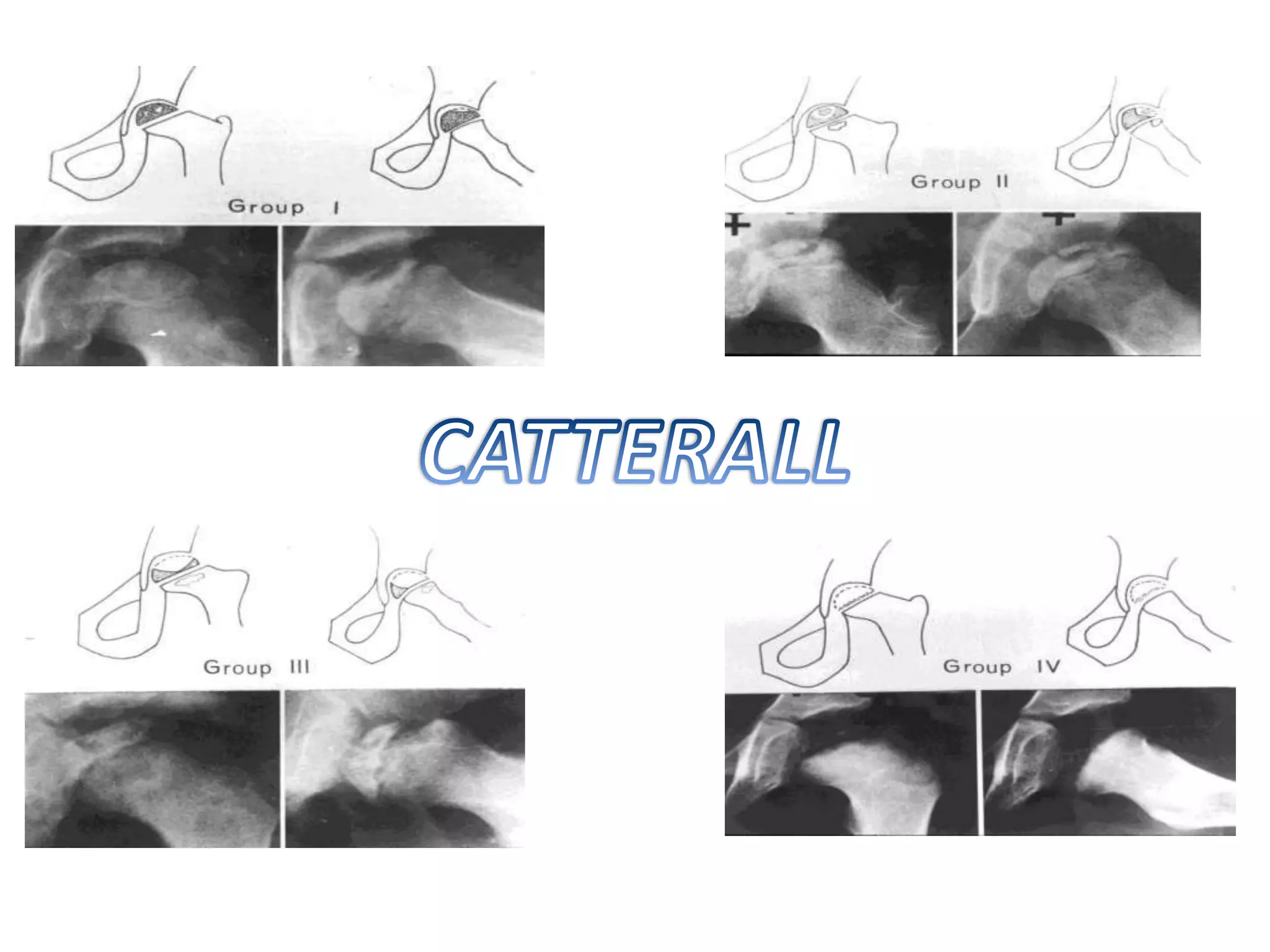
This document provides an overview of Legg Calve Perthes disease, including its definition, demographics, risk factors, pathogenesis, clinical