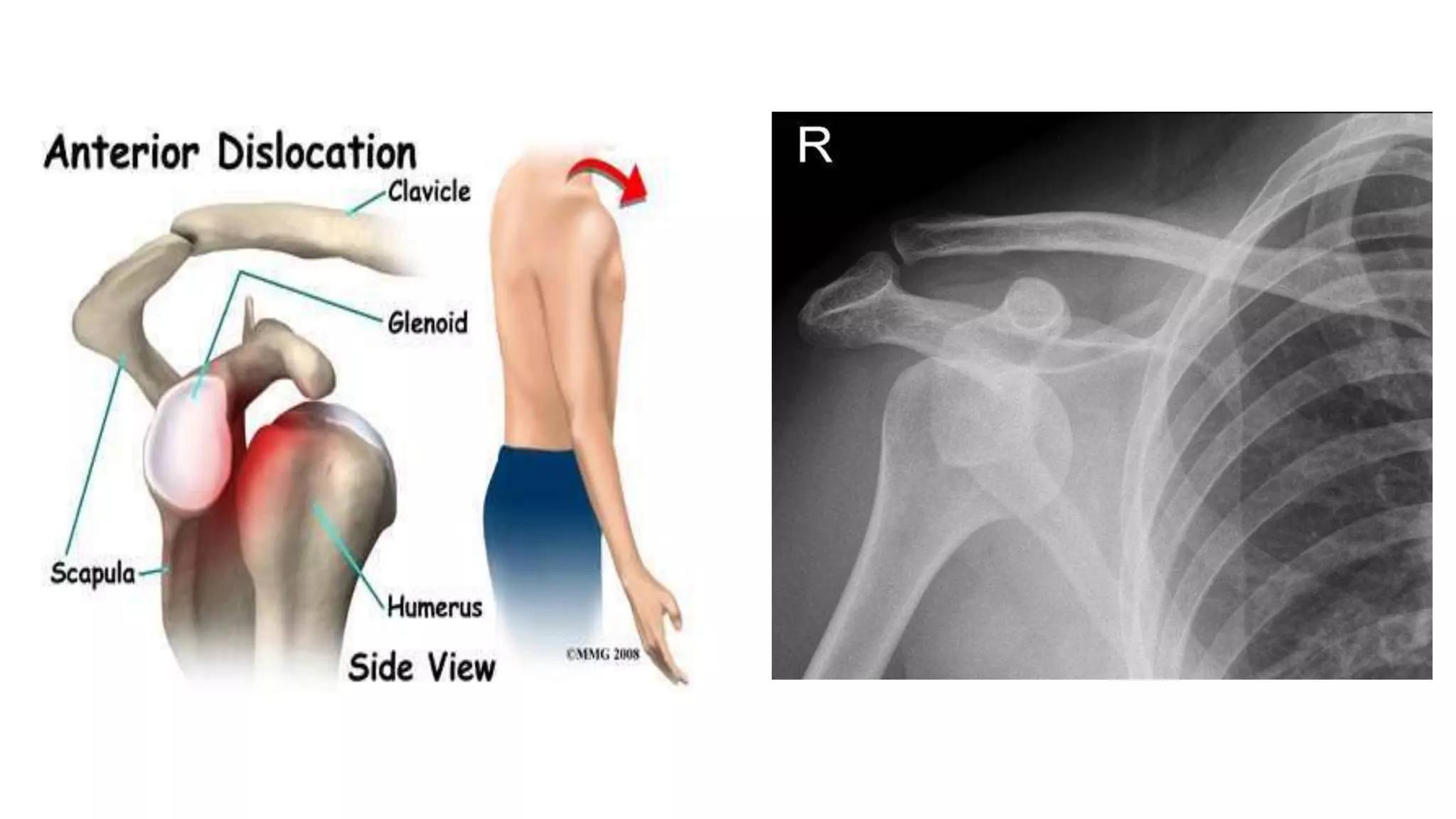
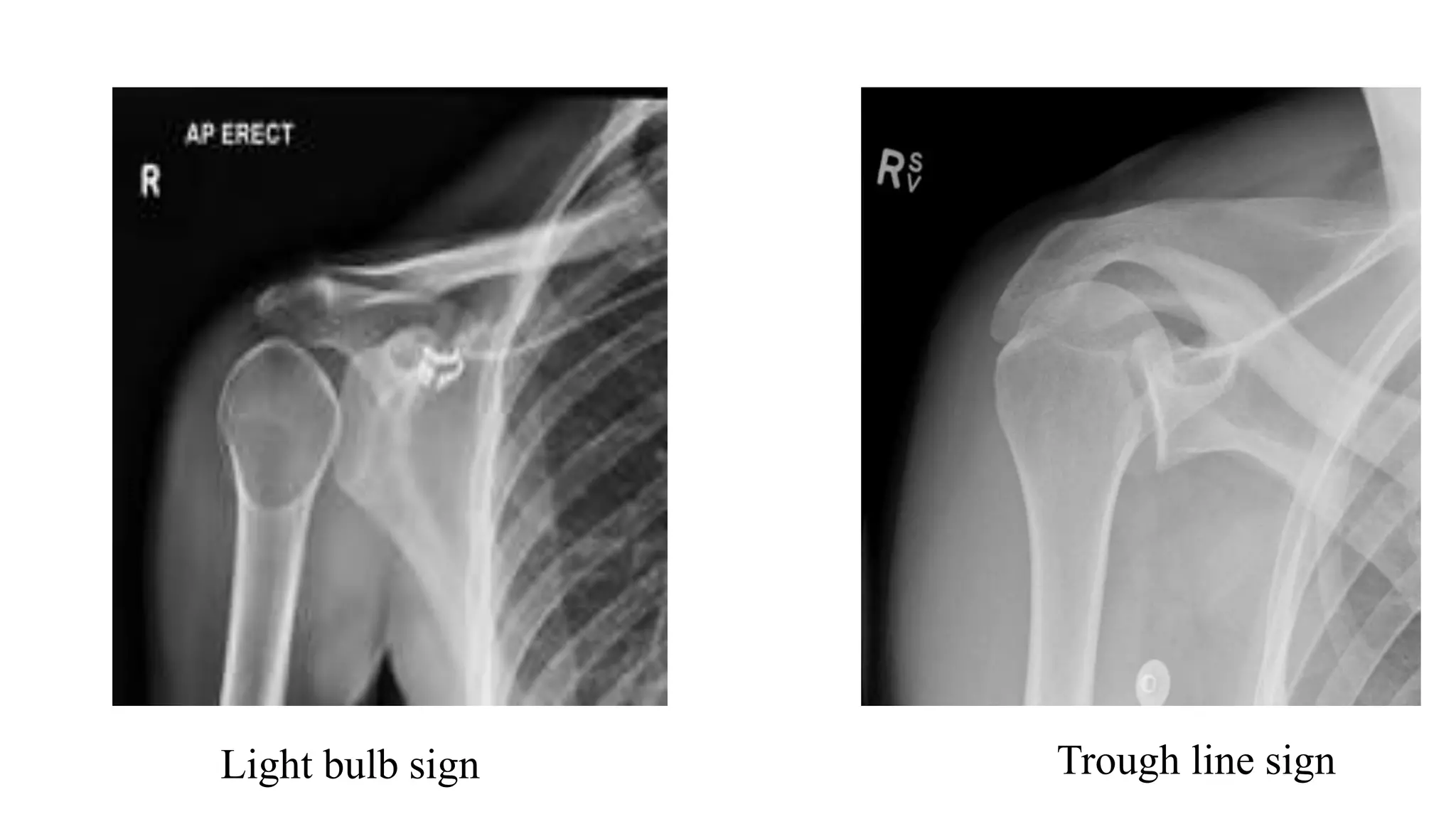
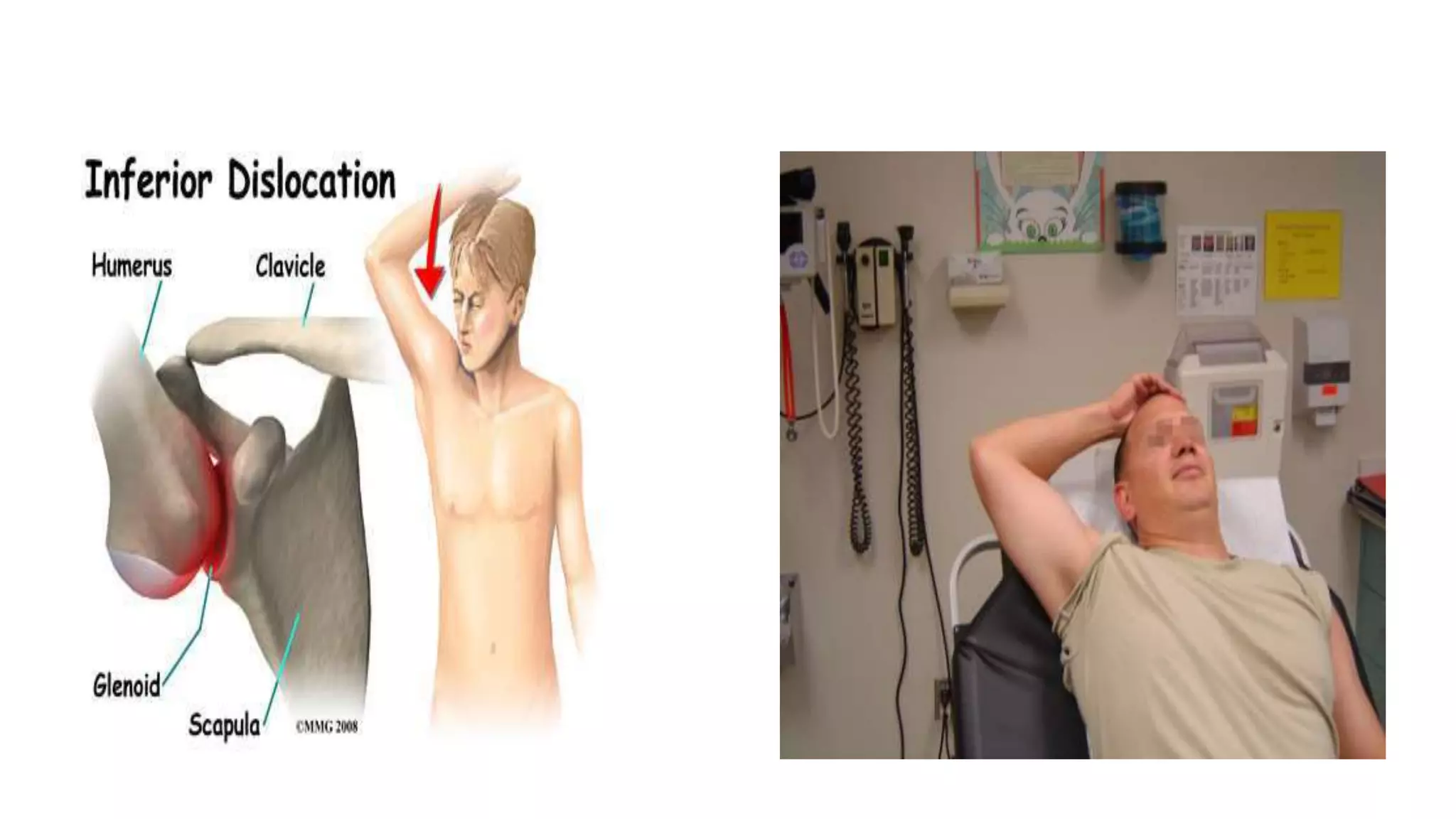
