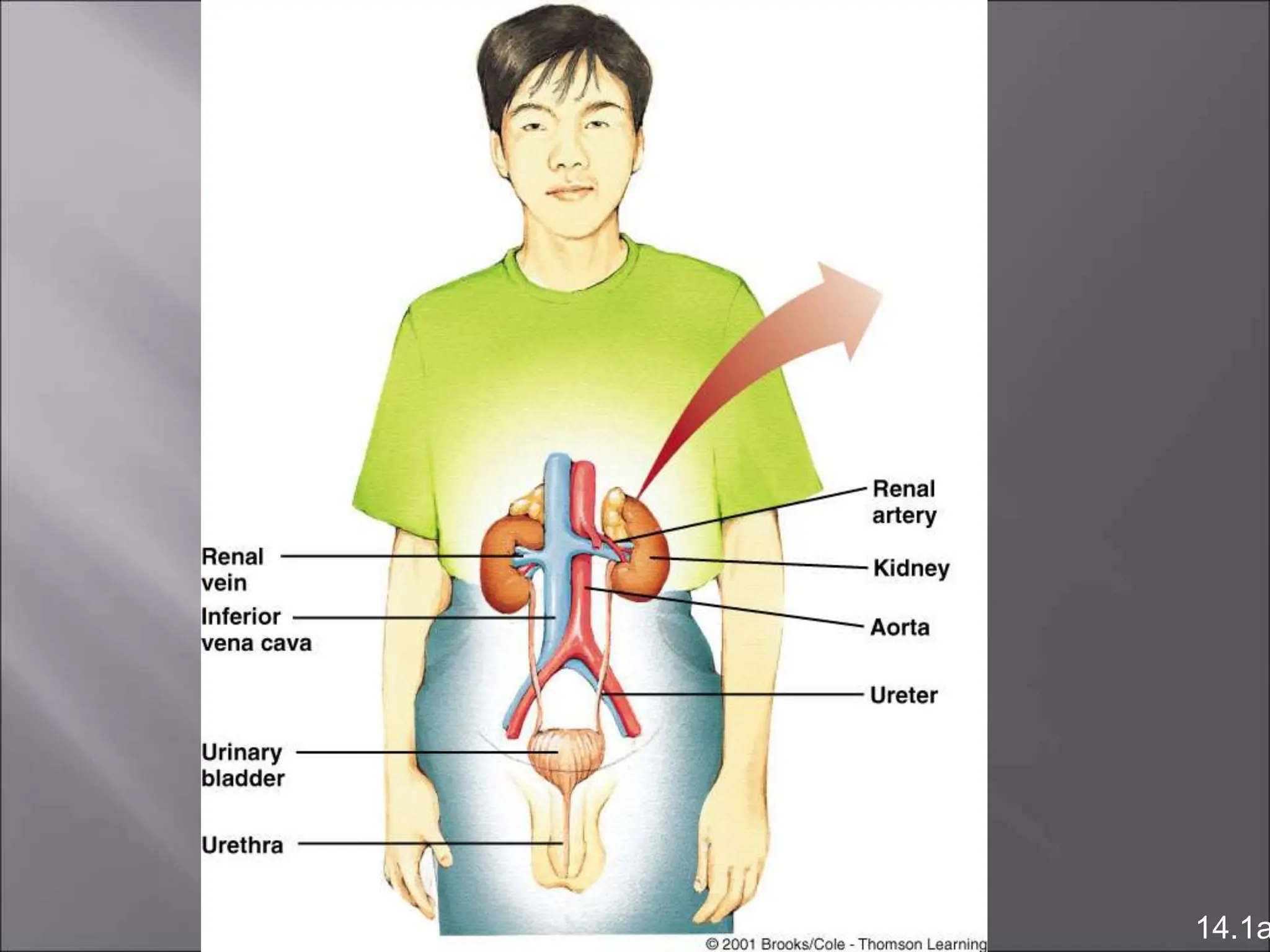