features, investigations, classifications, management, and surgical procedures. Some key points:
- It is avascular necrosis of the femoral head in children, most common in ages 4-8 years. Positive family history and low birth weight are risk factors.
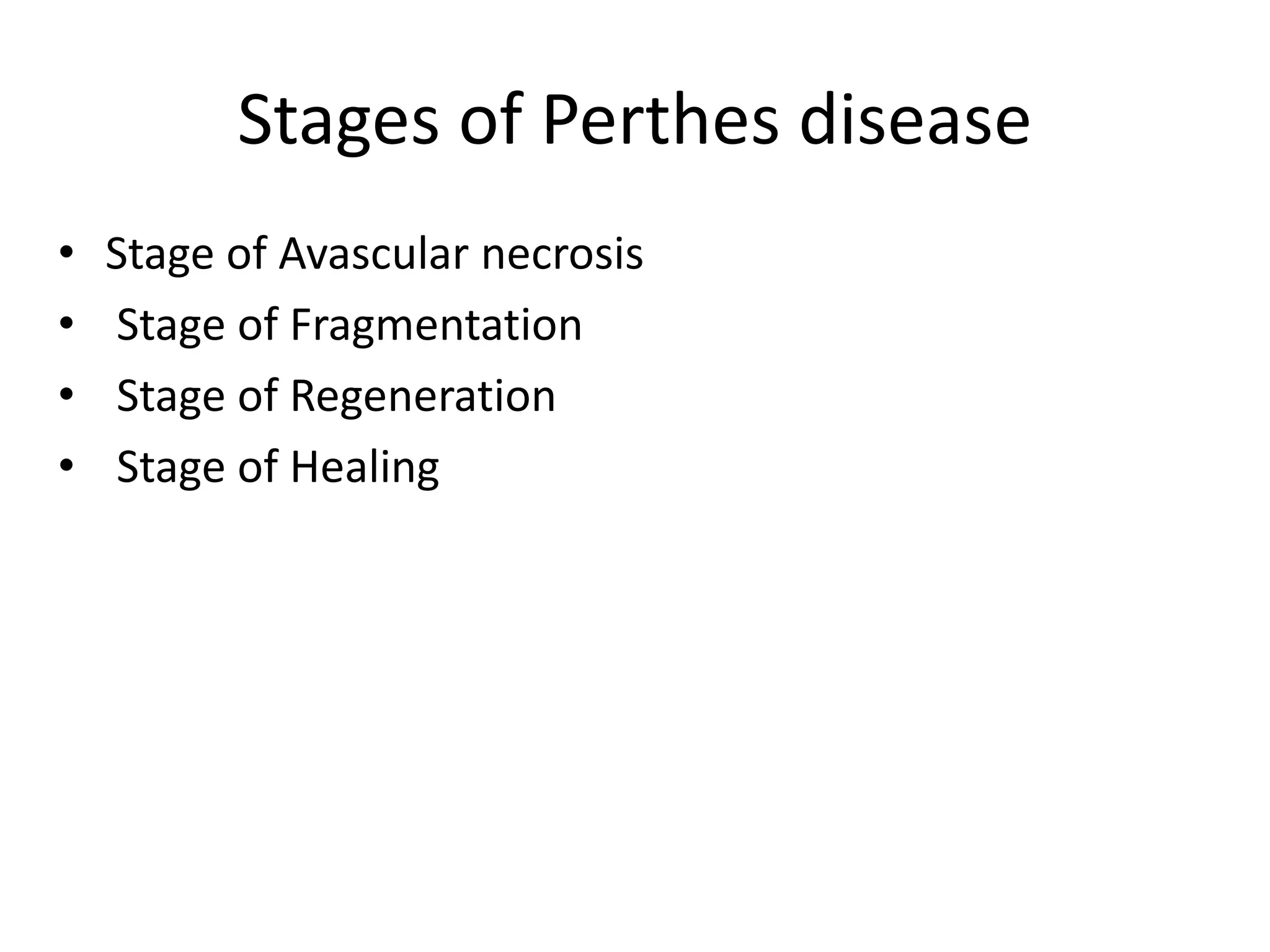
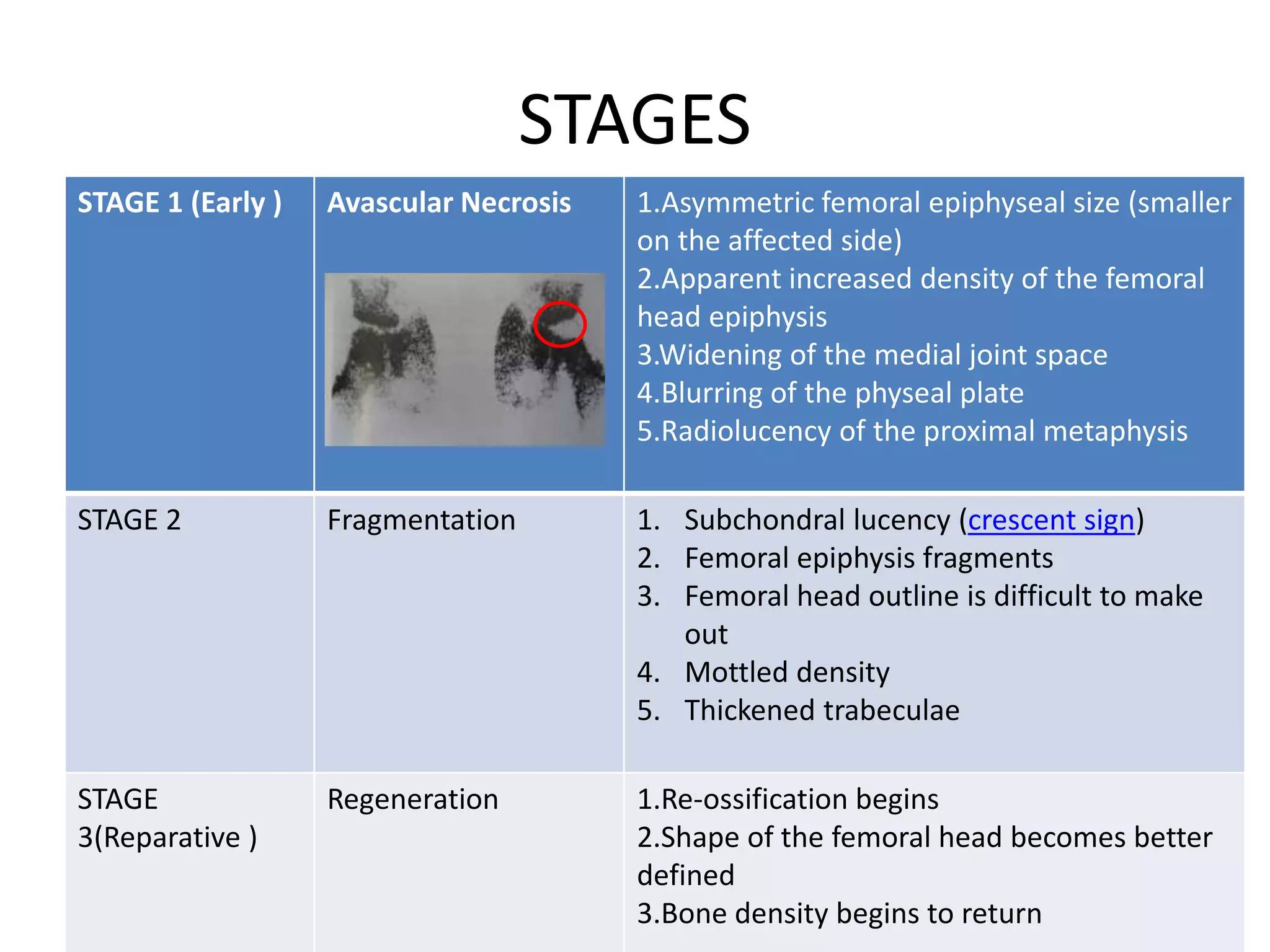
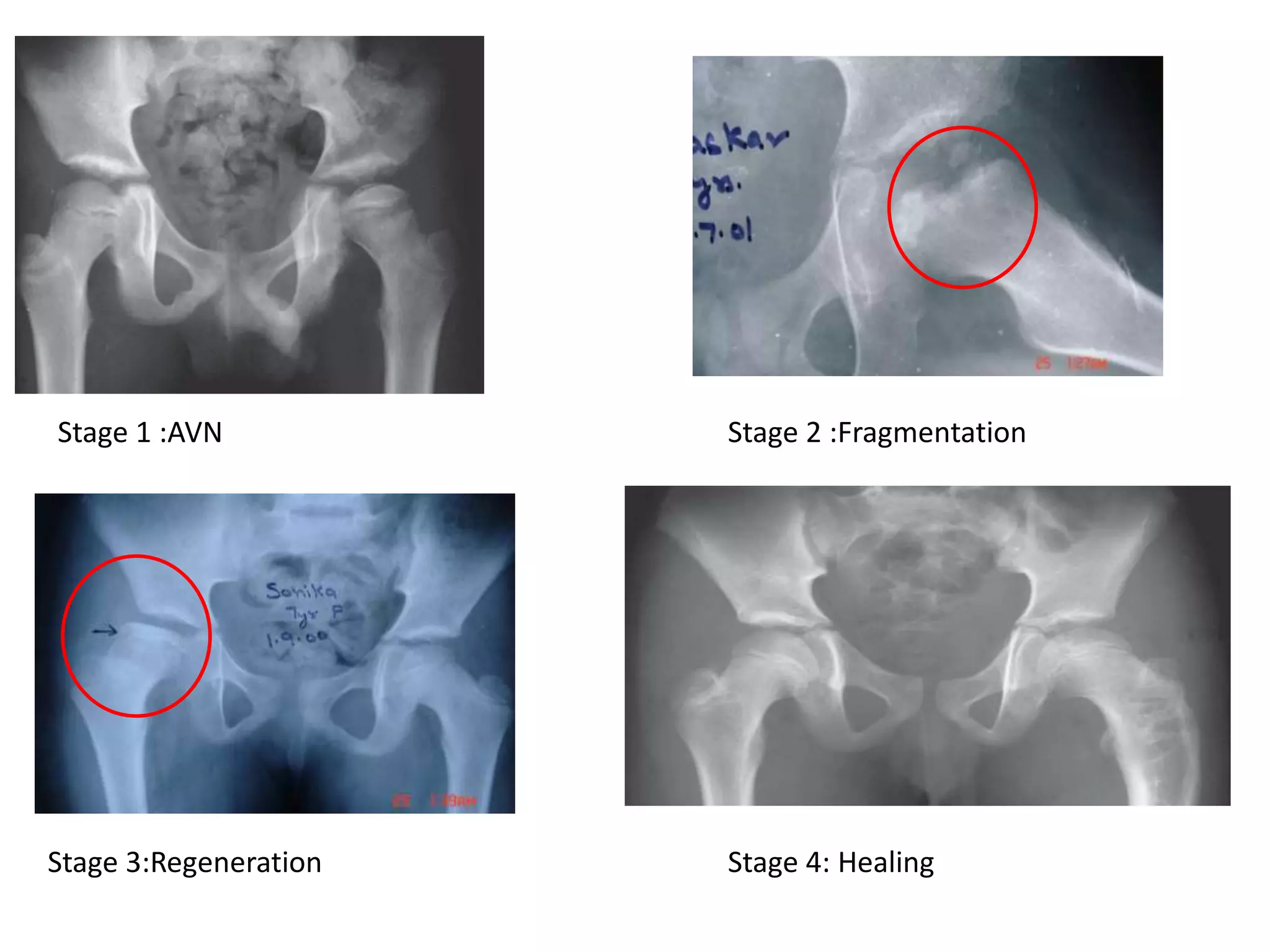