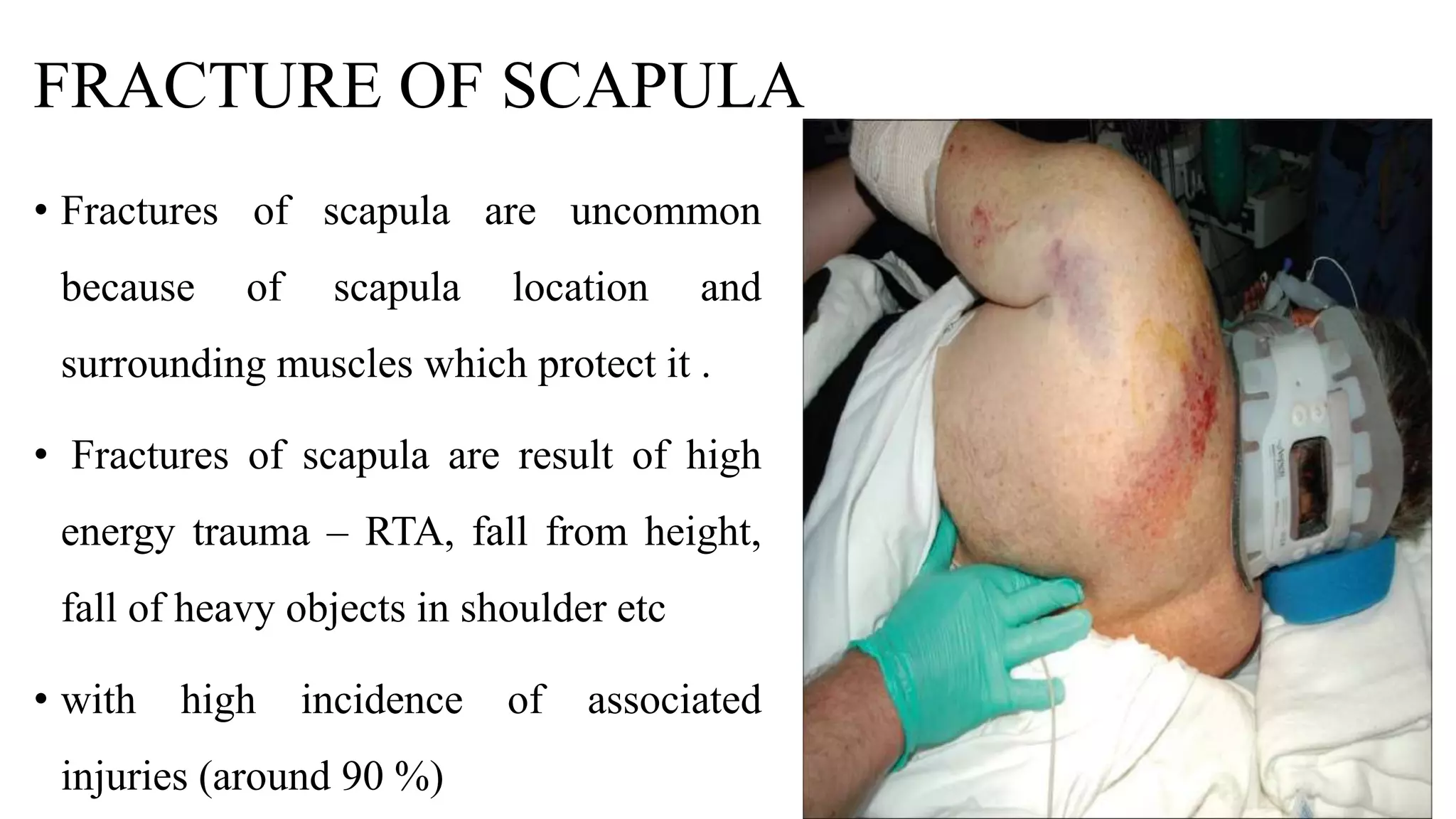
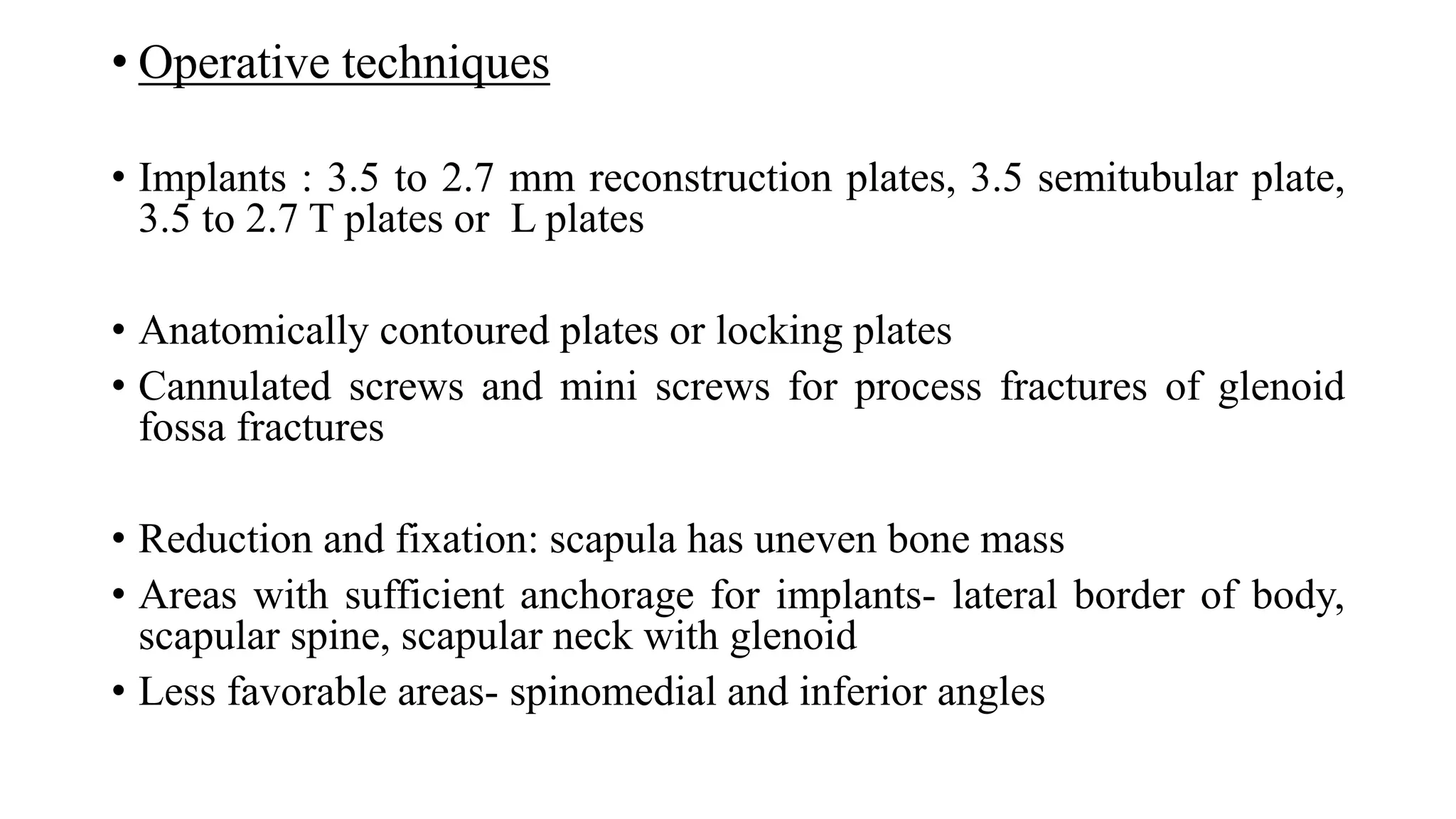
