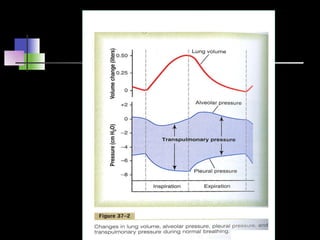
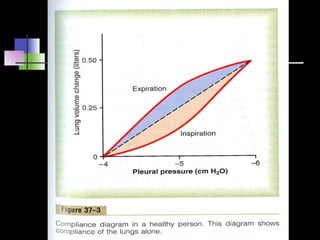
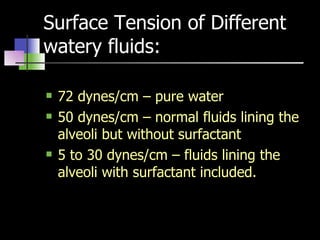
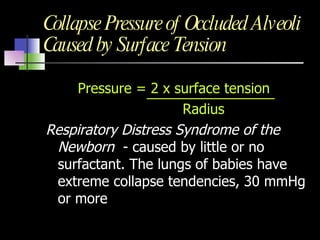
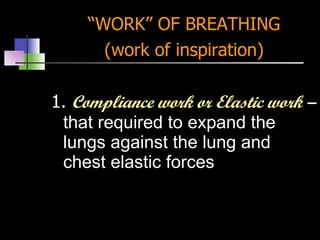
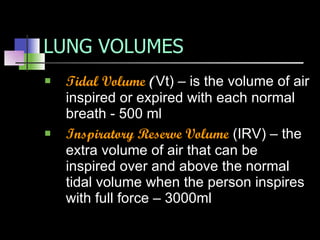
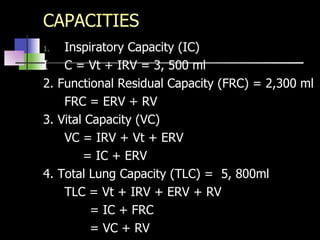
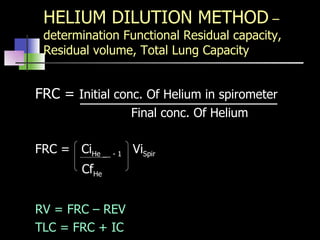
The document discusses the goals and major functional events of respiration, including pulmonary ventilation, diffusion of gases, transport of gases, and regulation of ventilation. It describes the respiratory system and muscles involved in inspiration and expiration. It also covers topics like compliance, surfactant, work of breathing, lung volumes, capacities, factors affecting lung function, and the functions of the respiratory passages.