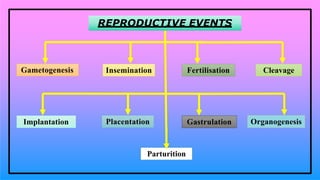
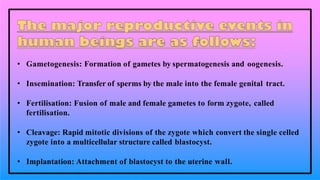
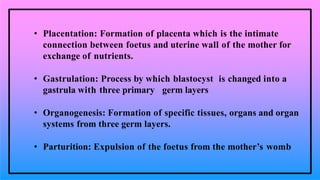
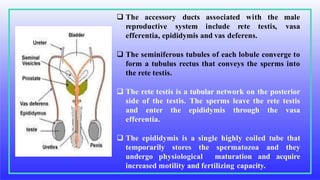
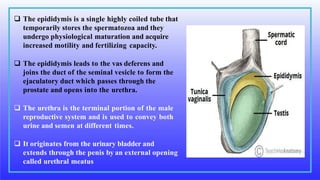
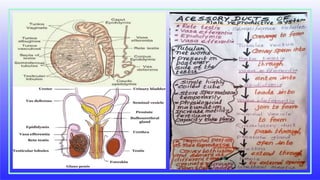
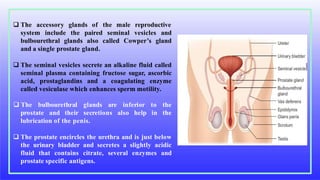
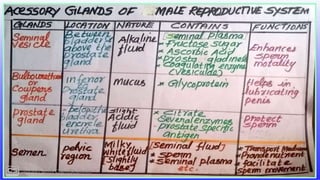
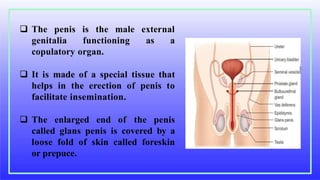
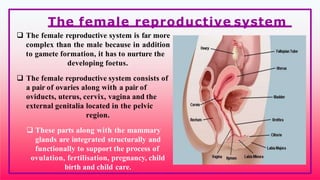
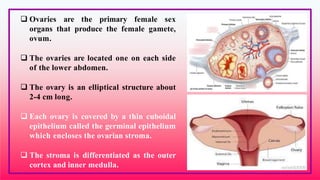
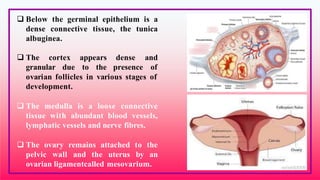
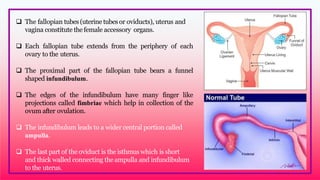
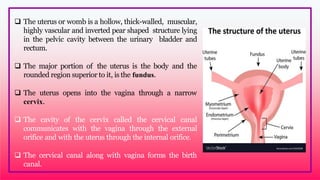
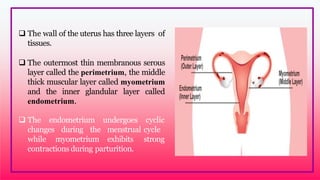
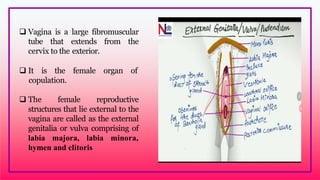
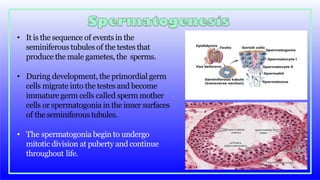
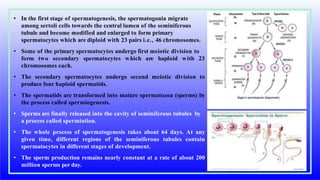
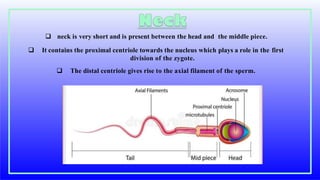
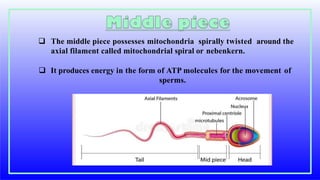
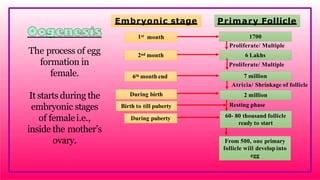
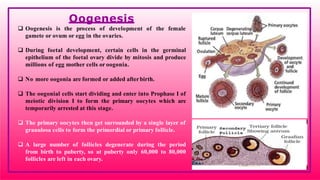
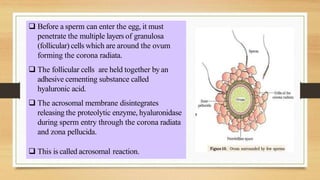
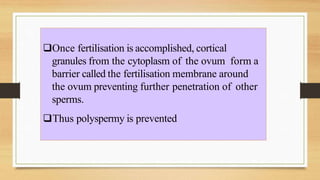
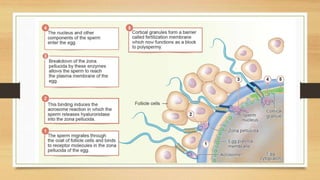
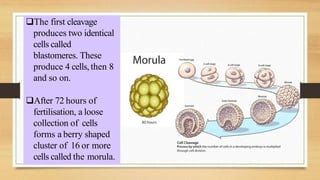
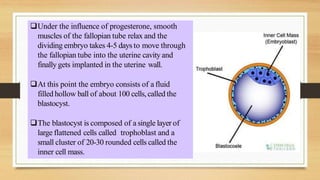
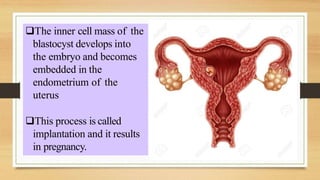
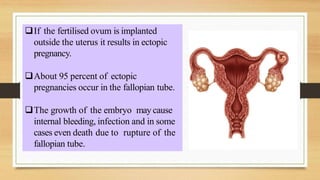
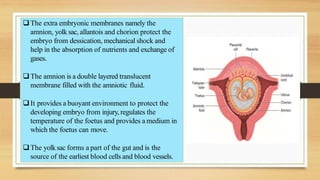
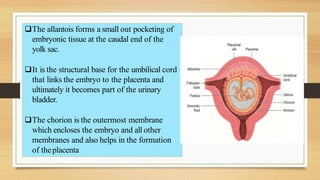
The document provides an overview of the human reproductive system. It describes the key functions and structures of both the male and female reproductive systems. In the male system, it explains gametogenesis (sperm production) in the testes and seminiferous tubules, and the role of accessory organs like the vas deferens and seminal vesicles. In the female system, it outlines gametogenesis (egg production) in the ovaries, as well as the functions of structures like the fallopian tubes, uterus, and vagina in supporting fertilization and pregnancy. Key reproductive events from fertilization to childbirth are also summarized.