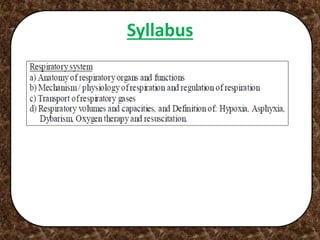
The document provides information on the respiratory system, including:
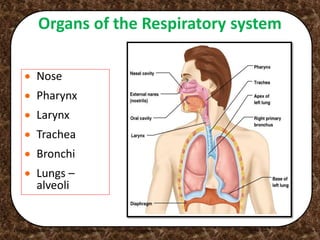
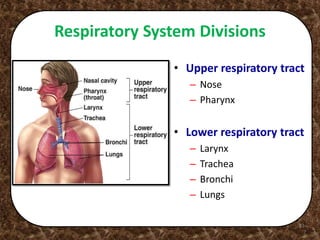
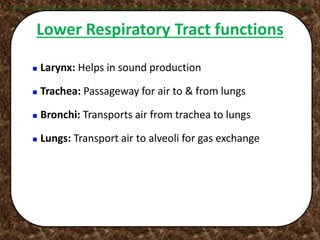
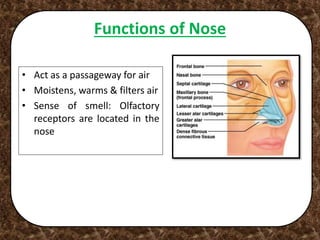
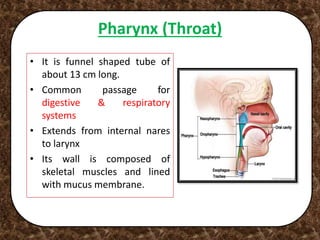
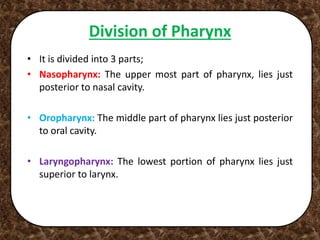
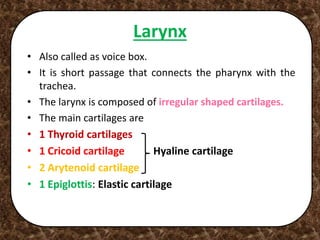
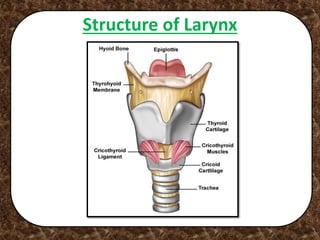
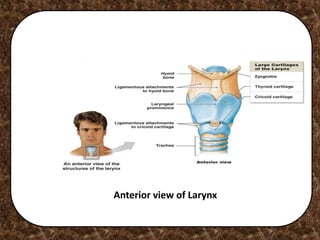
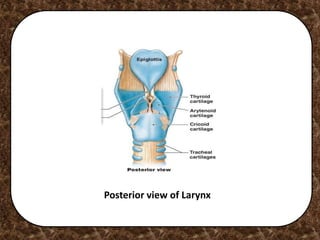
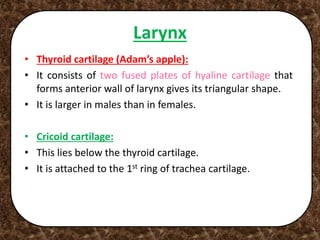
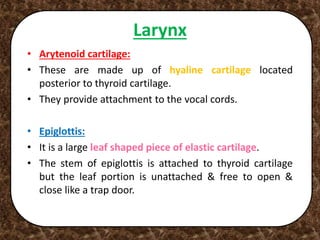
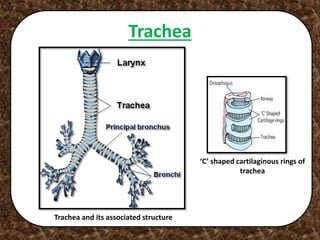
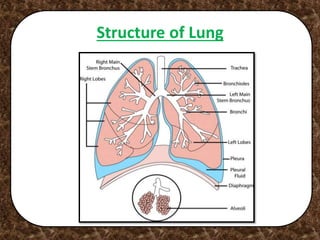
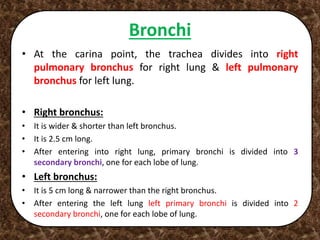
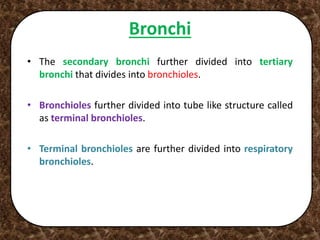
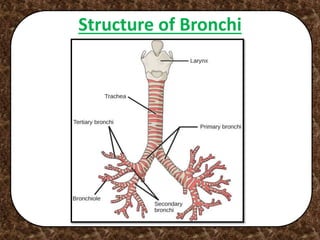
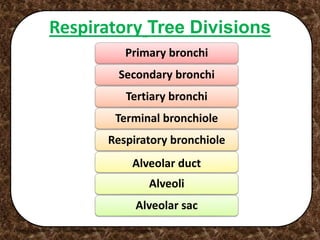
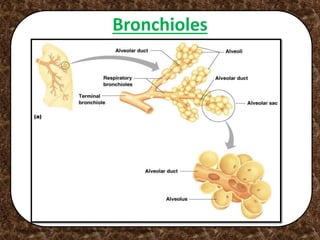
1. It describes the major organs of the respiratory system including the nose, pharynx, larynx, trachea, bronchi, and lungs.