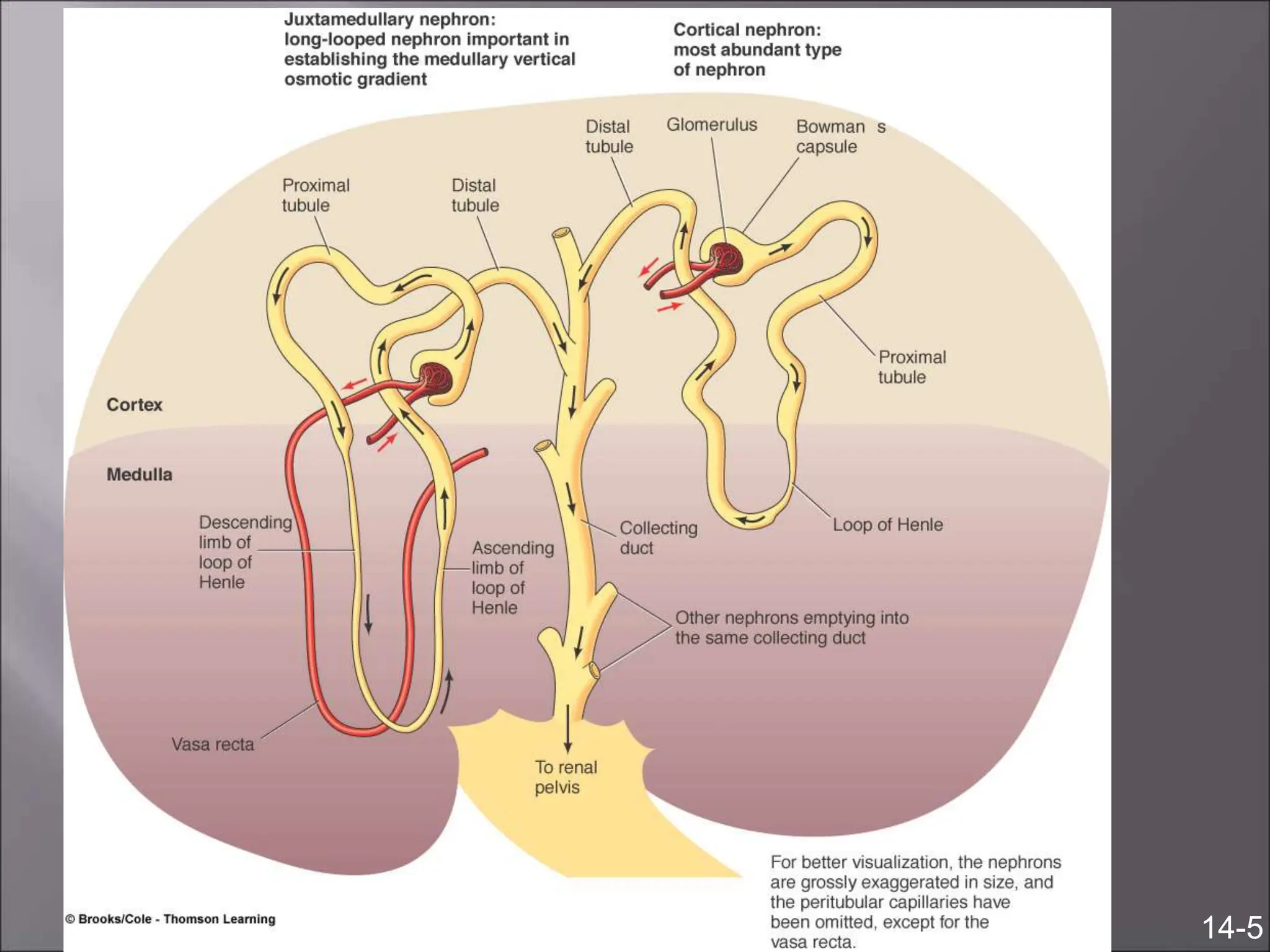
