The document provides an overview of the male and female reproductive systems including:
- Primary and secondary sex organs that produce and transport gametes in males (testes, ducts, glands) and females (ovaries, uterine tubes, uterus, vagina).
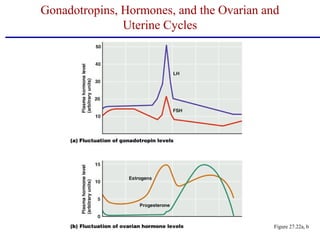
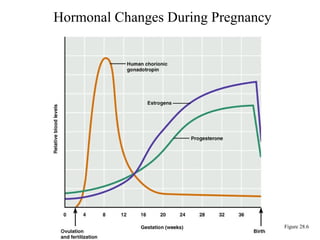
- The hormonal regulation of the testes and ovaries, including feedback loops between the hypothalamus, pituitary gland, and gonads.
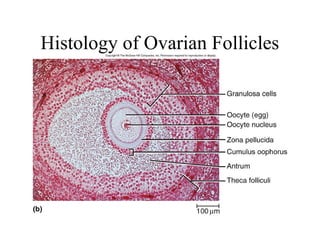
- Spermatogenesis and oogenesis, the processes by which gametes are produced in the testes and ovaries.
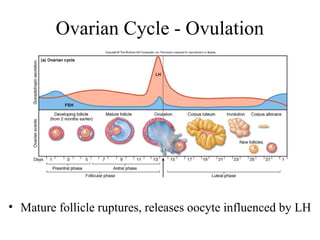
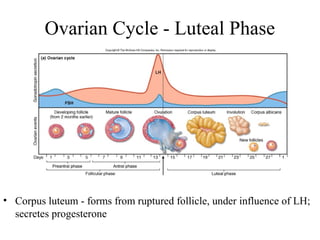
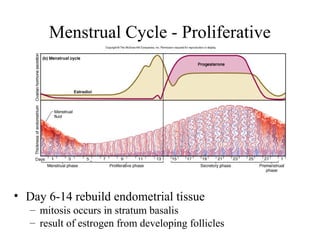
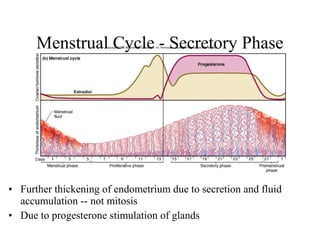
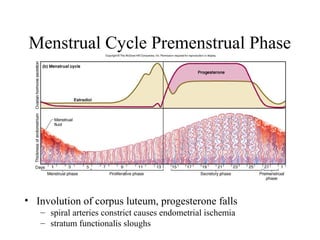
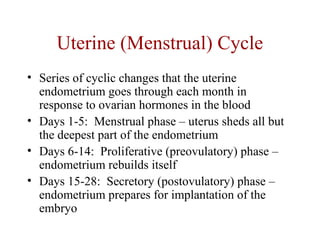
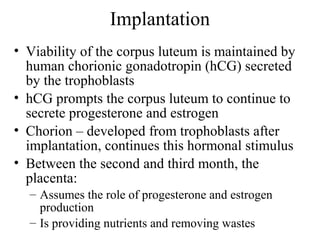
- The ovarian and uterine cycles regulated by hormones including estrogen and progesterone. Key events like ovulation and menstruation are described.
- Fertilization and early embryonic development up