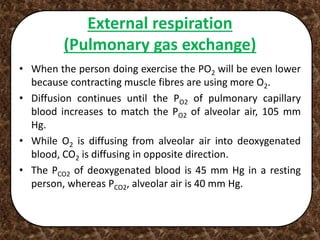
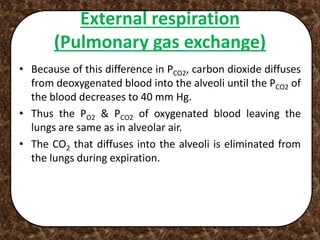
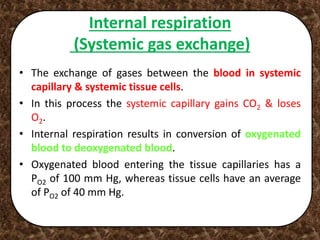
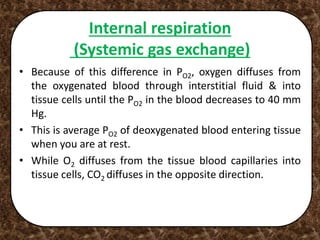
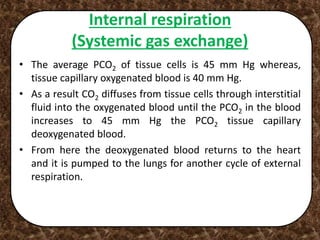
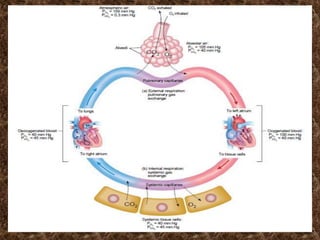
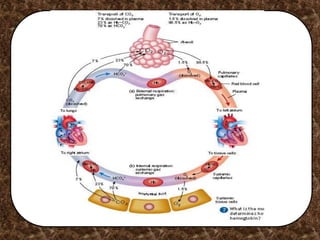
2. It explains the processes of external respiration which is the exchange of gases between the lungs and blood, and internal respiration which is the exchange of gases between the blood and cells.
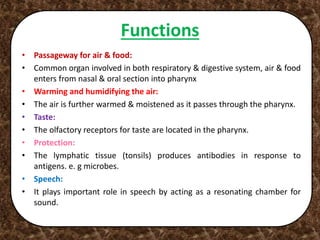
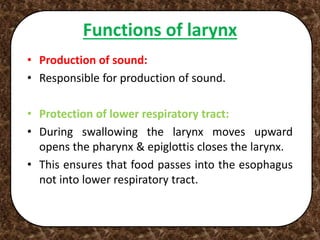
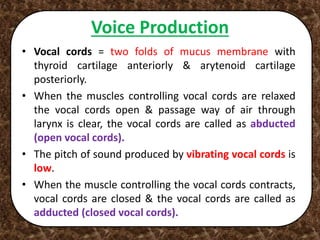
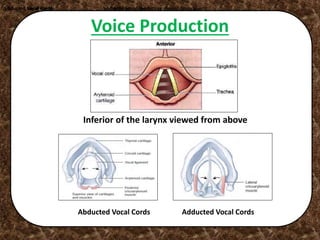
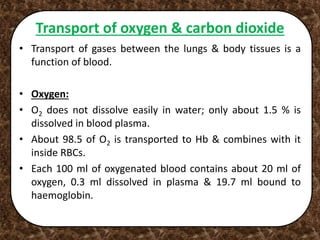
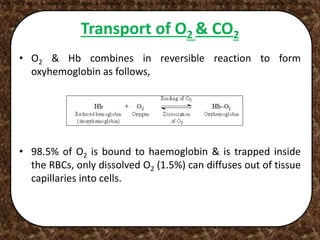
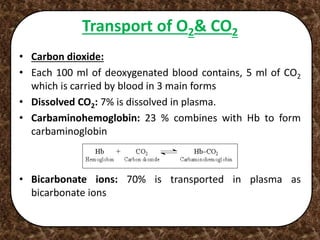
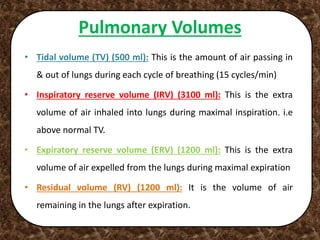
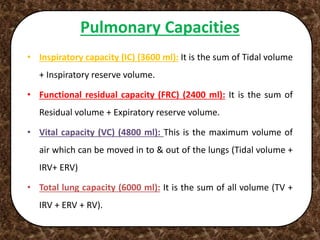
3. It provides details on pulmonary ventilation, the transport of oxygen and carbon dioxide in the blood and tissues, and the role of the respiratory system in regulating blood pH, sound production, thermoregulation and protection from pathogens.