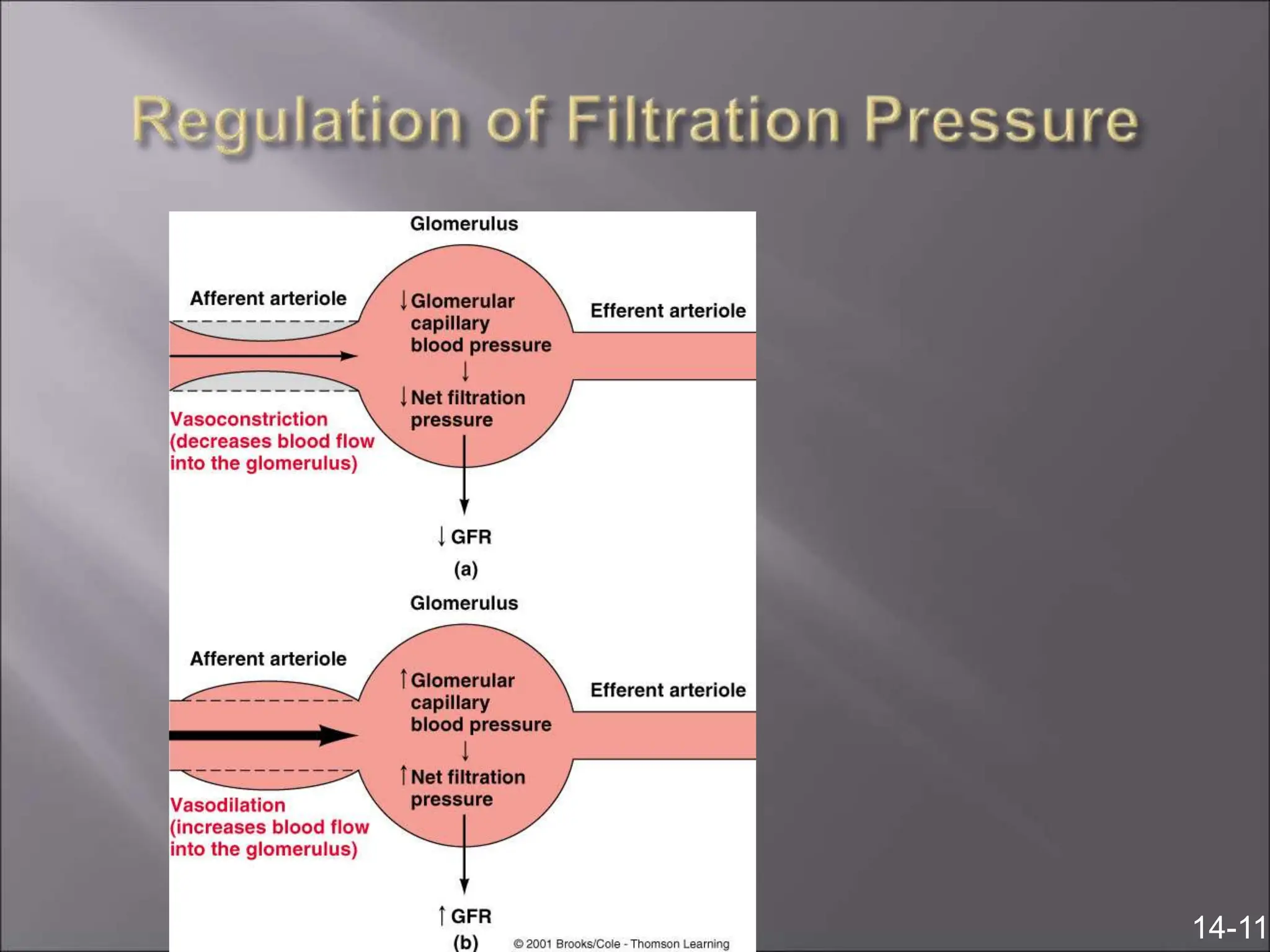
