This document provides information on sarcoidosis, including:
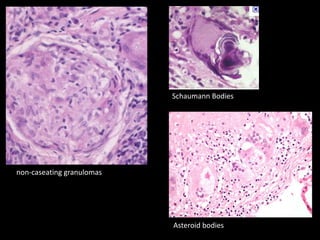
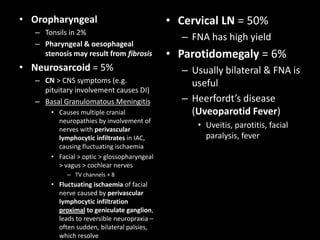
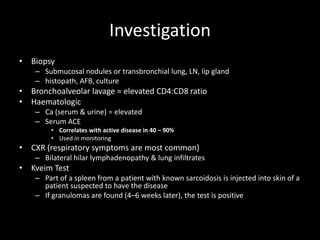
1) It is a chronic granulomatous disease characterized by noncaseating granuloma formation of unknown cause, often affecting the lungs and lymph nodes.
2) It has a higher prevalence in African Americans and Japanese populations. The disease often affects people aged 20-40 and has a female predominance.
3) Granulomas form as a result of an abnormal cellular immune response potentially triggered by infectious agents. This leads to the formation of noncaseating granulomas containing giant cells.
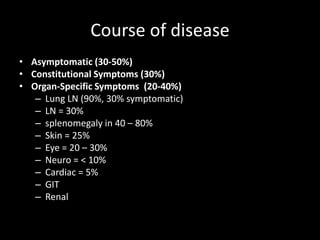
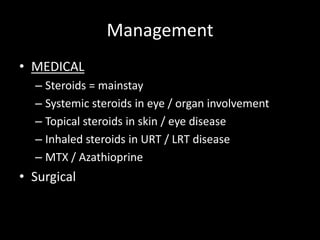
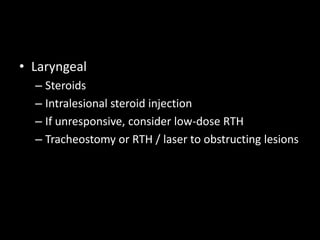
4) The disease can have acute or chronic presentations and involve multiple organs, with lungs and lymph nodes most commonly affected. Corticost