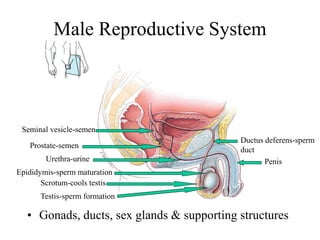
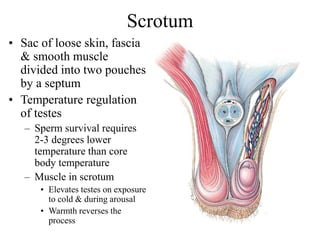
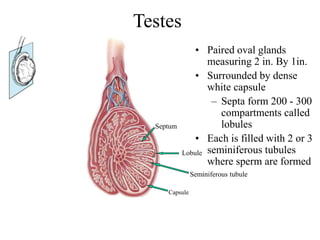
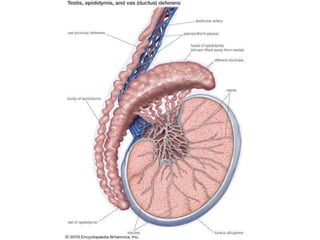
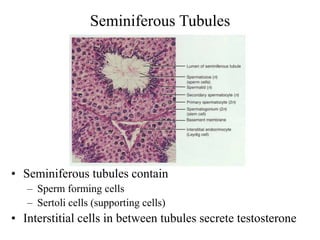
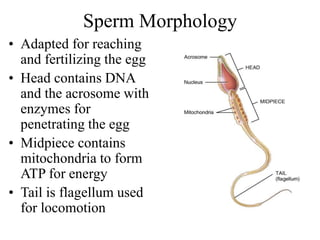
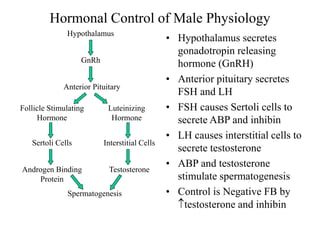
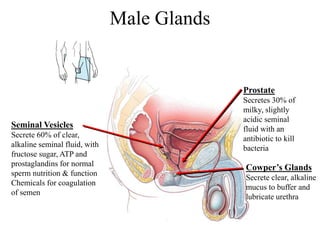
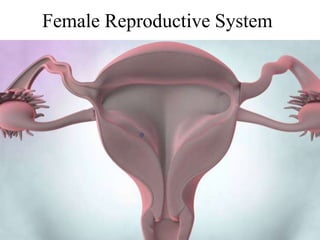
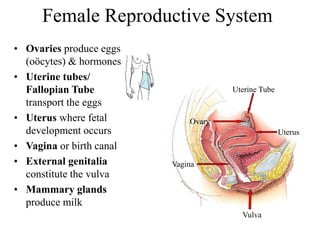
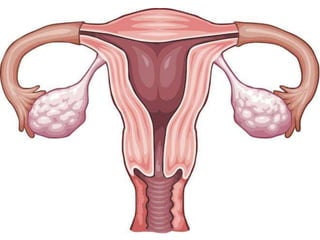
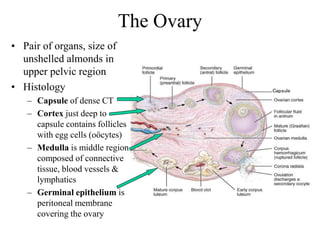
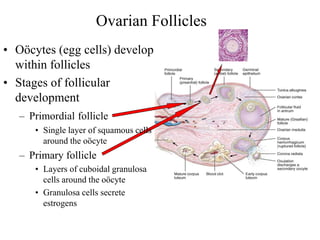
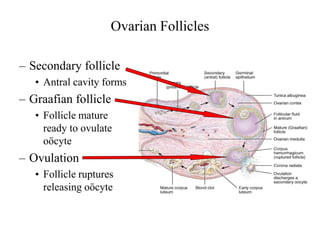
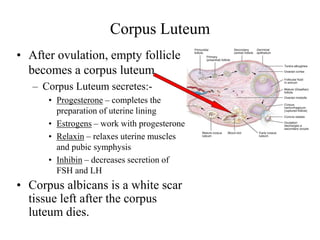
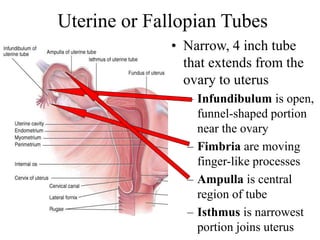
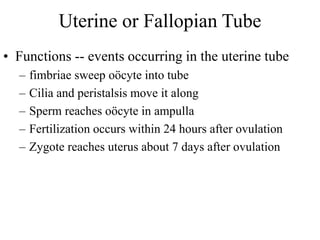
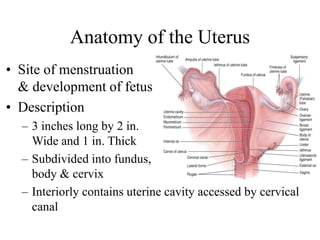
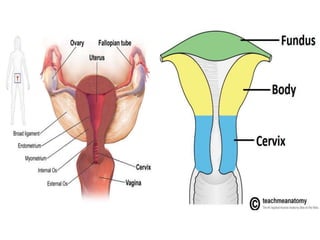
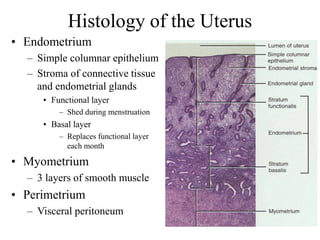
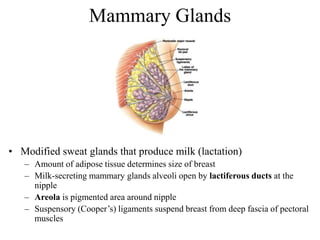
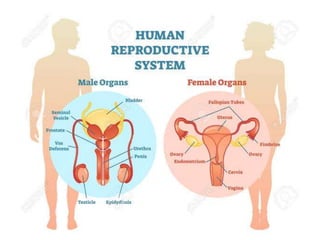
The document provides an overview of the male and female reproductive systems. It describes the key organs in both systems, including their functions and how they work together in processes like sperm production, ovulation, fertilization, and pregnancy. For the male system it covers the testes, penis, scrotum, seminal vesicles, prostate and their roles. For the female it discusses the ovaries, fallopian tubes, uterus, vagina, and mammary glands. Hormonal regulation is also summarized for both reproductive cycles.
![The Reproductive System
Anatomy of the Male and Female
Reproductive Systems
By: Dr. Shahbaz Ahmad PT
DPT [UIPT][UOL]
MS-MSK-PT [UIPT][UOL]
LECTURER [LIHS][LCPS]](https://image.slidesharecdn.com/sexualreproductivesystem-191130183030/85/Sexual-reproductive-system-2-320.jpg)