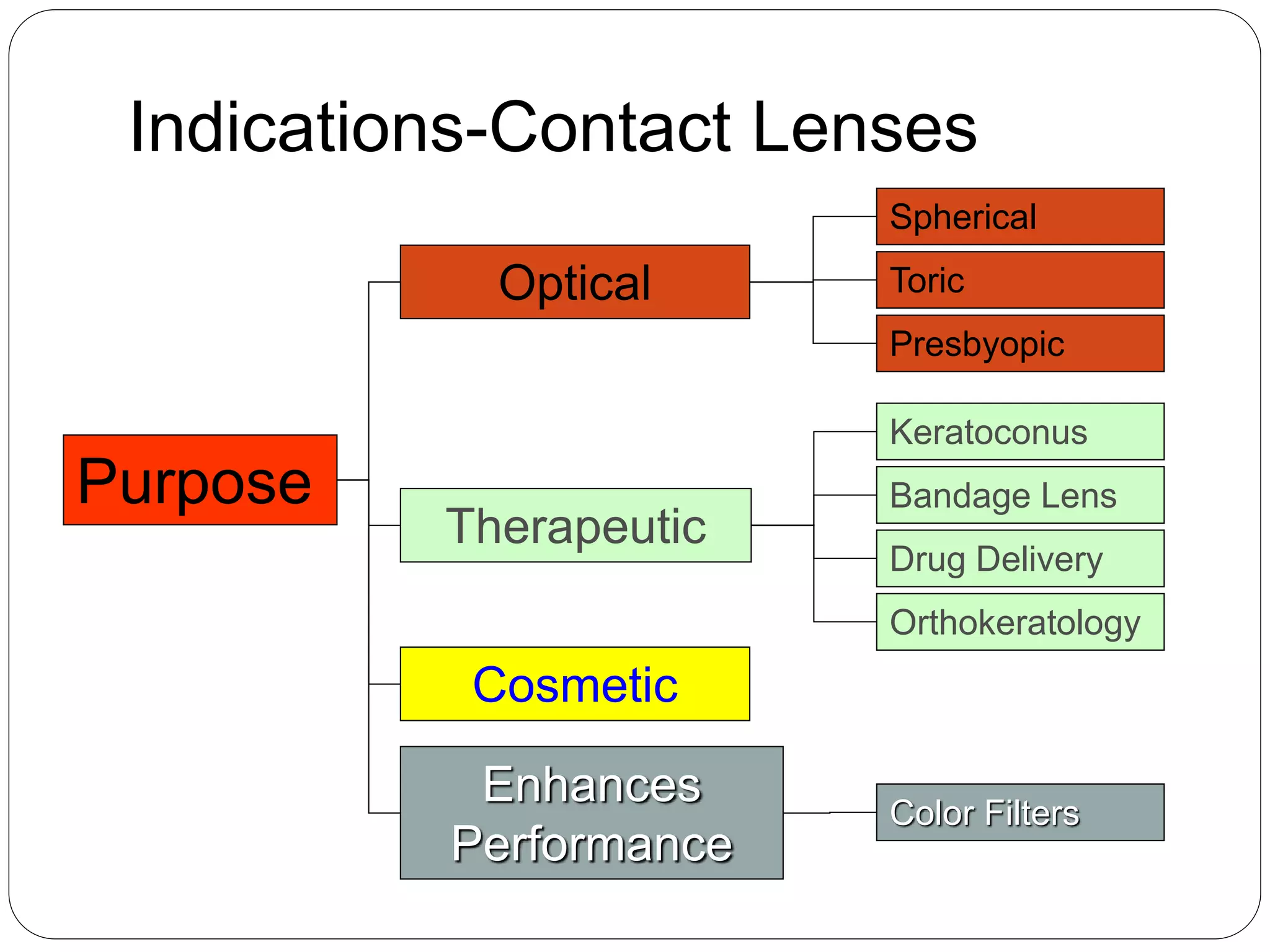
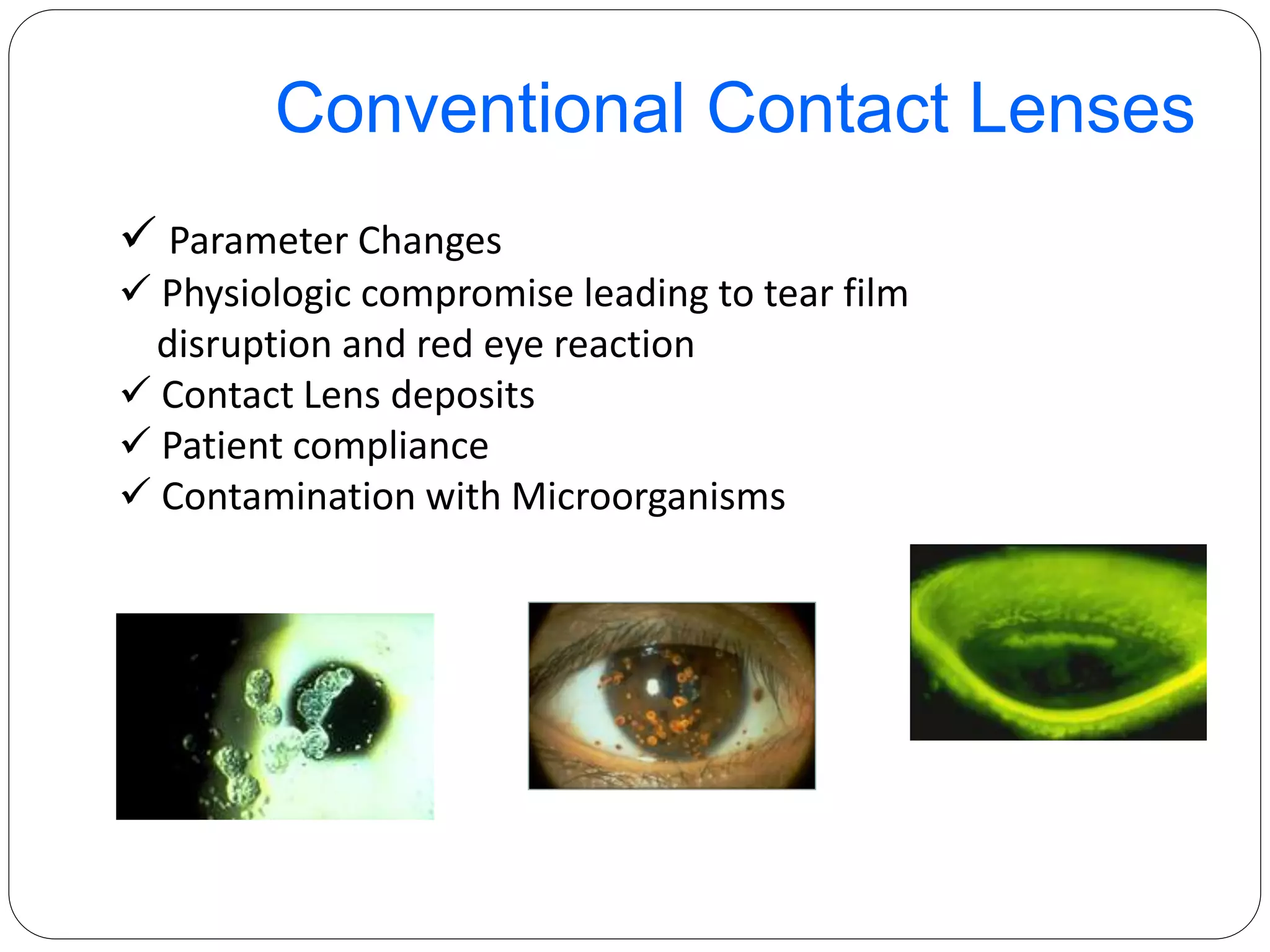
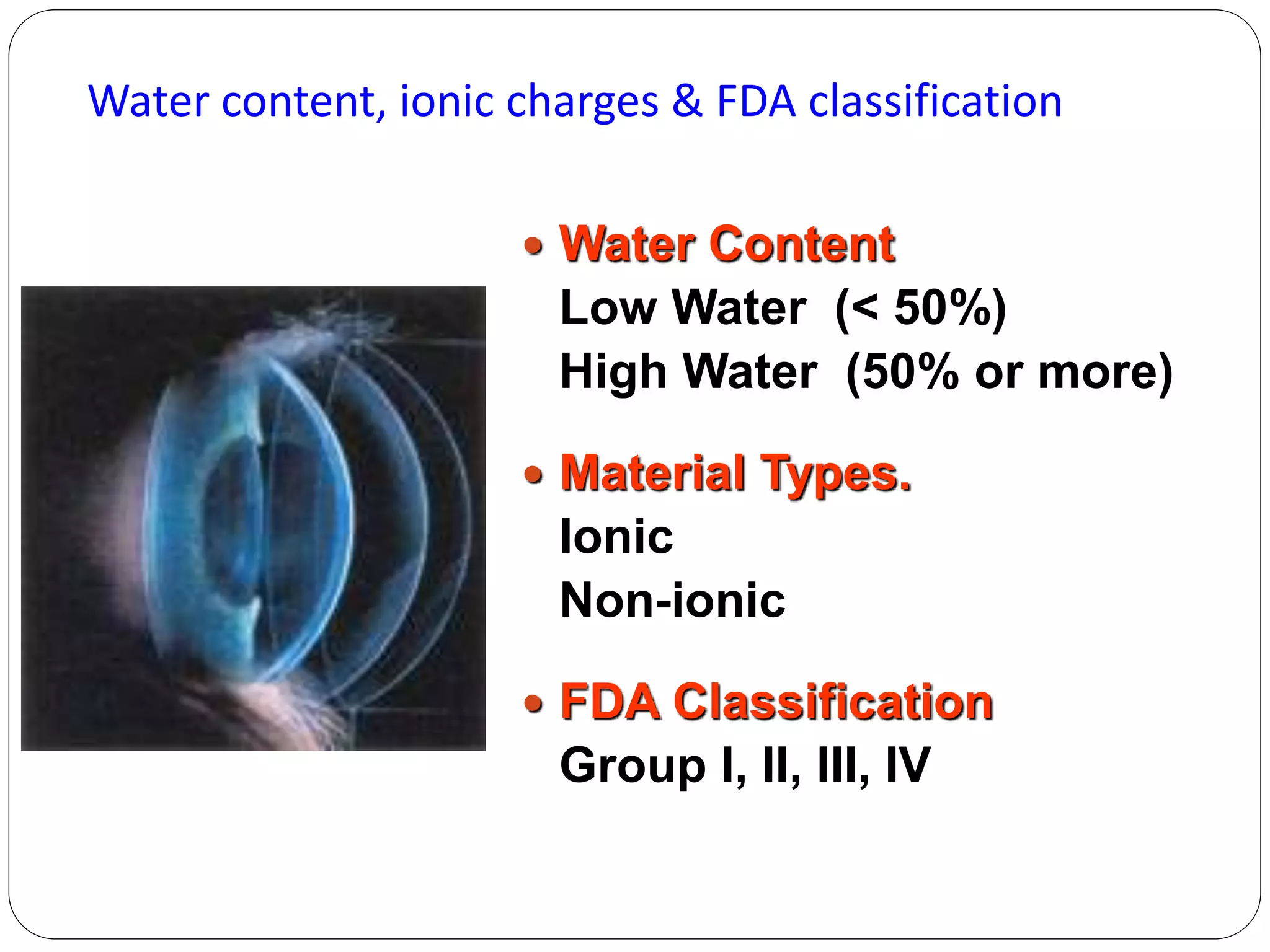
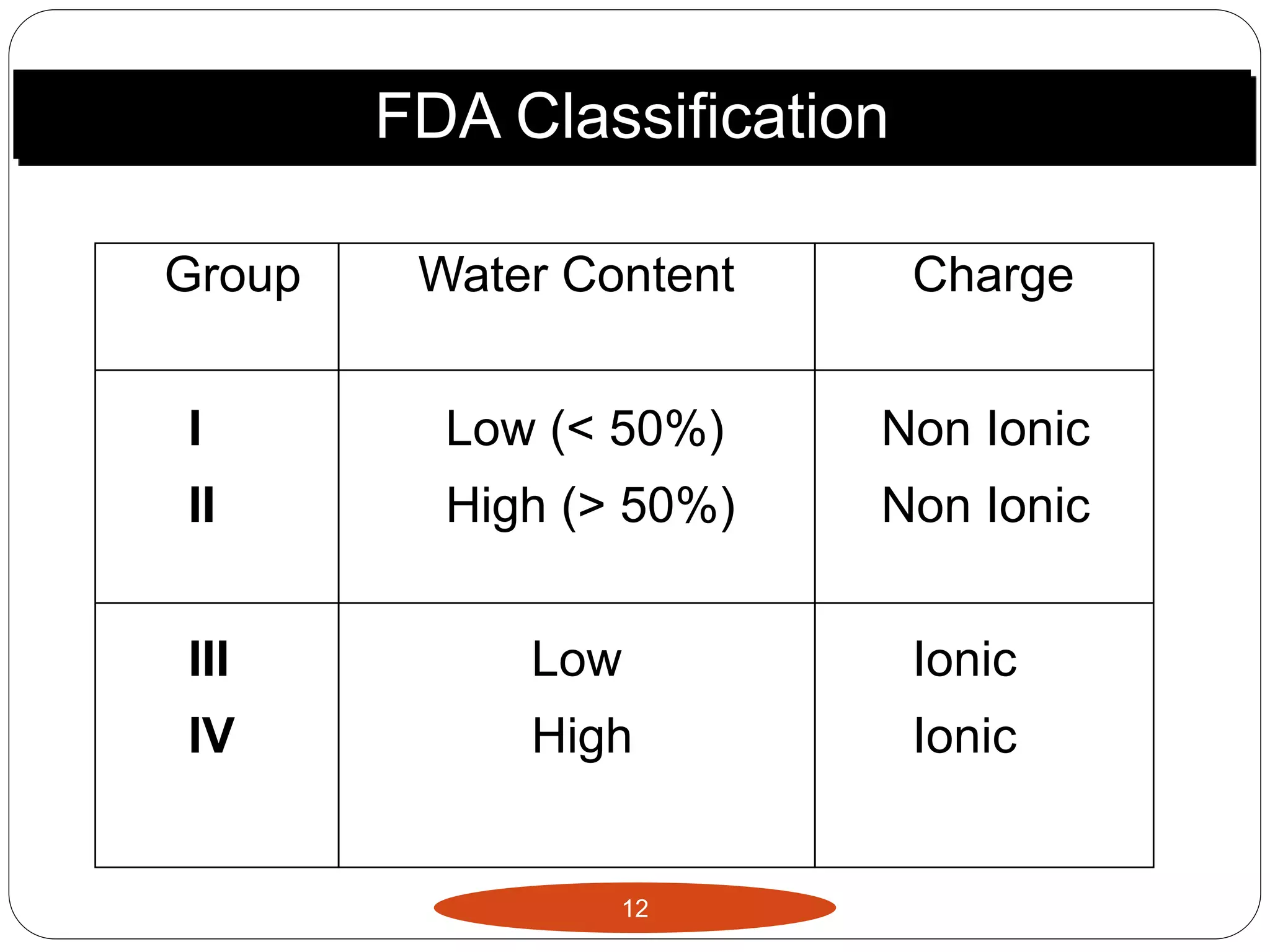
