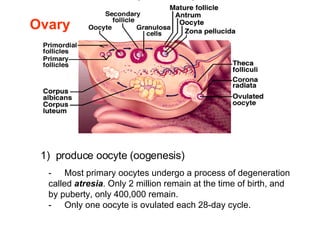
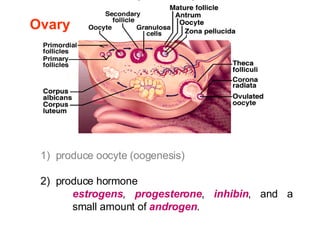
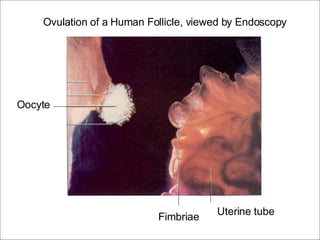
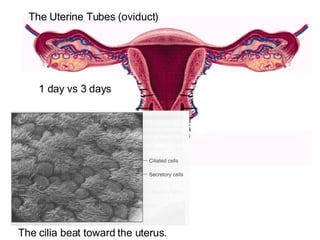
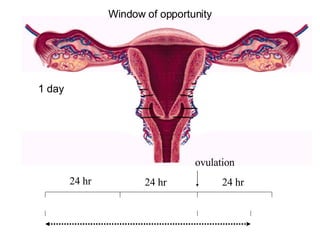
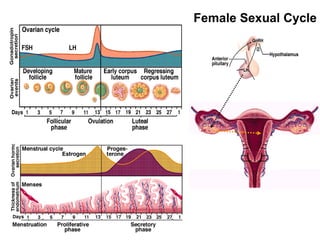
The female reproductive system undergoes a monthly cycle to prepare for potential pregnancy. If pregnancy does not occur, the thickened uterine lining sloughs off during menstruation. The cycle consists of three phases - the follicular phase where an egg is selected and matured, ovulation of the egg, and the luteal phase where the corpus luteum secretes hormones in preparation for potential implantation. This cycle is regulated by hormones from the hypothalamus, pituitary gland, ovaries and uterus.