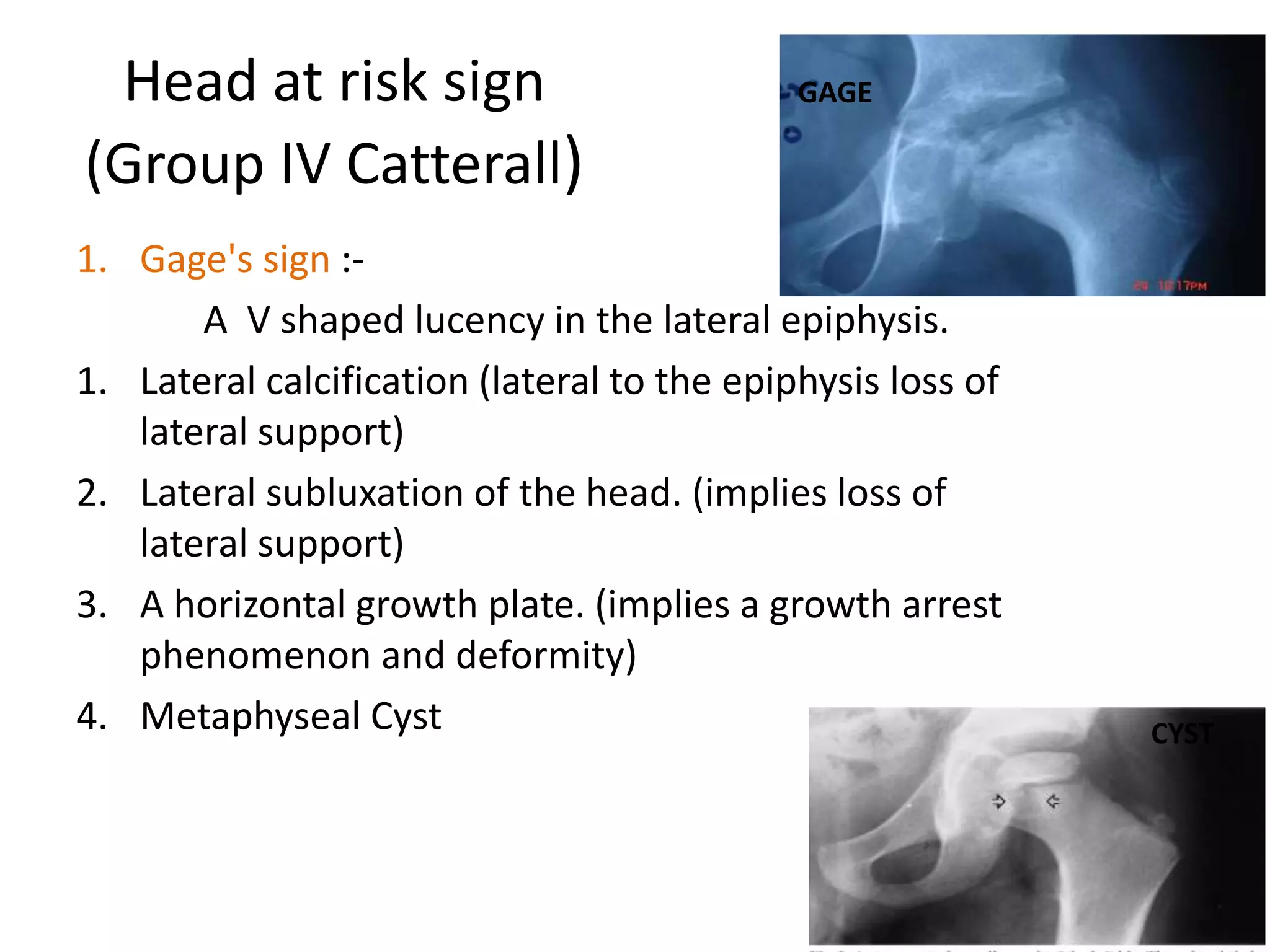
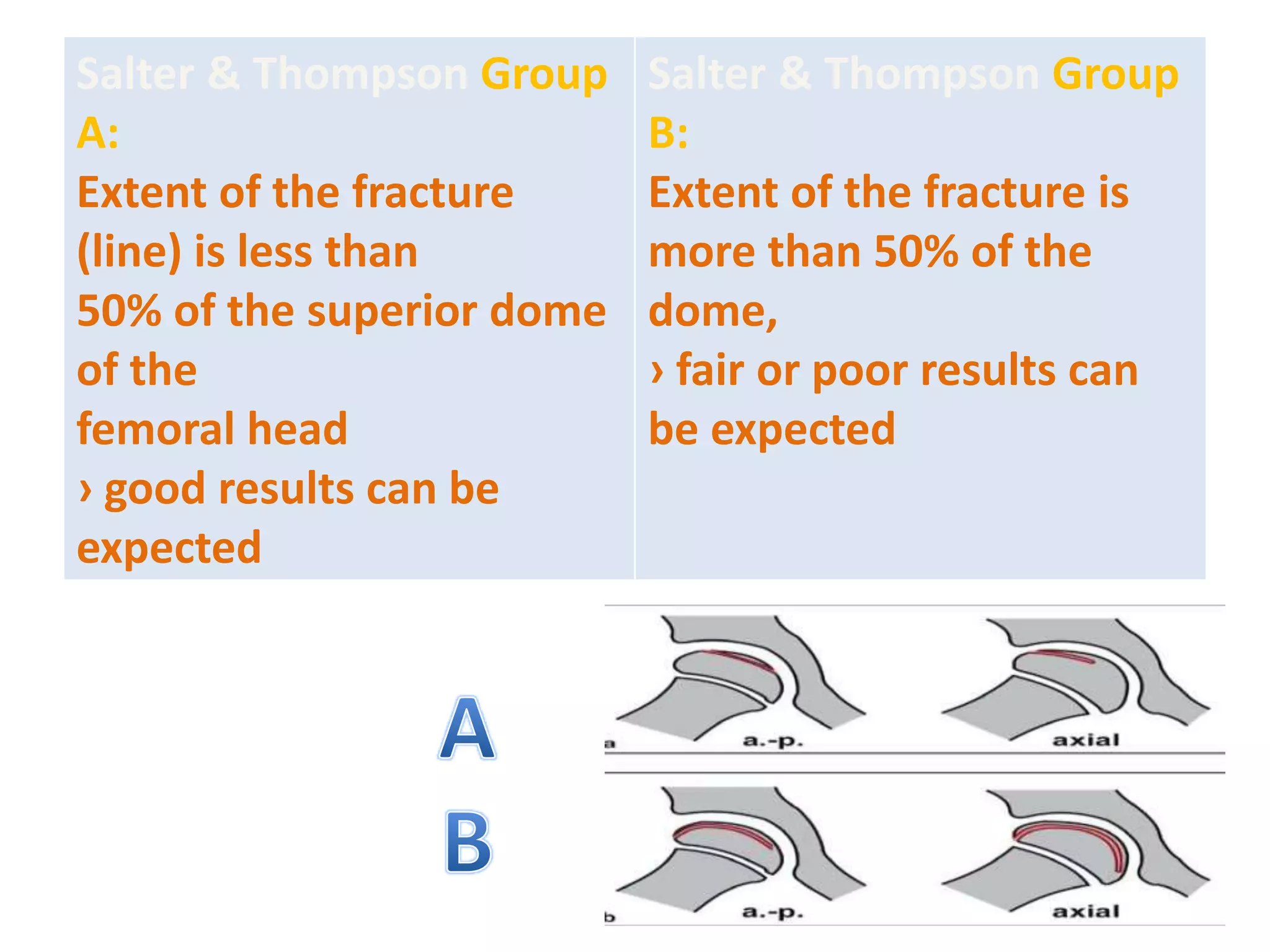
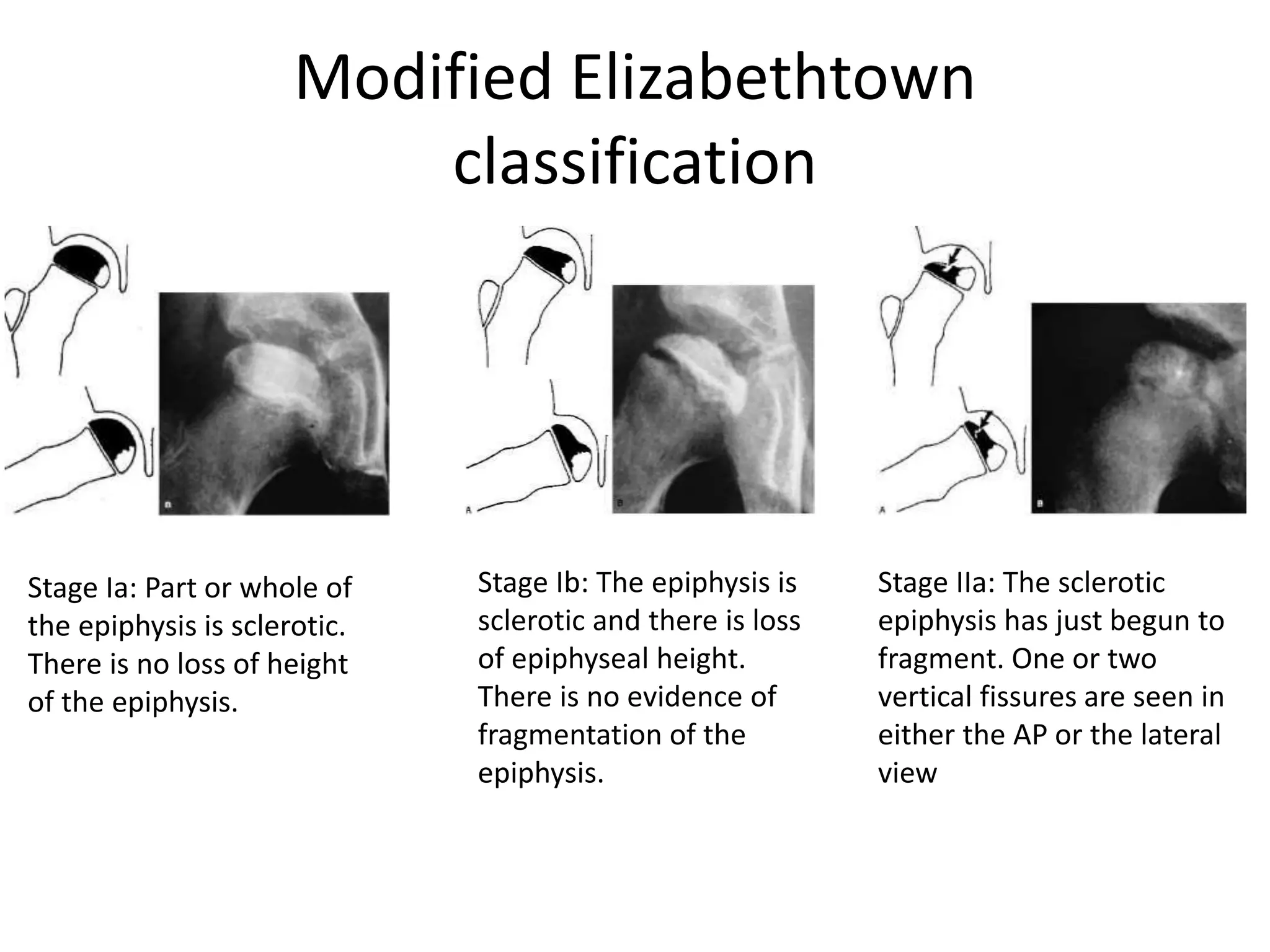
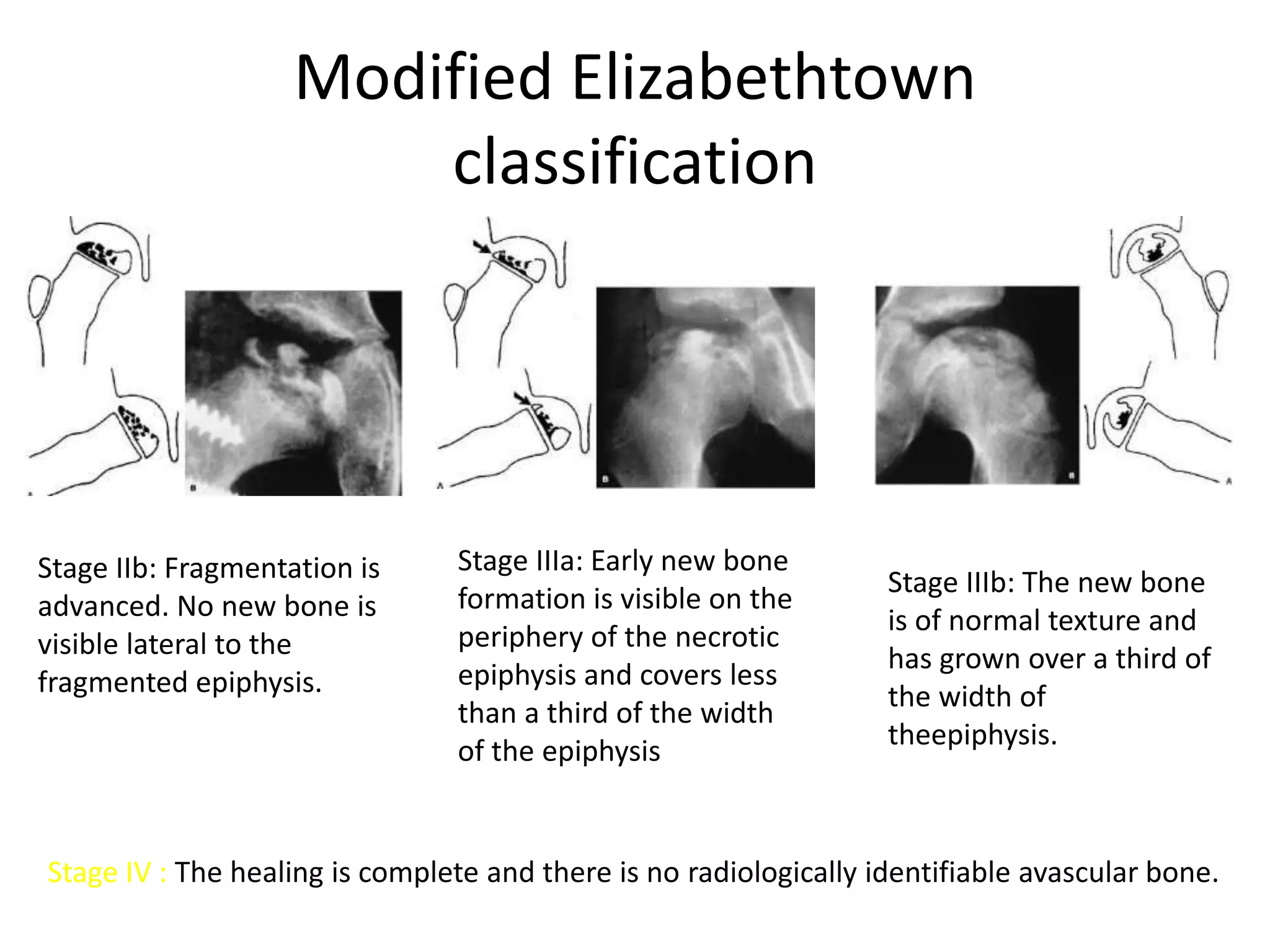