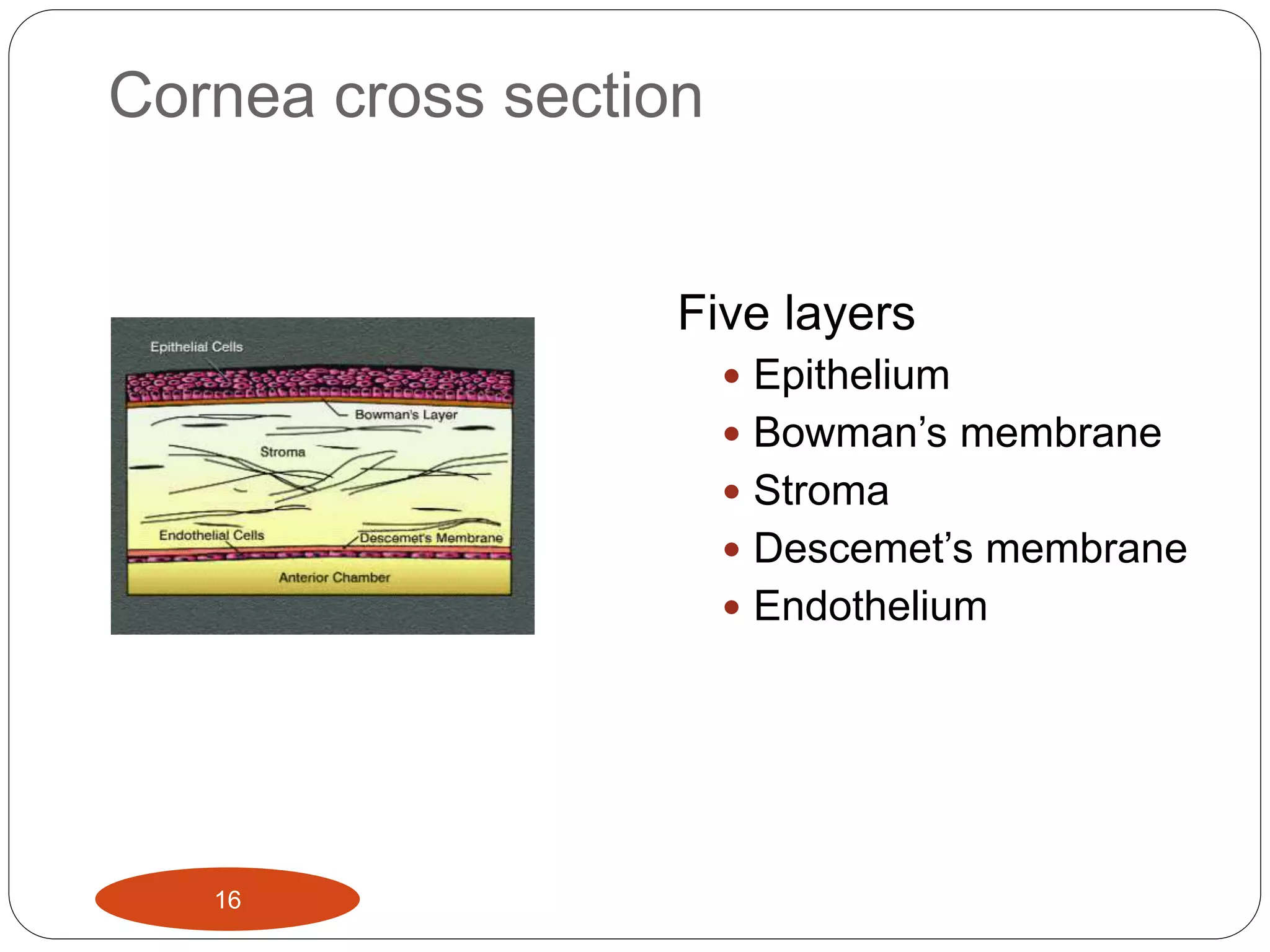
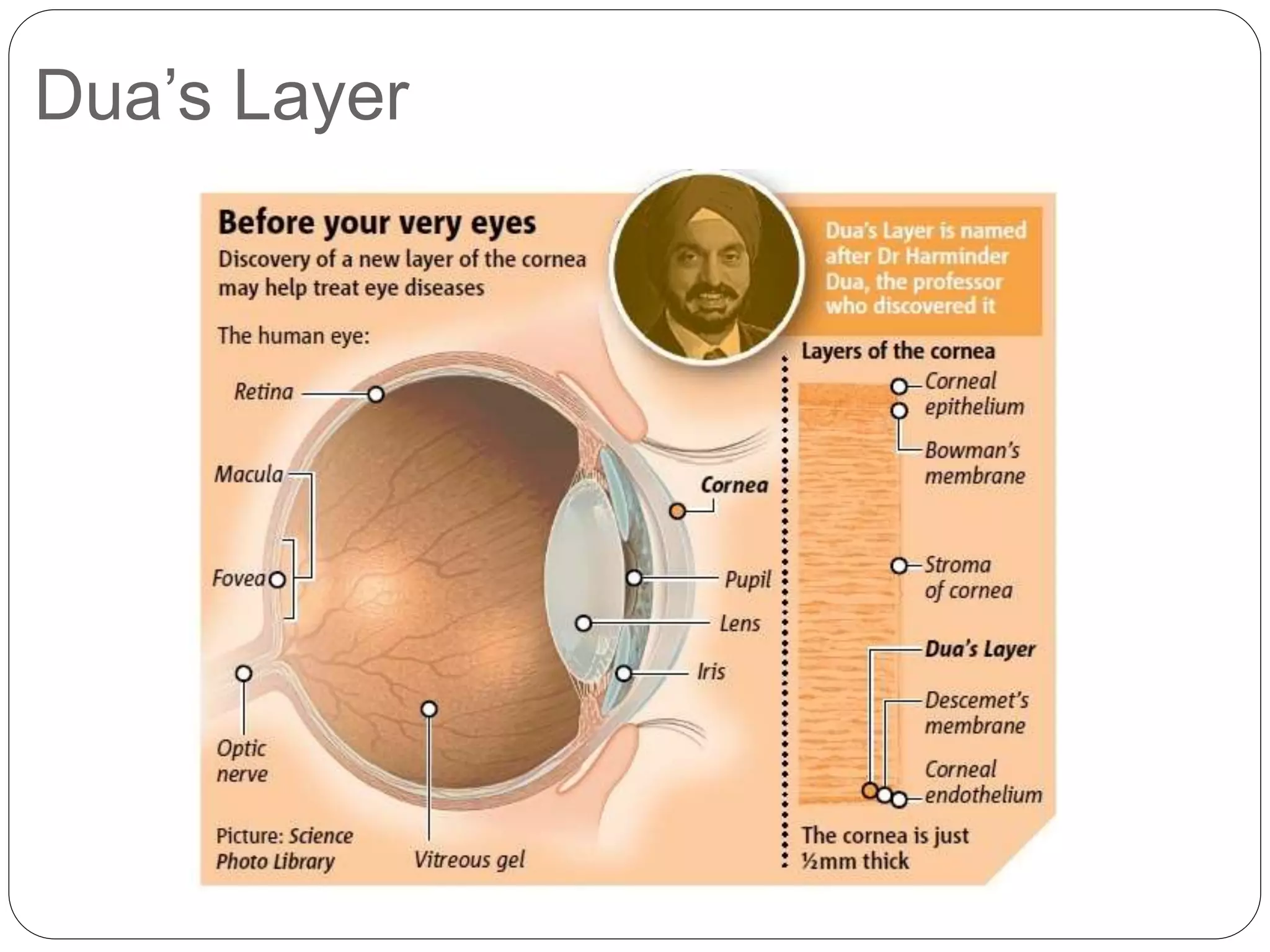
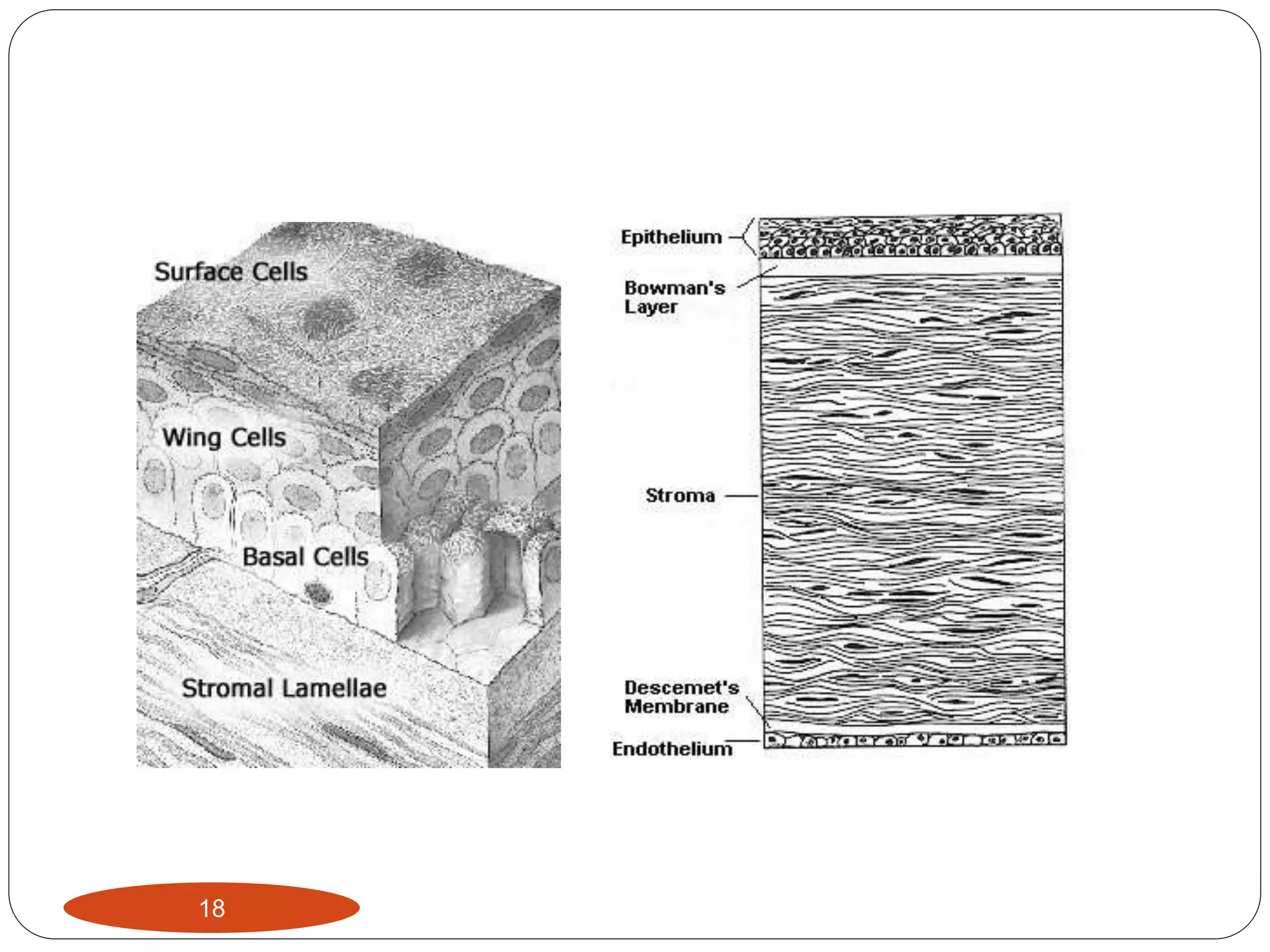
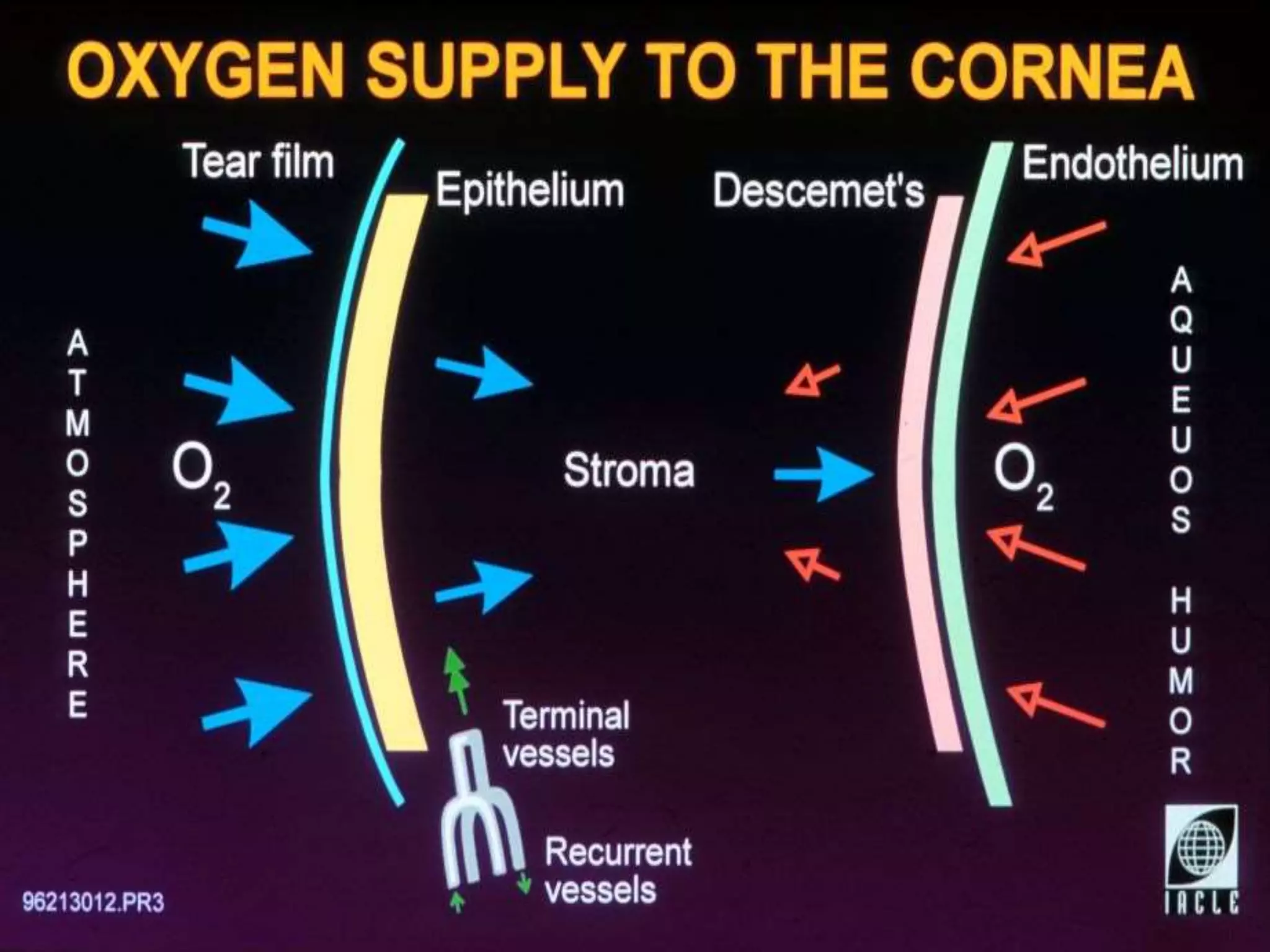
