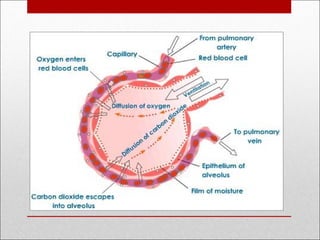
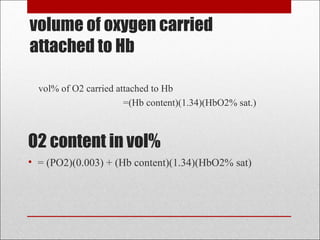
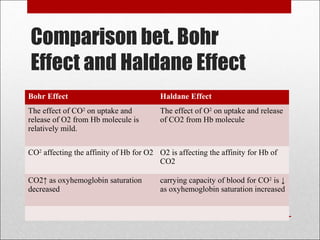
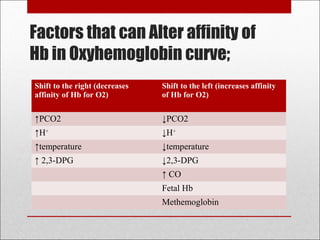
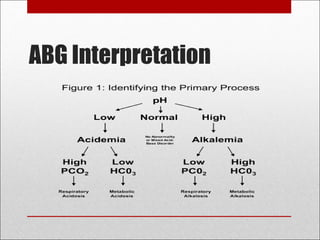
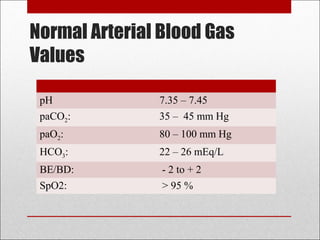
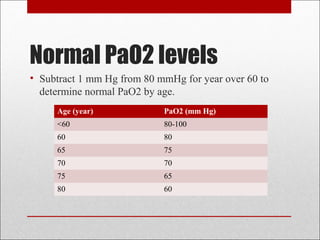
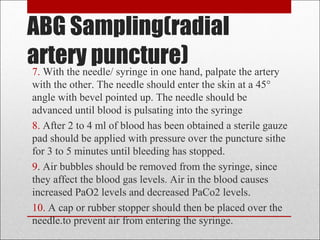
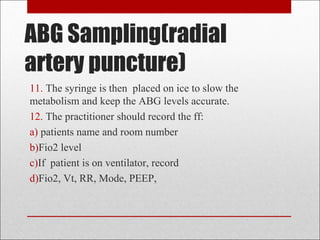
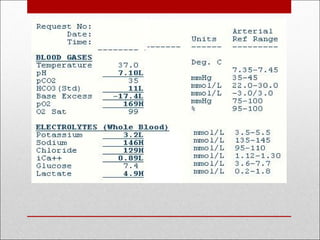
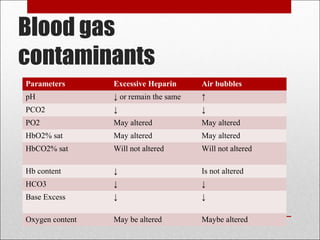
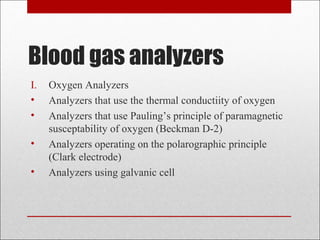
This document discusses arterial blood gas analysis, including the physiology of oxygenation and factors that influence hemoglobin's affinity for oxygen. It provides reference ranges for blood gas values and guidelines for interpreting results. Techniques for obtaining blood samples and potential complications are outlined. Blood gas analyzers and quality assurance procedures are also reviewed.