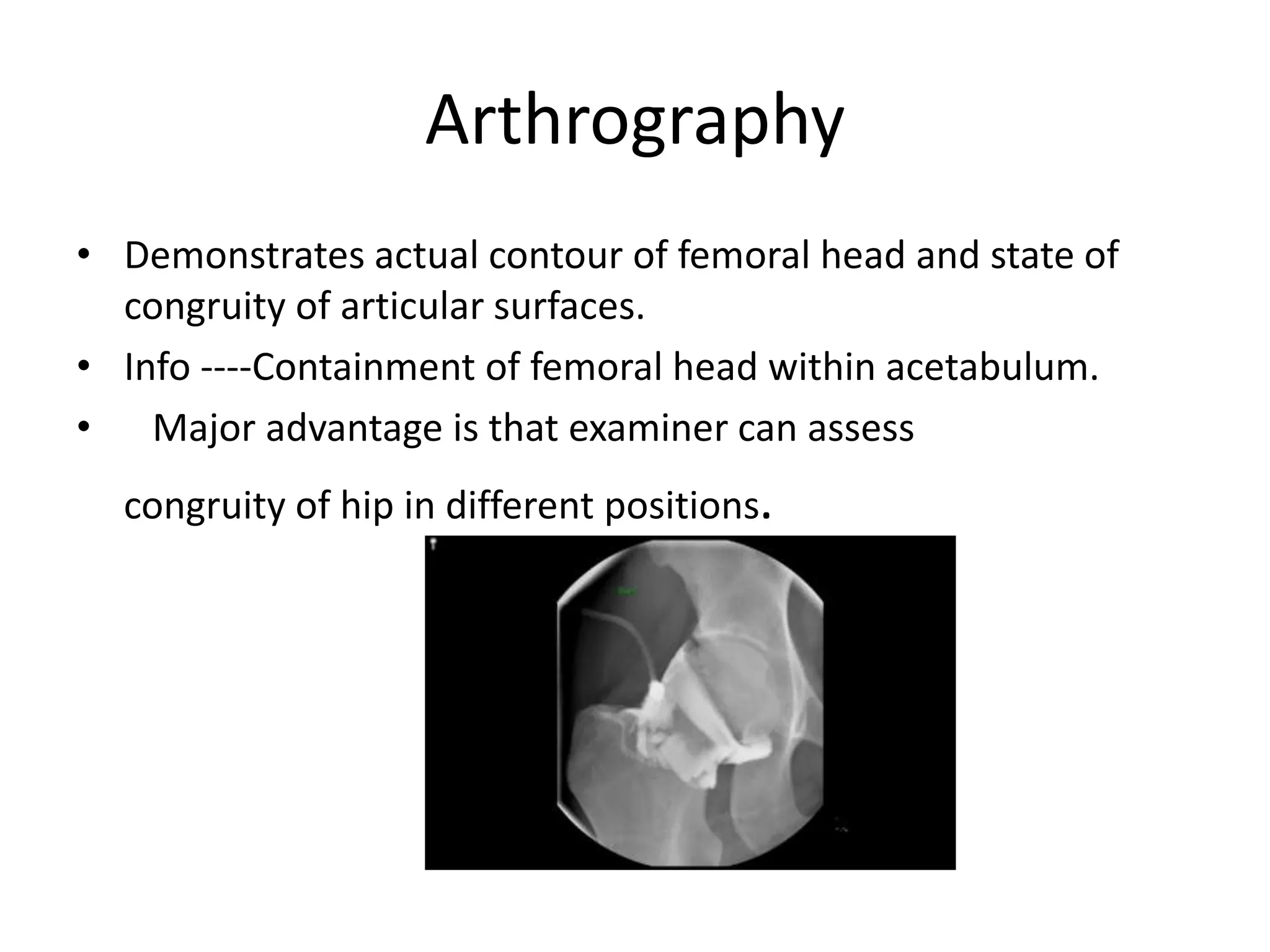
- Clinical features include hip/thigh pain aggravated by movement. Imaging shows stages from avascular necrosis to fragmentation to regeneration/healing.