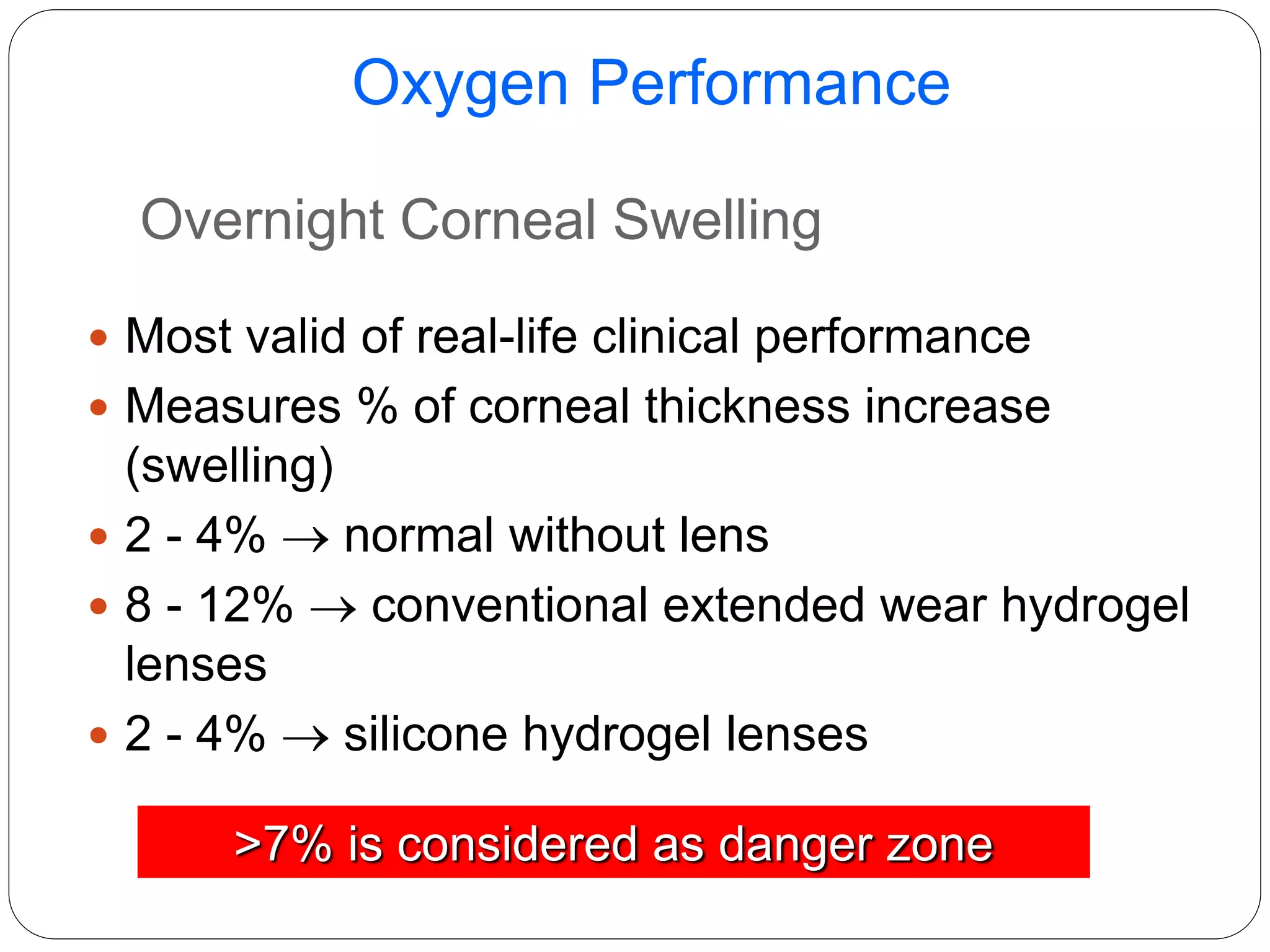
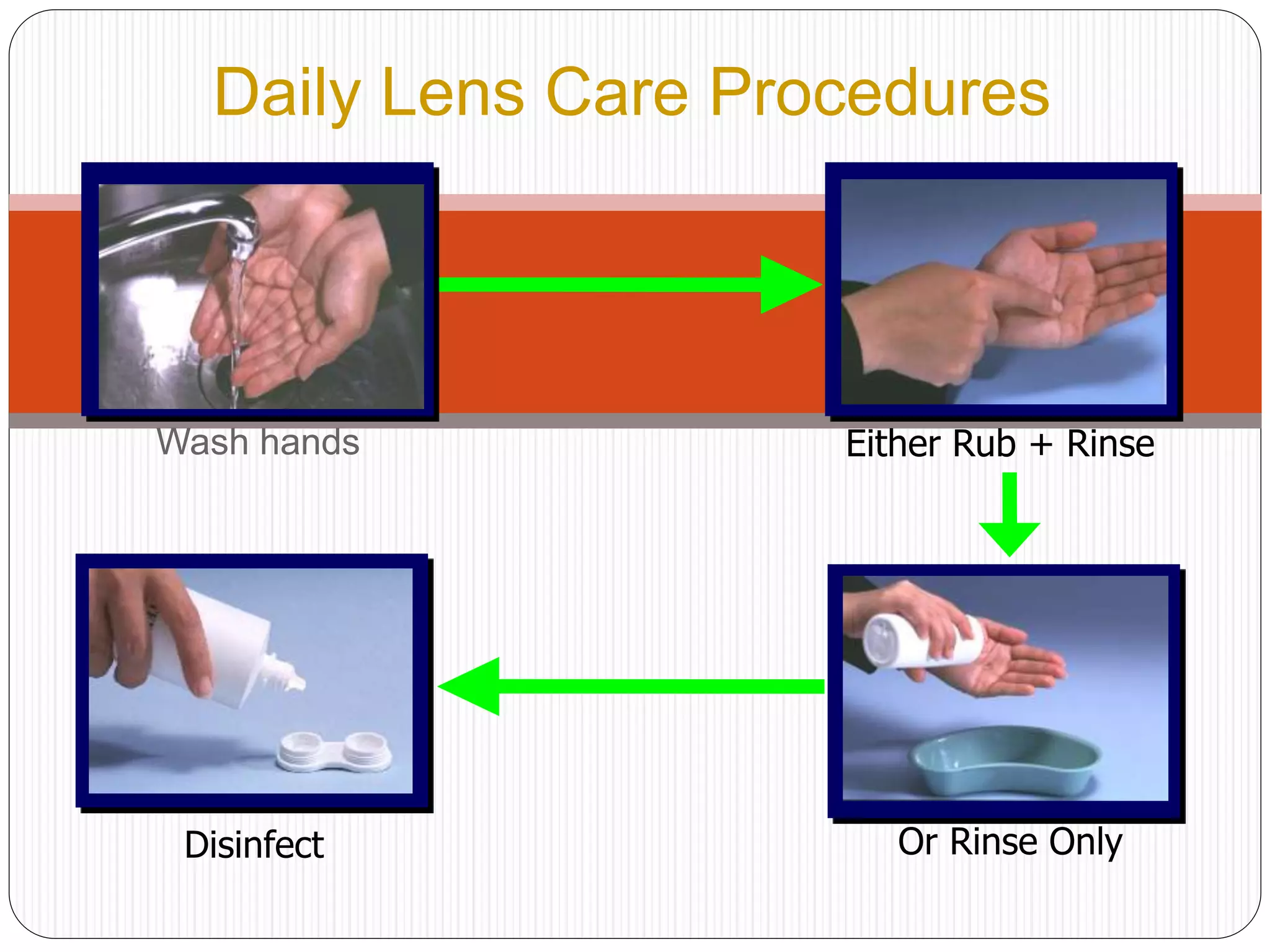
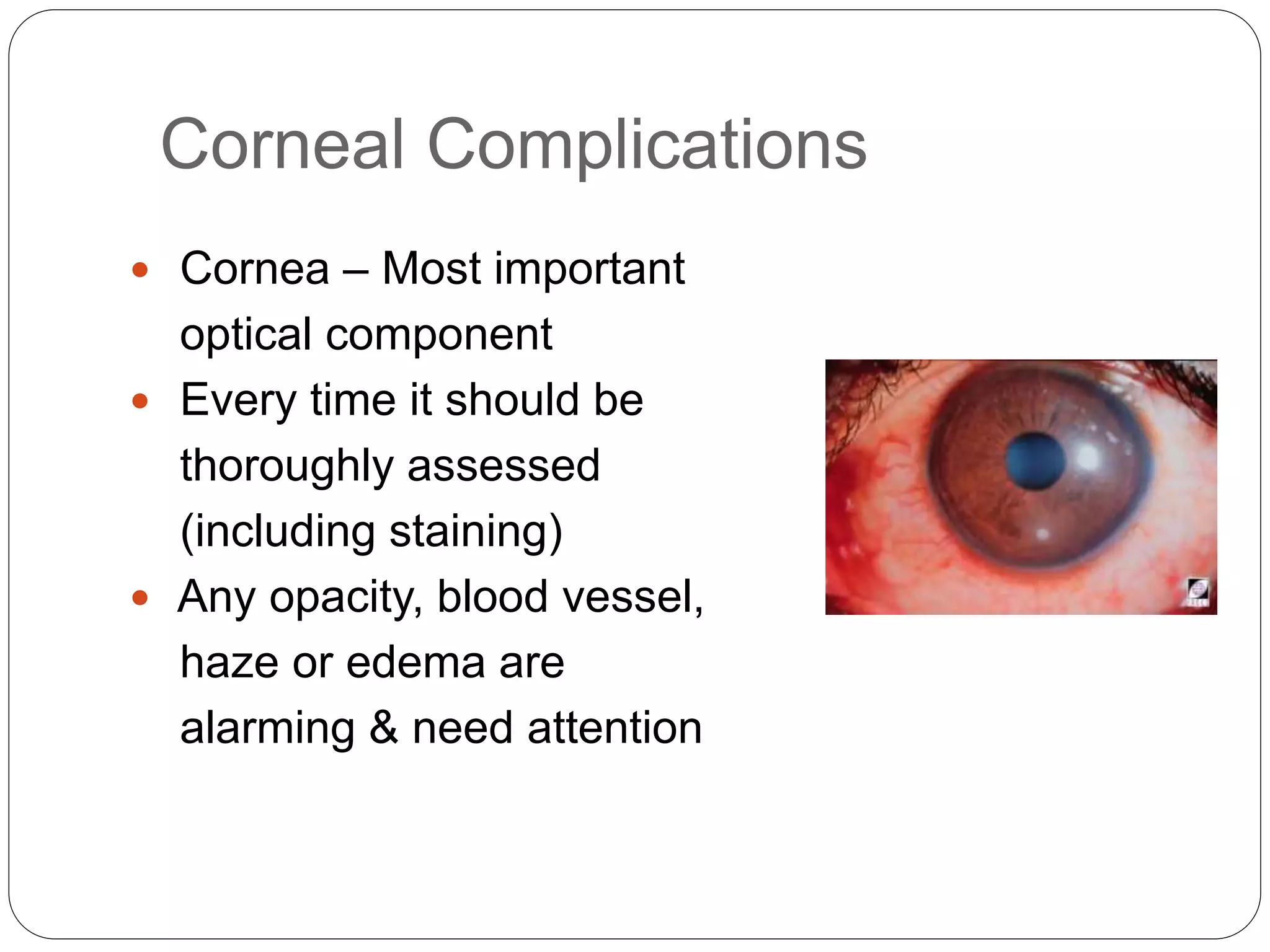
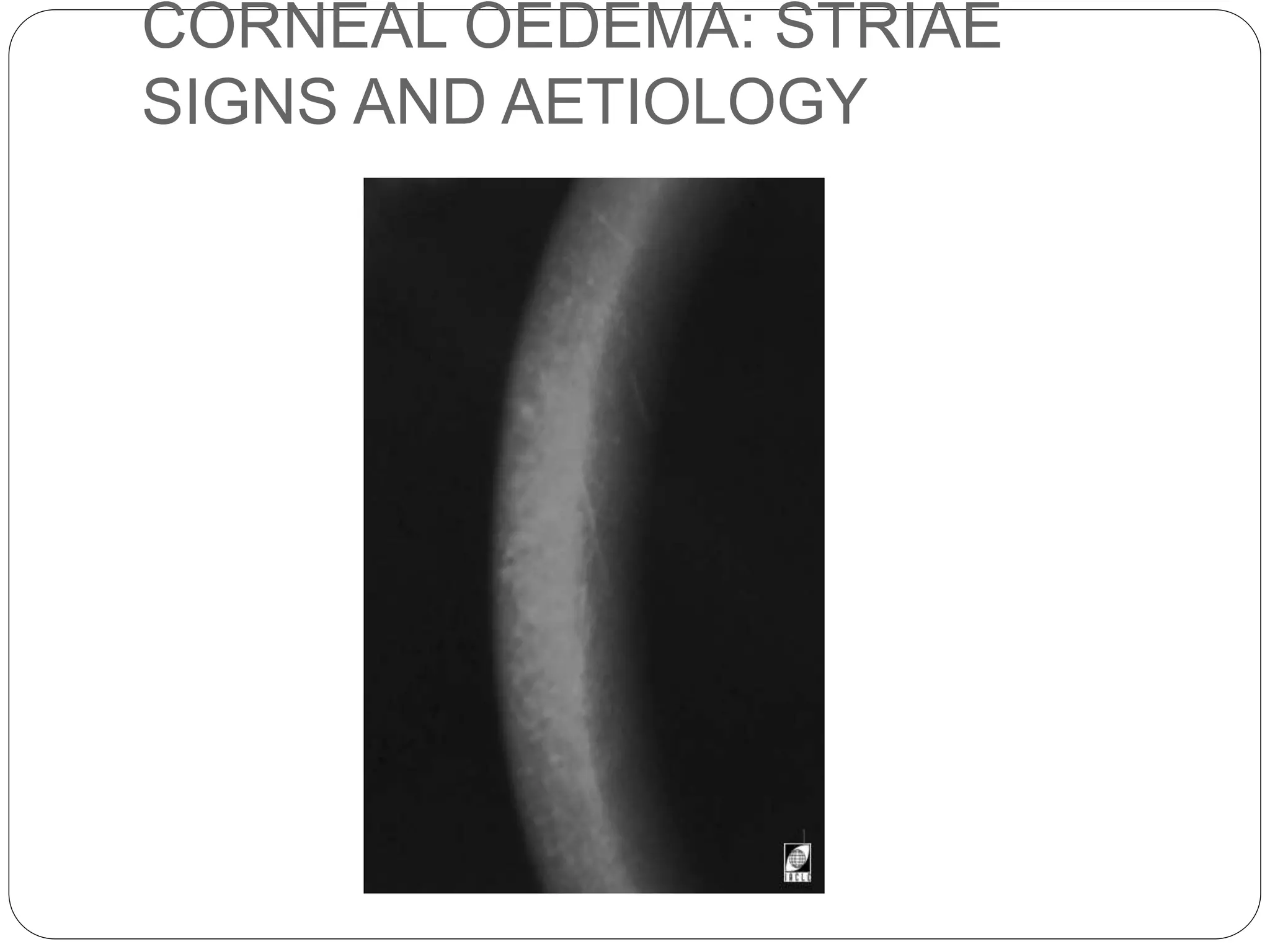
