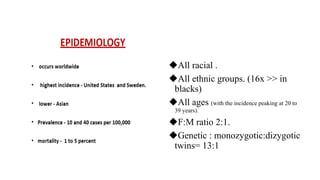
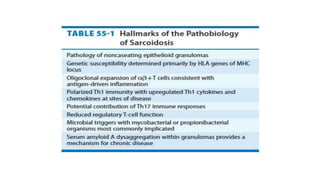
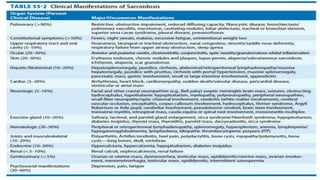
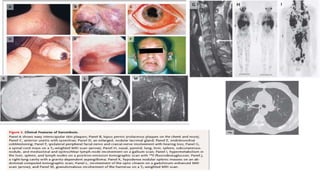
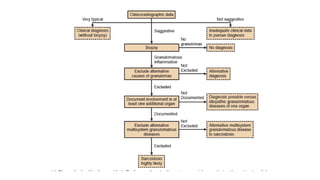
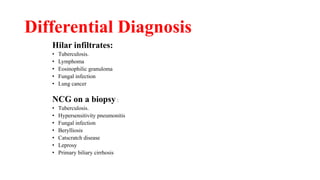
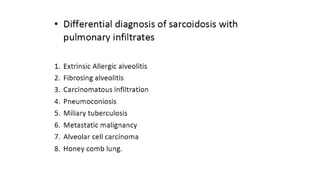
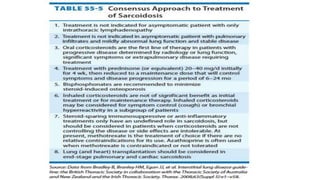
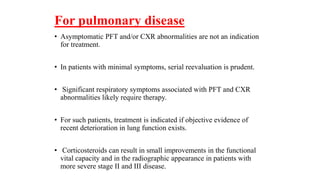
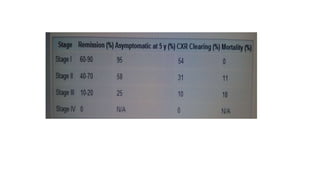
Sarcoidosis is a multisystem inflammatory disease primarily affecting the lungs, characterized by noncaseating epithelioid granulomas and has an unknown etiology. It has varying prevalence across demographics and can lead to diverse symptoms, with pulmonary involvement being most common, while also potentially affecting skin, eyes, liver, and nervous system. Diagnosis relies on clinical, radiologic, and histologic evidence, and treatment primarily involves corticosteroids, with many patients experiencing significant improvement or remission over time.