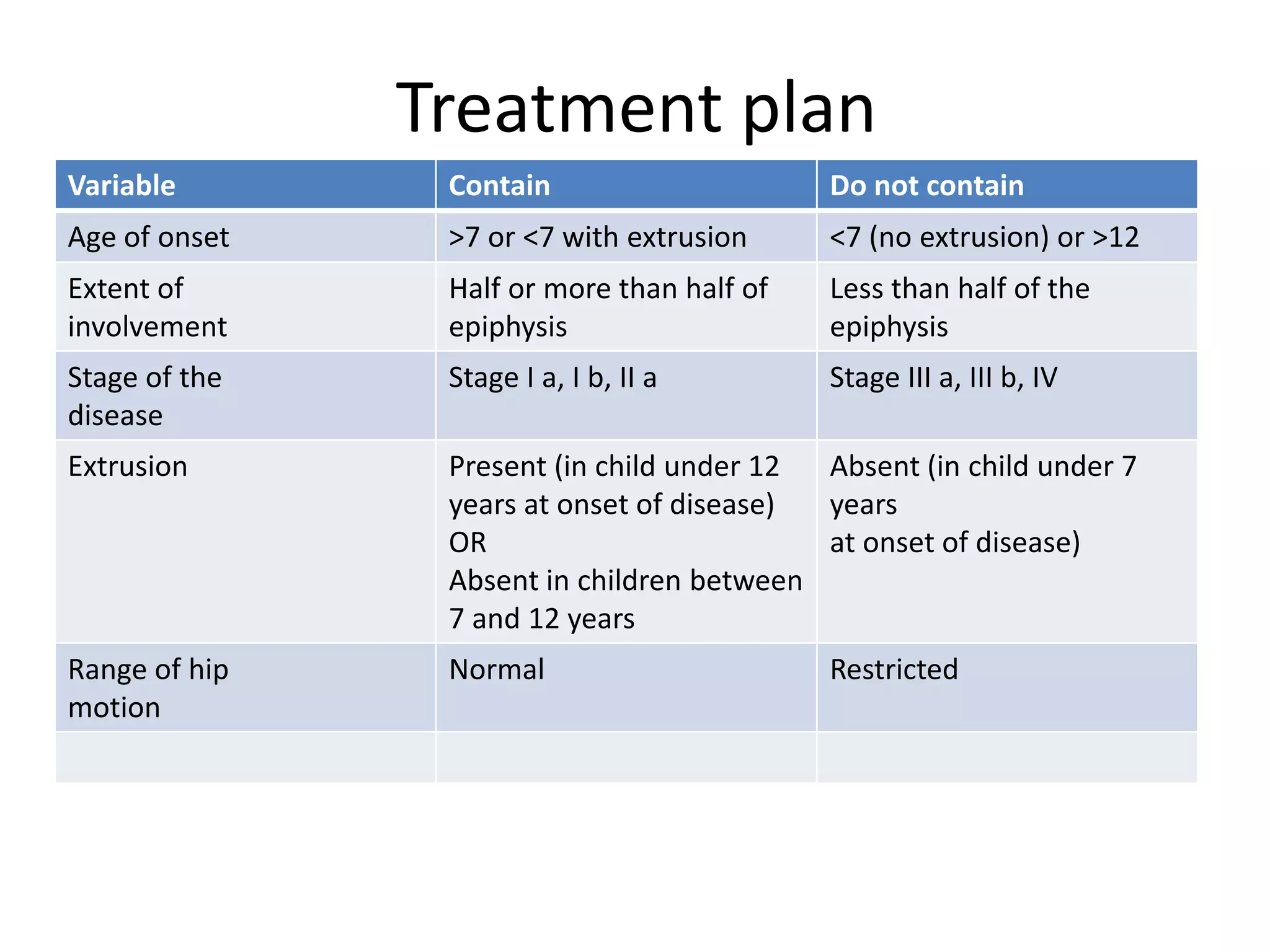
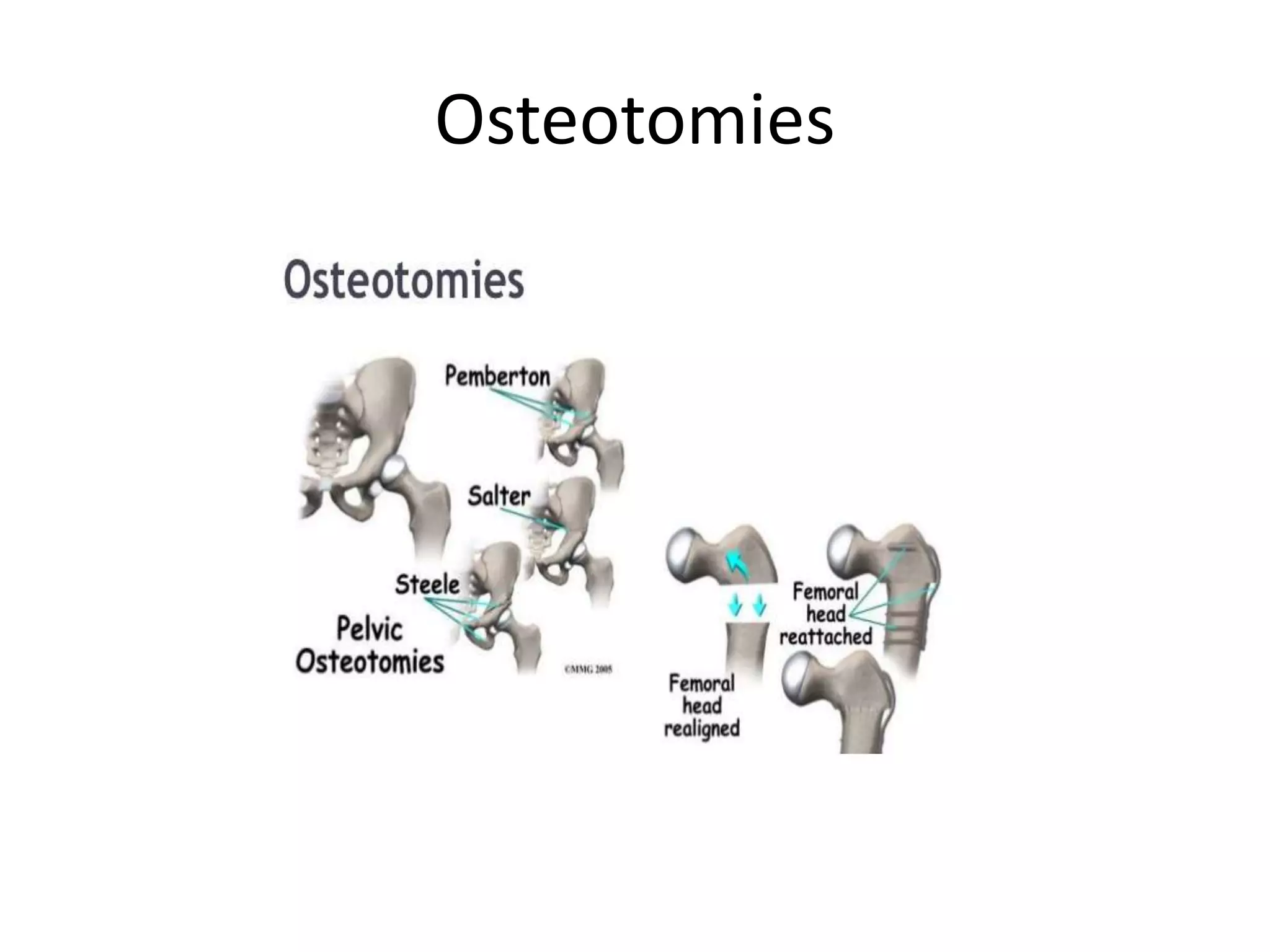
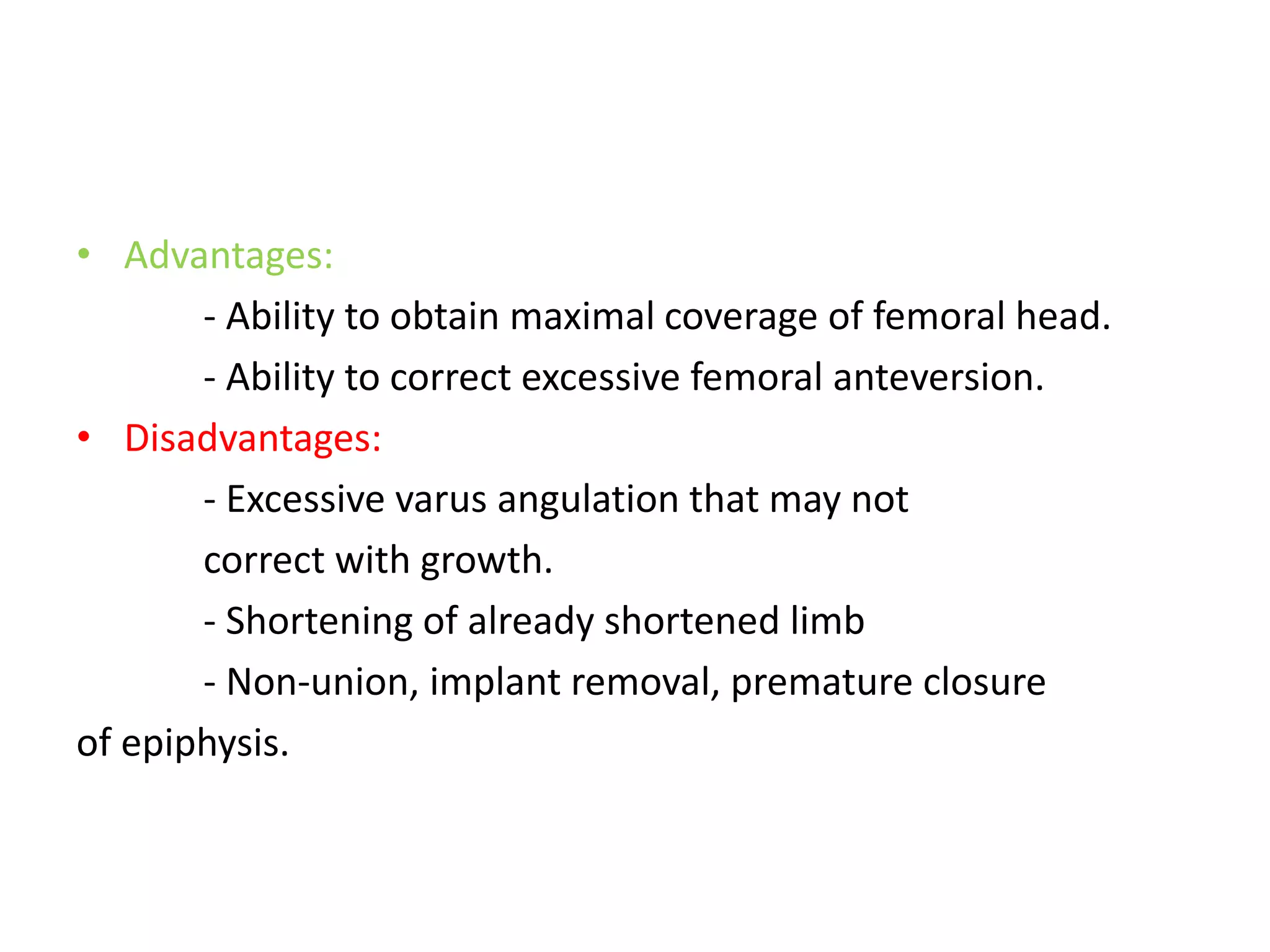