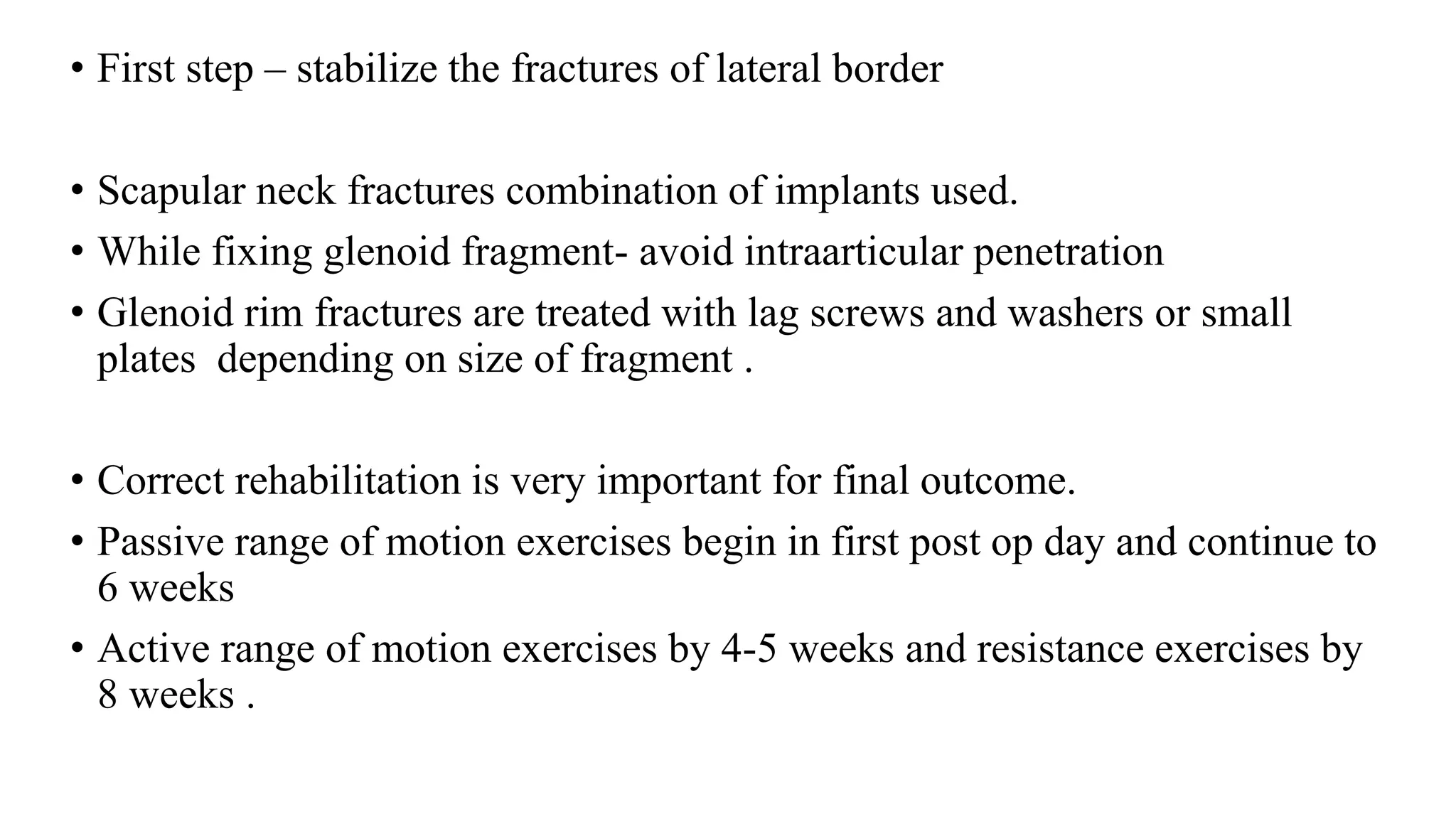
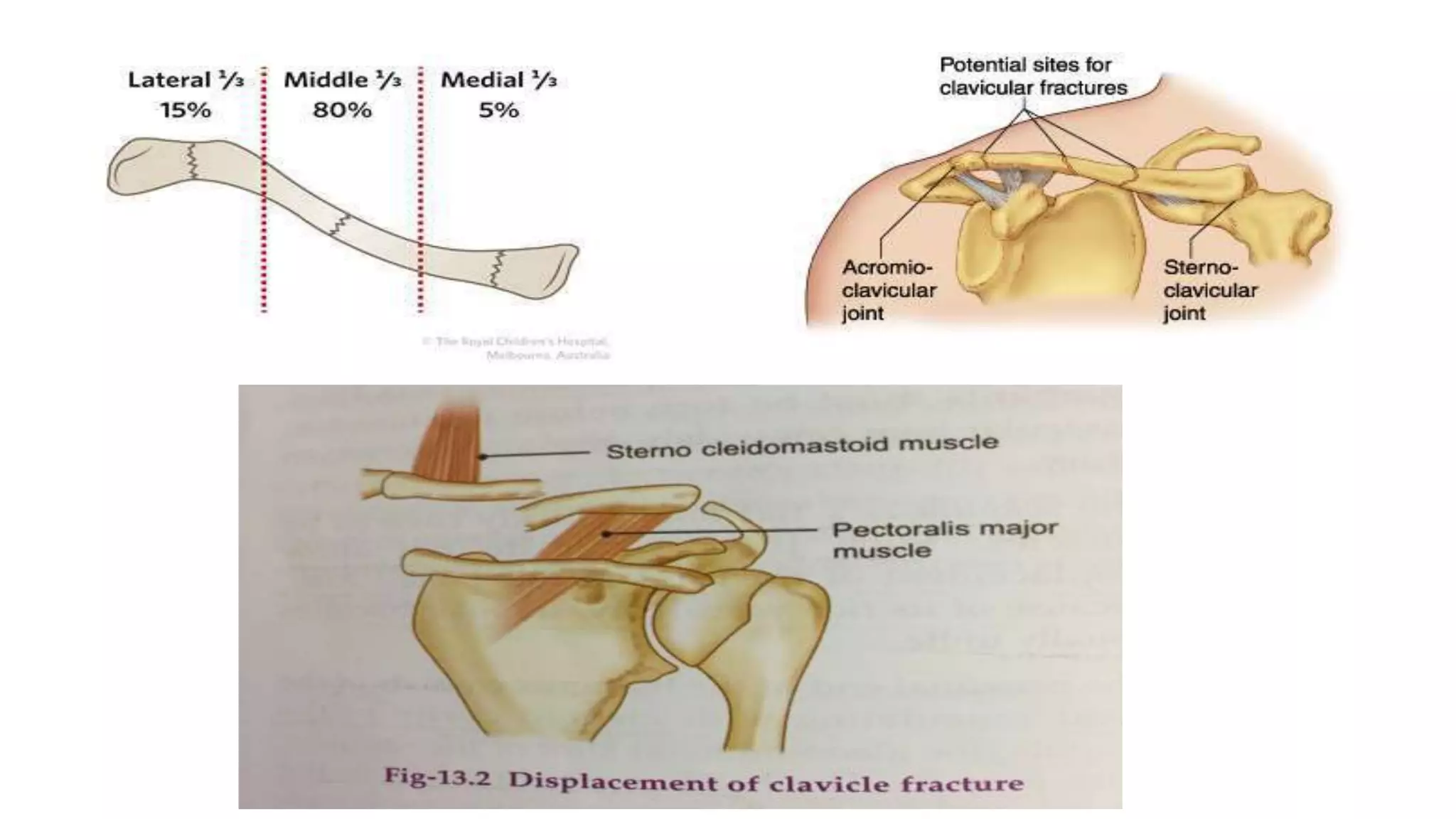
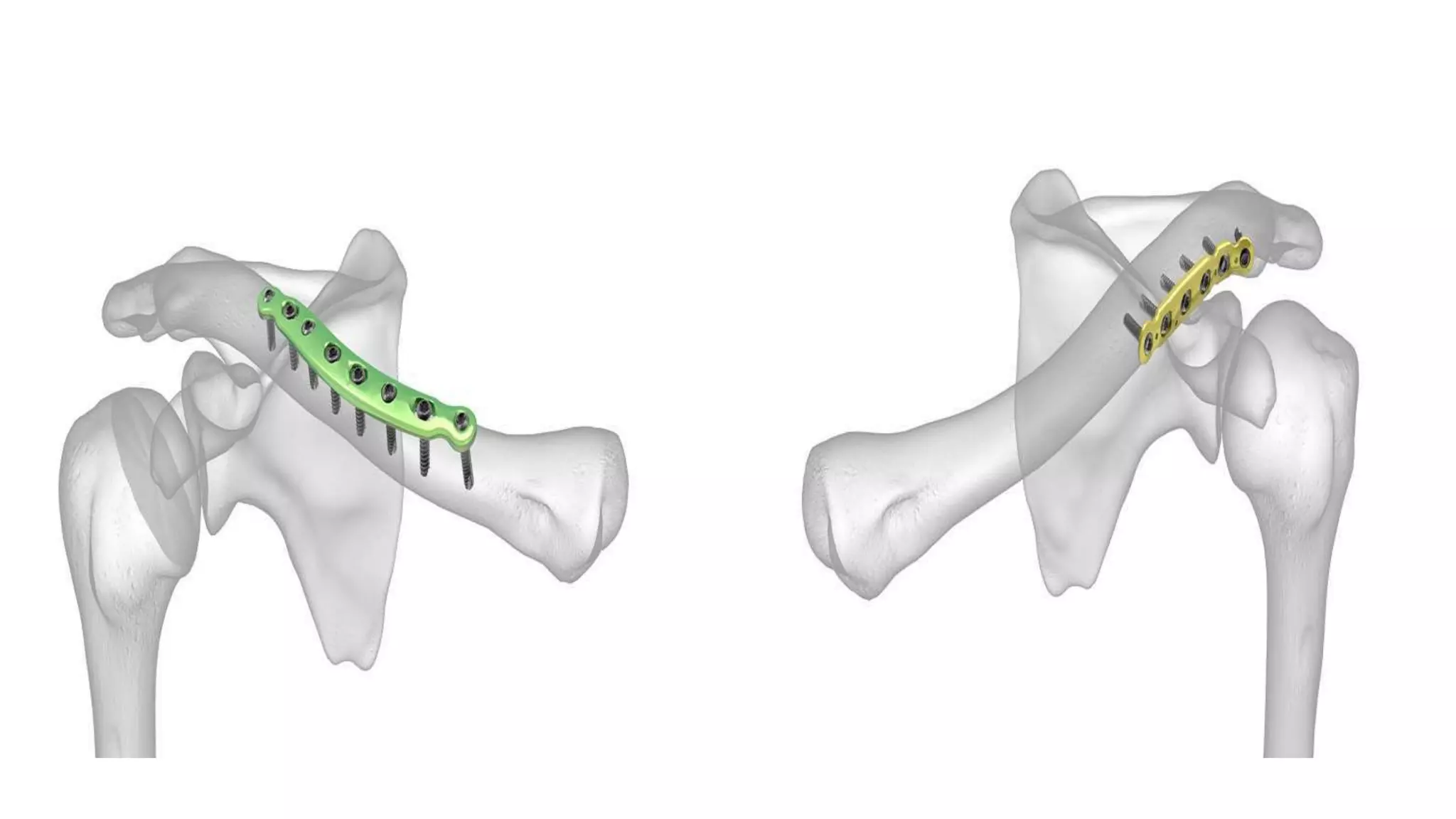
This document discusses fractures around the shoulder joint, including proximal humerus fractures, shoulder dislocations, scapular fractures, and clavicular fractures. It provides details on the anatomy, classifications, clinical presentations, imaging, and treatment options for each type of injury. Treatment may involve closed reduction, open reduction with various surgical techniques like plating or nailing depending on the fracture pattern and bone quality. Post-operative rehabilitation is important for optimal outcomes.