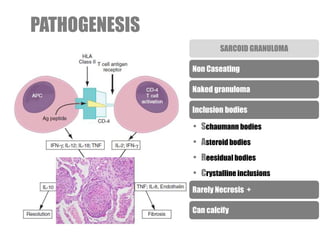
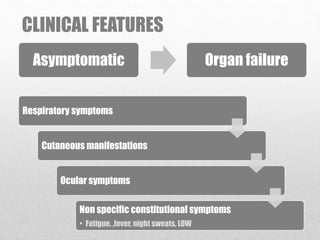
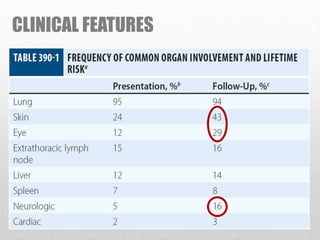
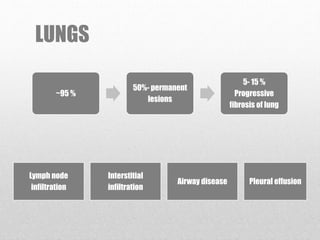
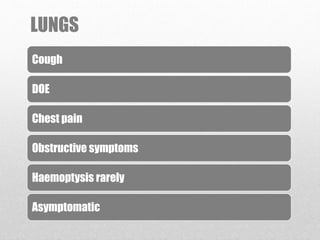
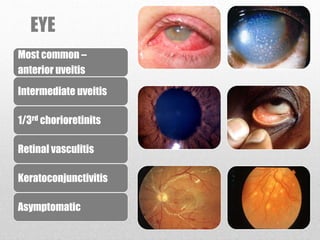
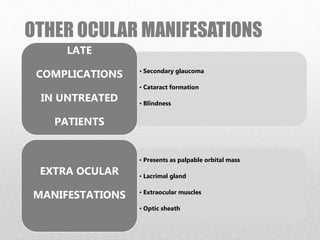
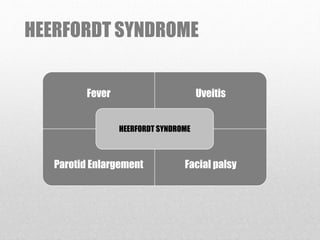
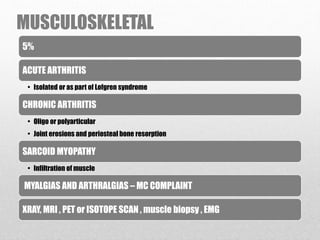
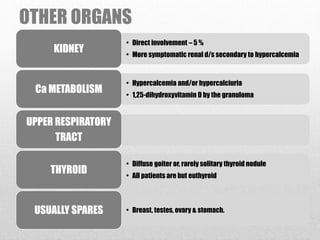
- Sarcoidosis is a multi-system inflammatory disease characterized by non-caseating granulomas that can affect multiple organs. It most commonly involves the lungs, skin, and eyes.
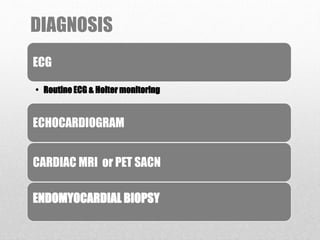
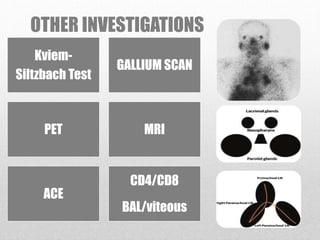
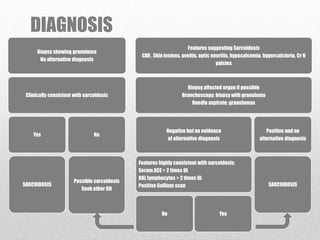
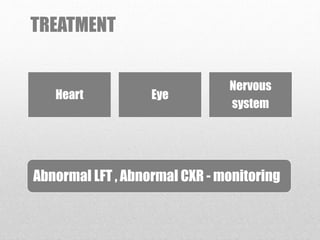
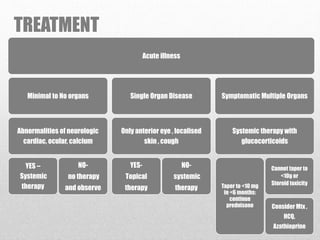
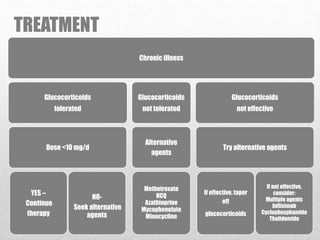
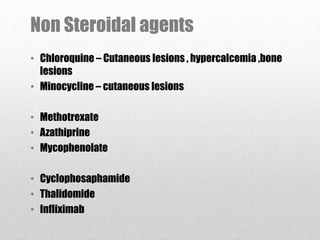
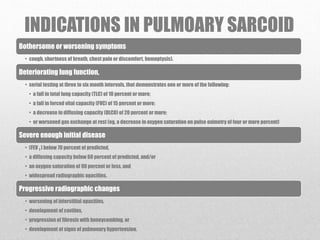
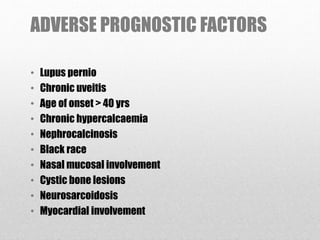
- Diagnosis requires compatible clinical features along with histological evidence of non-caseating granulomas and exclusion of alternative diagnoses. Treatment involves glucocorticoids and immunosuppressants depending on the severity and organs involved. Prognosis depends on the specific organs affected and presence of adverse factors like lupus pernio or chronic uveitis.