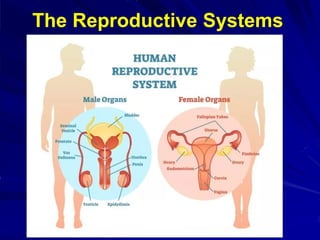
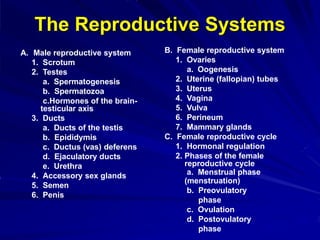
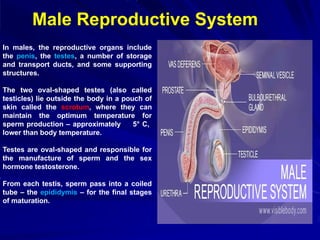
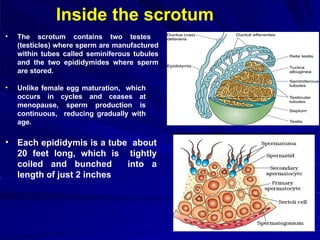
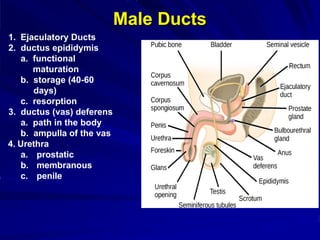
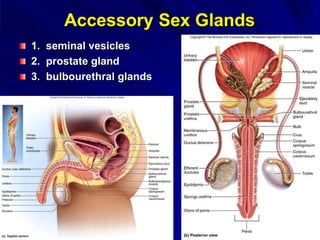
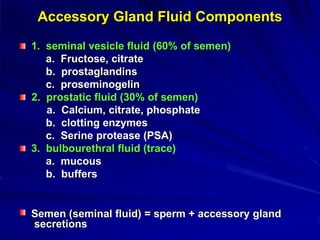
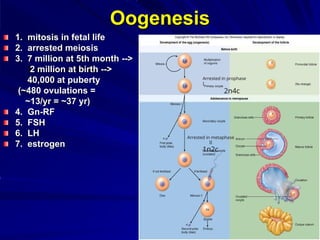
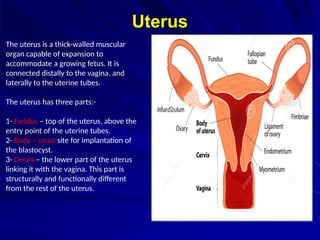
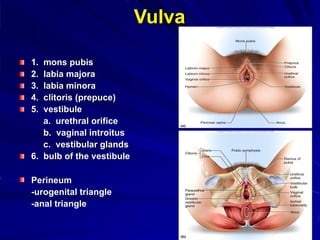
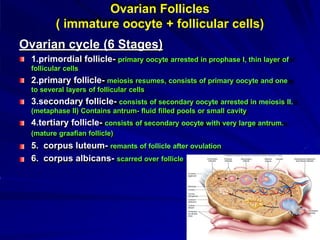
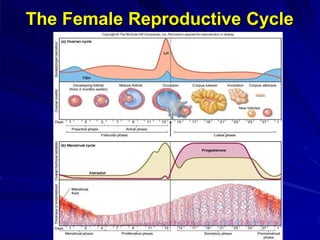
The document outlines the male and female reproductive systems, detailing their anatomical structures and functions, including the process of gametogenesis, hormonal regulation, and the reproductive cycle. It describes the roles of gonads, ducts, and accessory glands in males, as well as the ovaries, uterine tubes, uterus, and vagina in females. Additionally, it explains key processes like spermatogenesis and oogenesis, alongside hormonal interactions guiding reproduction.