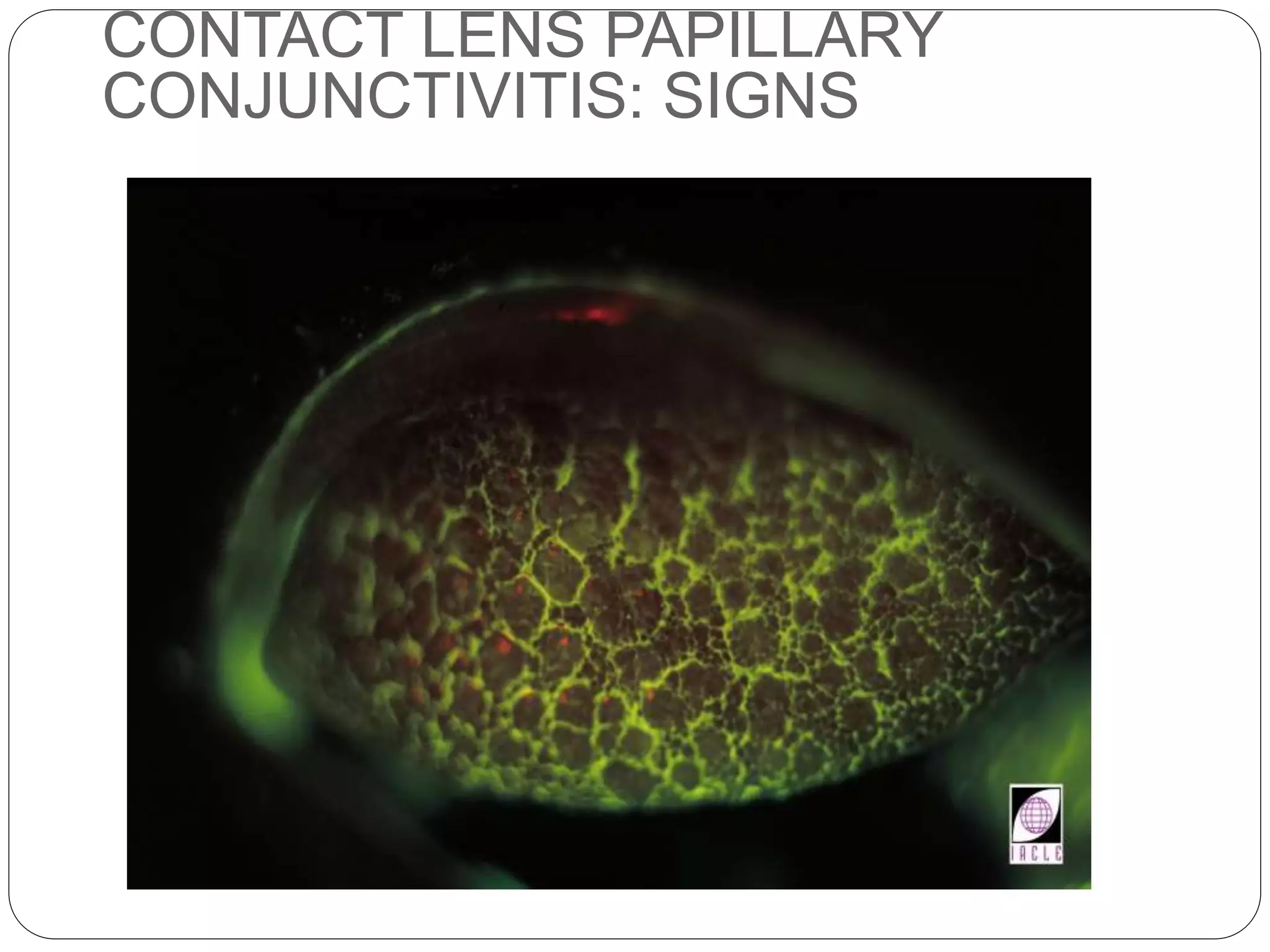
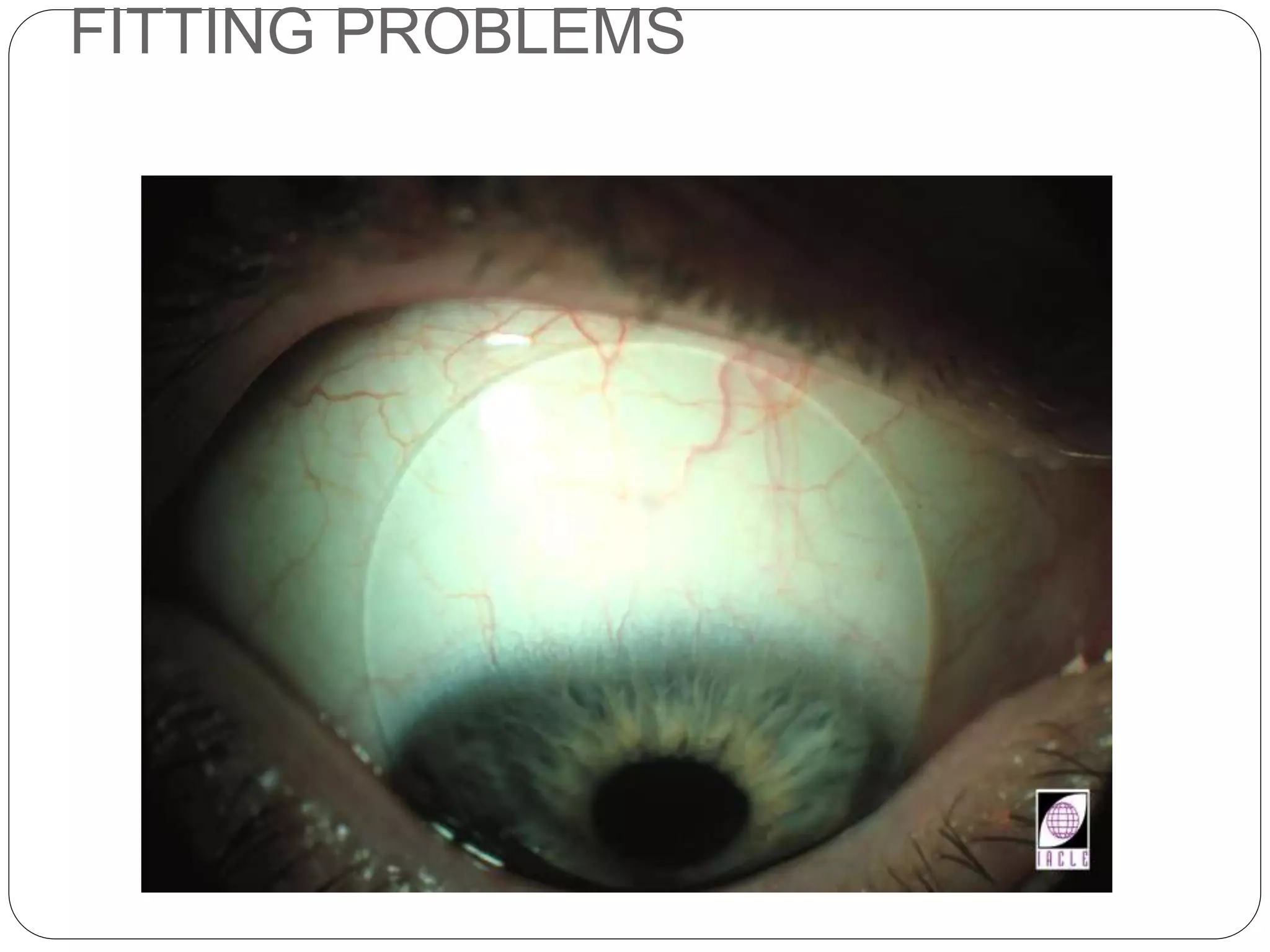
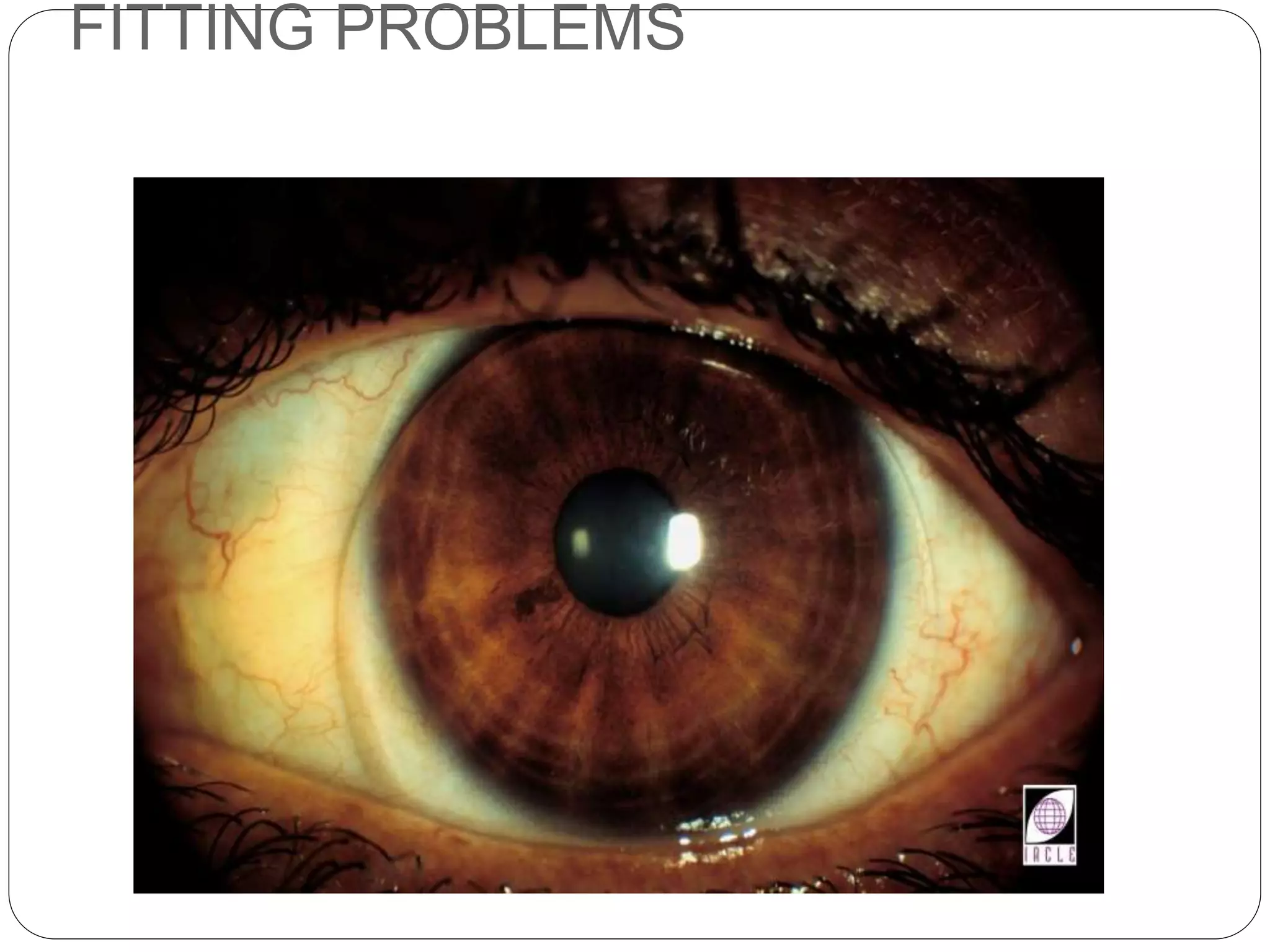
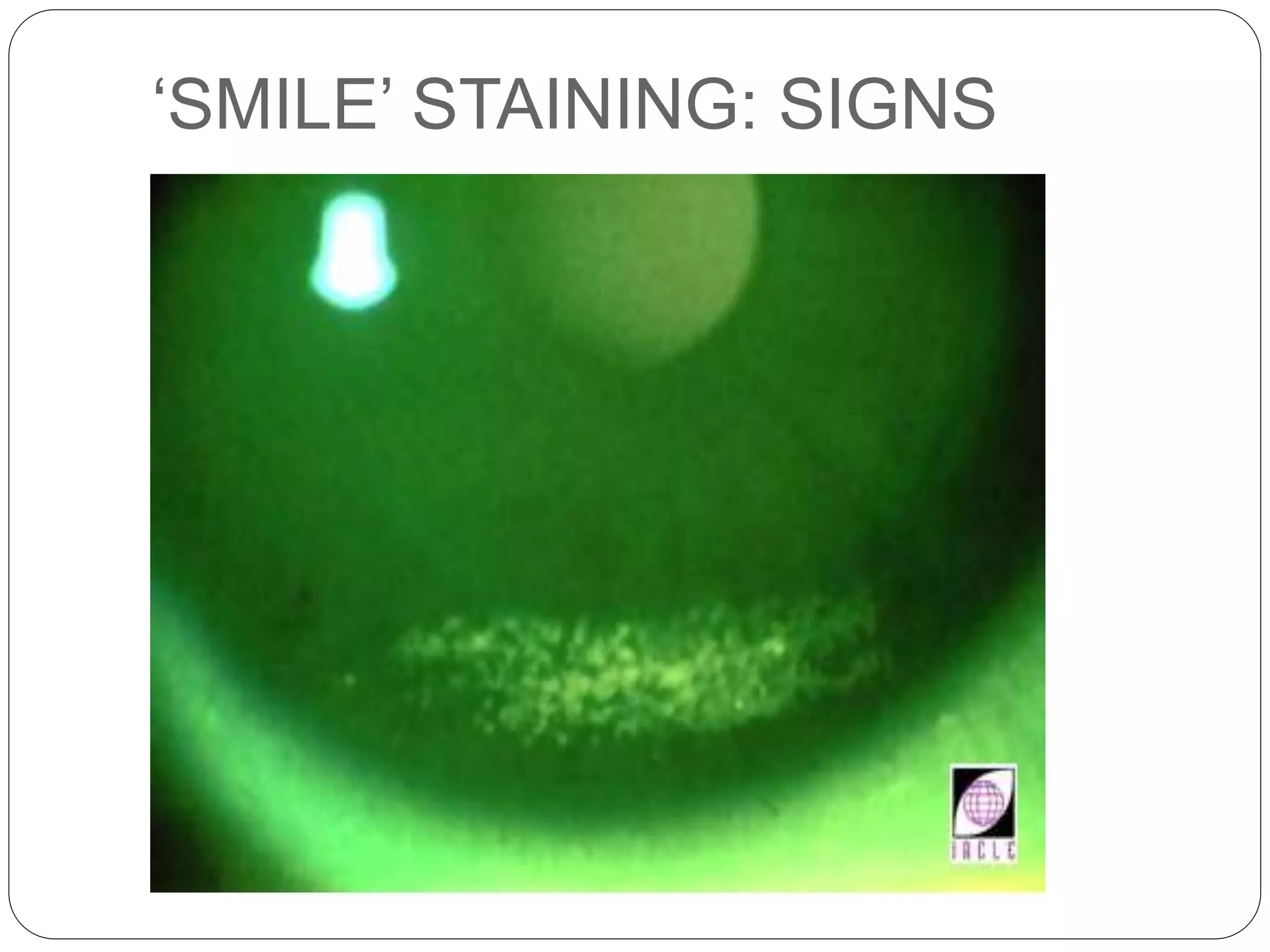