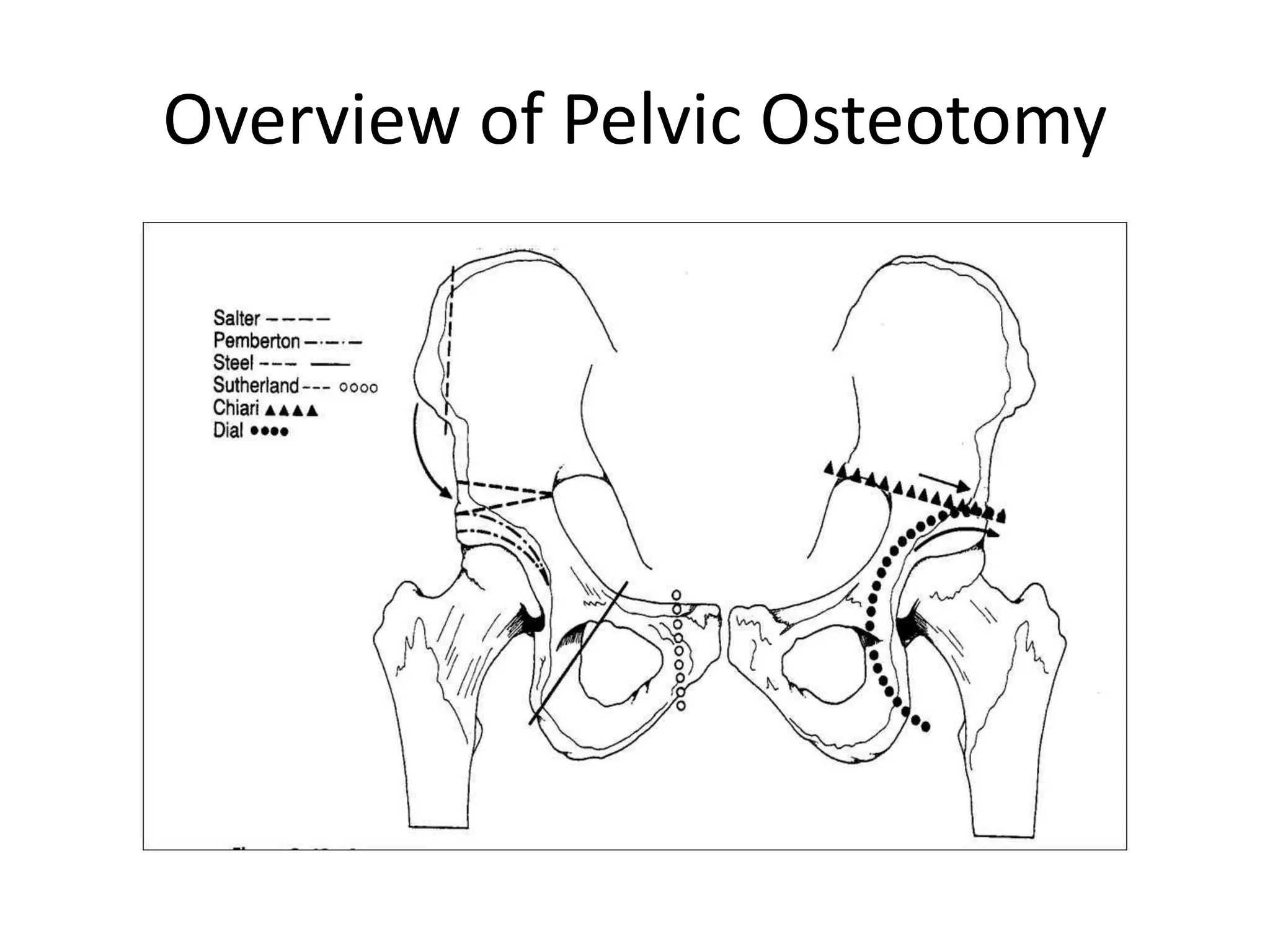
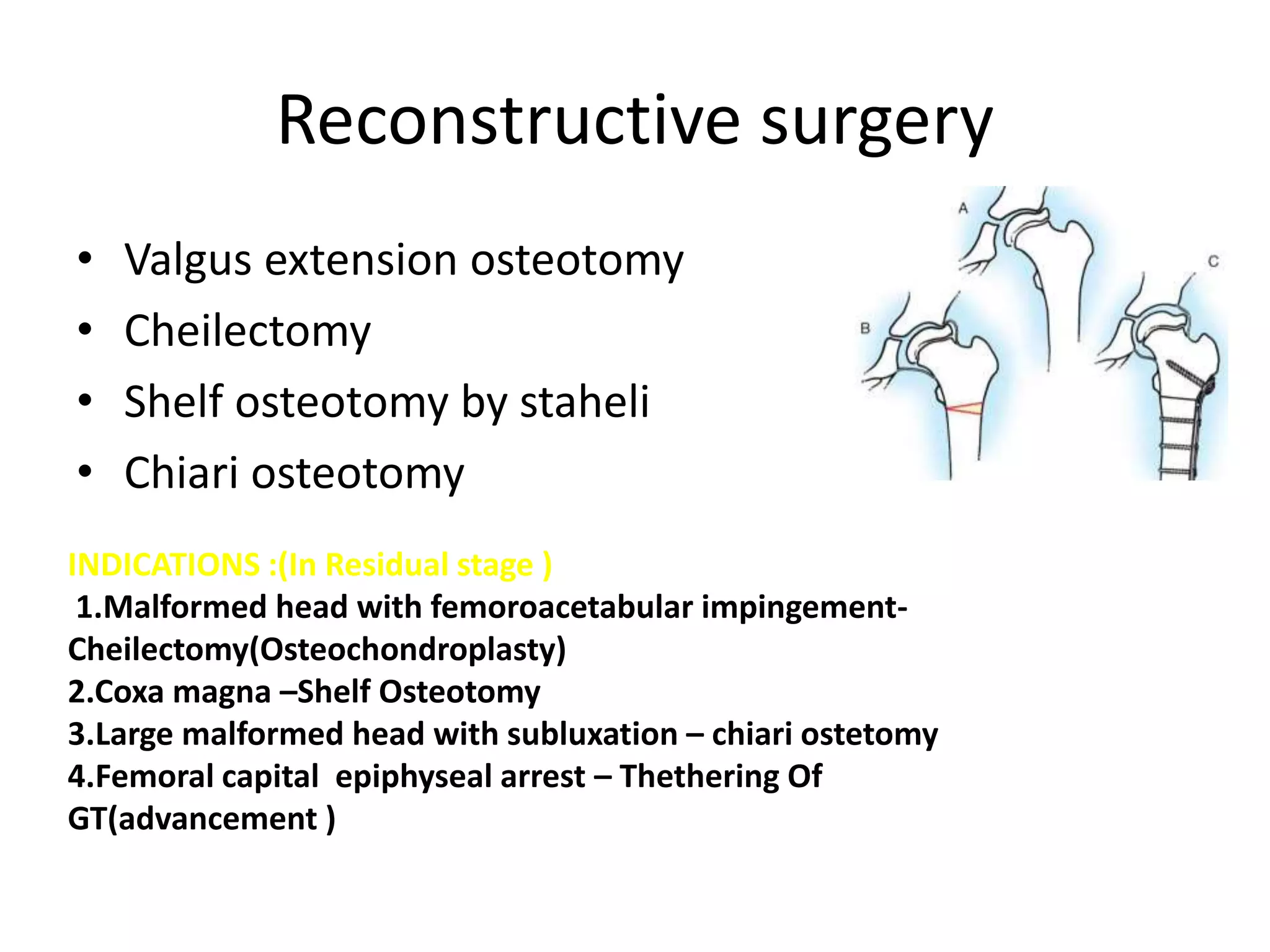
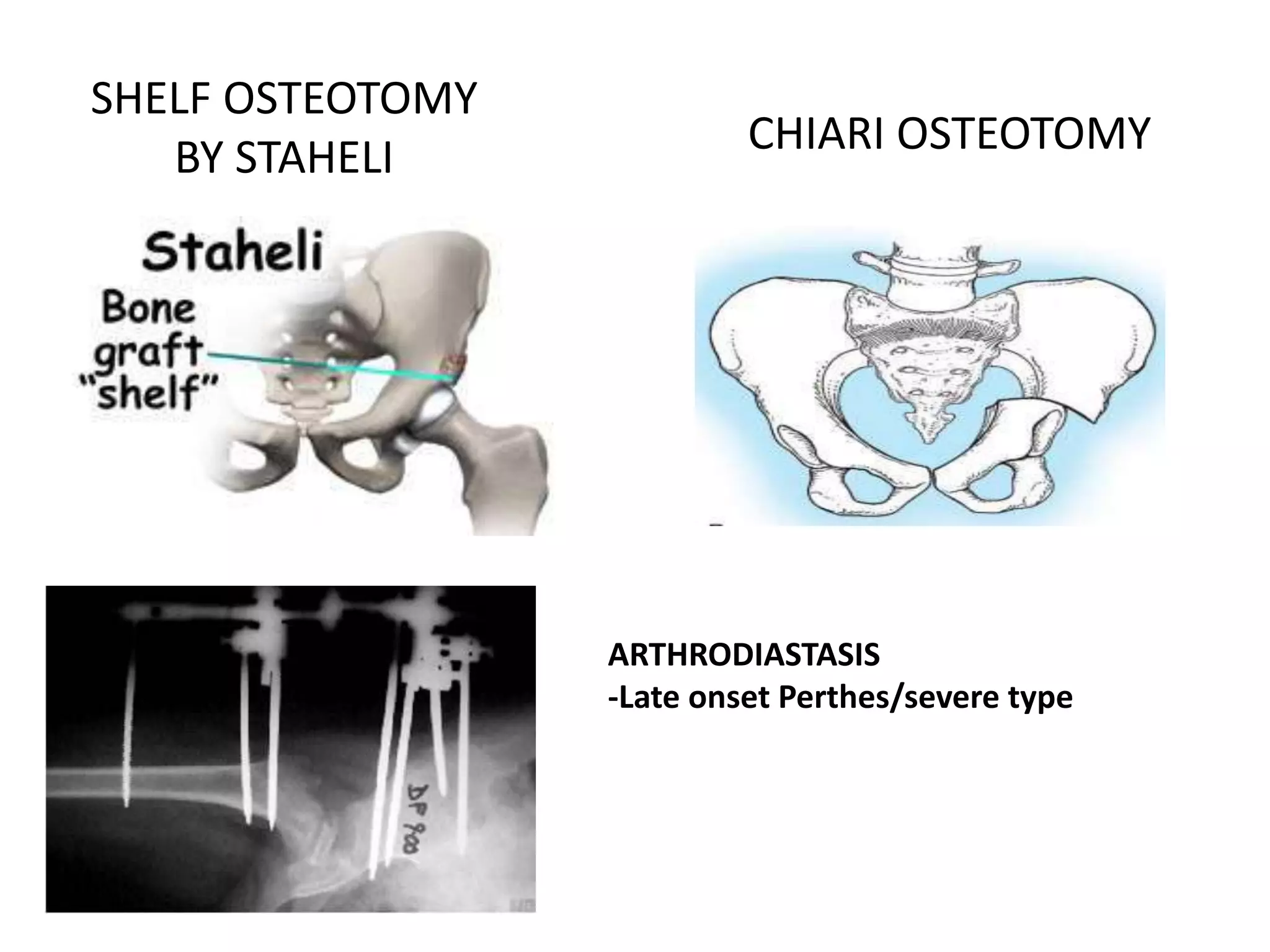
- Conservative management includes bracing for young/mild cases. Surgical containment is used for more severe/older cases to encourage spherical remodeling.
- Procedures