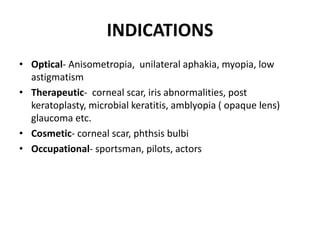
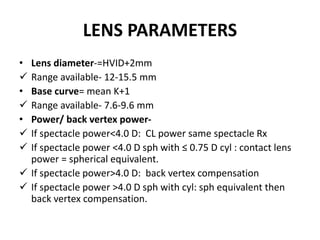
The document discusses soft contact lenses, covering their indications, contraindications, advantages, disadvantages, complications, and classifications based on wear modalities. It also details the fitting and evaluation processes, including initial examination, lens parameters, insertion and removal techniques, and fitting evaluation criteria. Overall, it provides a comprehensive overview of soft contact lens usage and management.