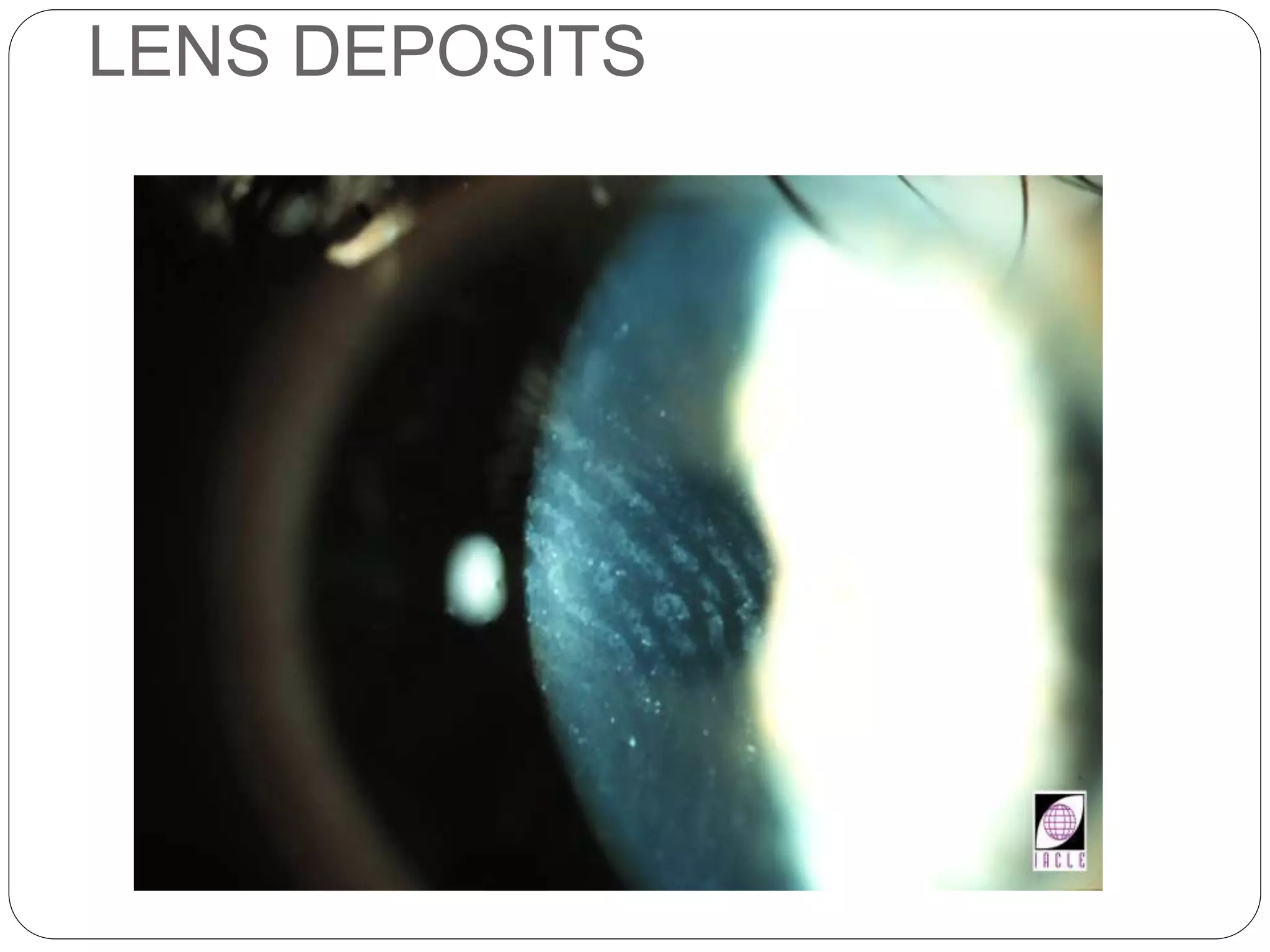
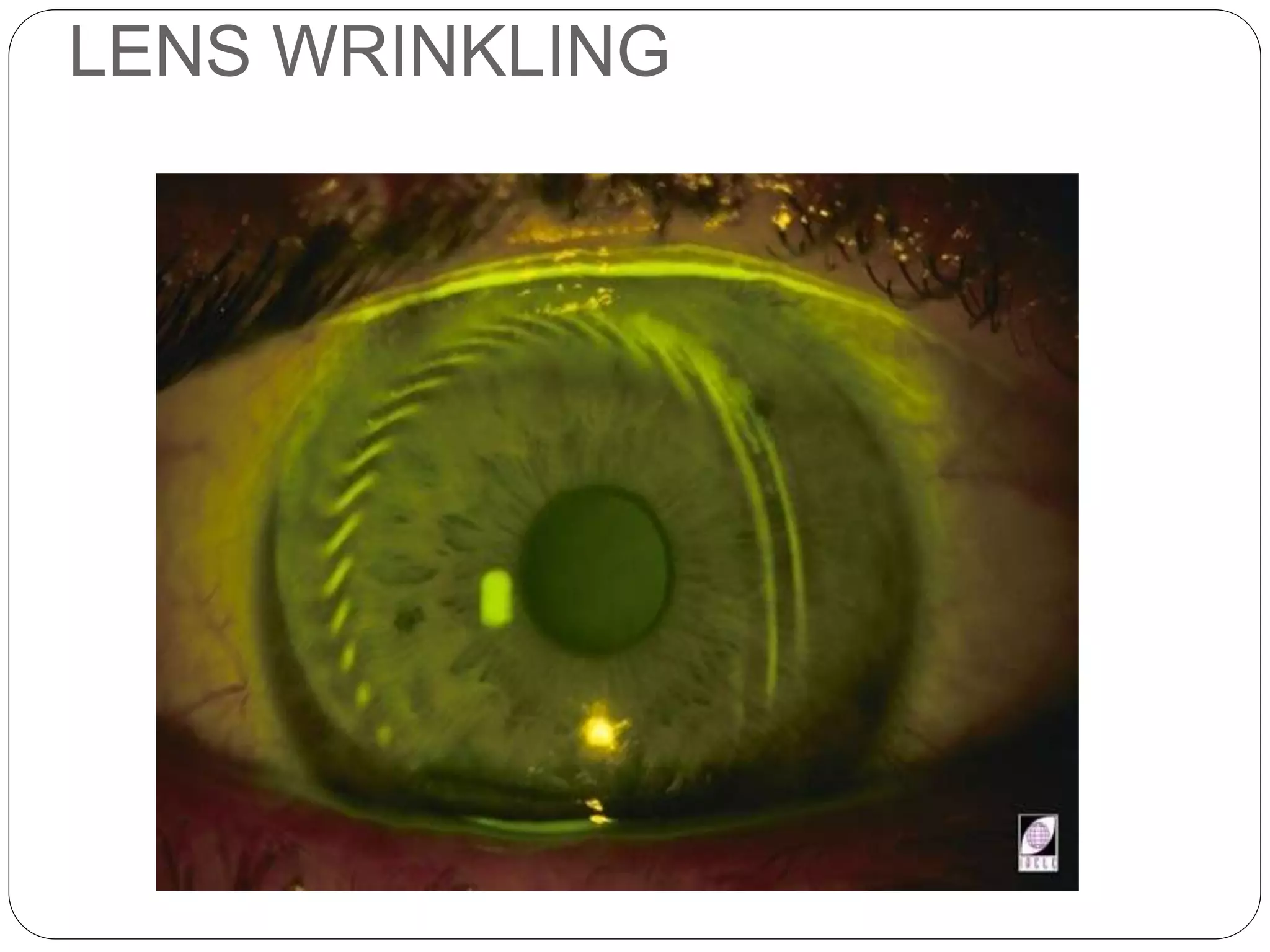
This document discusses contact lens wear and corneal health. It outlines the key factors for successful contact lens wear, including 12 hours of comfortable wear and good end-of-day comfort. It also discusses consumers' priorities around contact lens health and definitions of a "healthier contact lens." Silicone hydrogel lenses are highlighted as improving oxygen transmission and reducing complications compared to conventional lenses. Proper lens care, handling, materials selection and follow-up care are emphasized to prevent complications and support corneal health with contact lens wear.