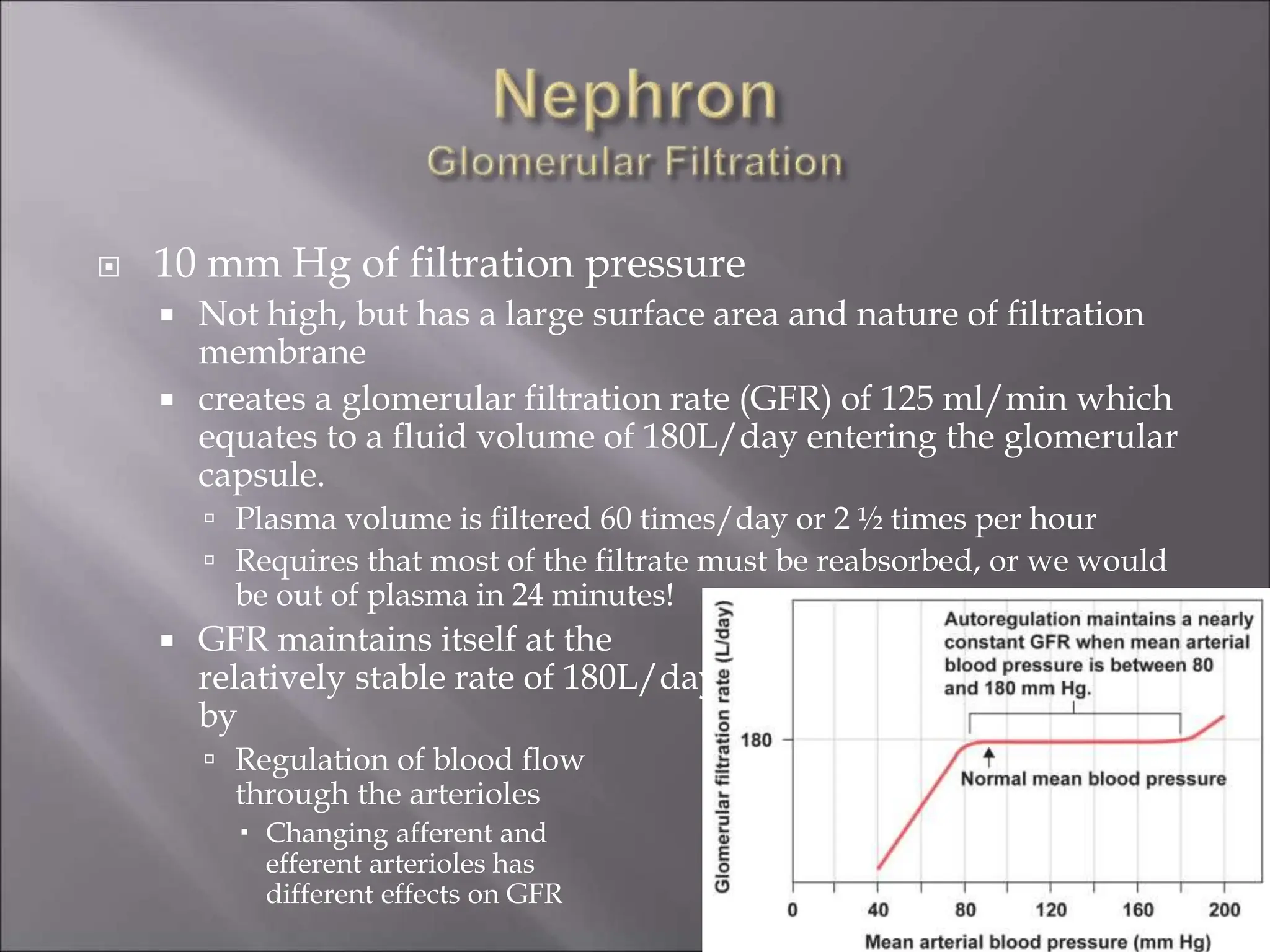
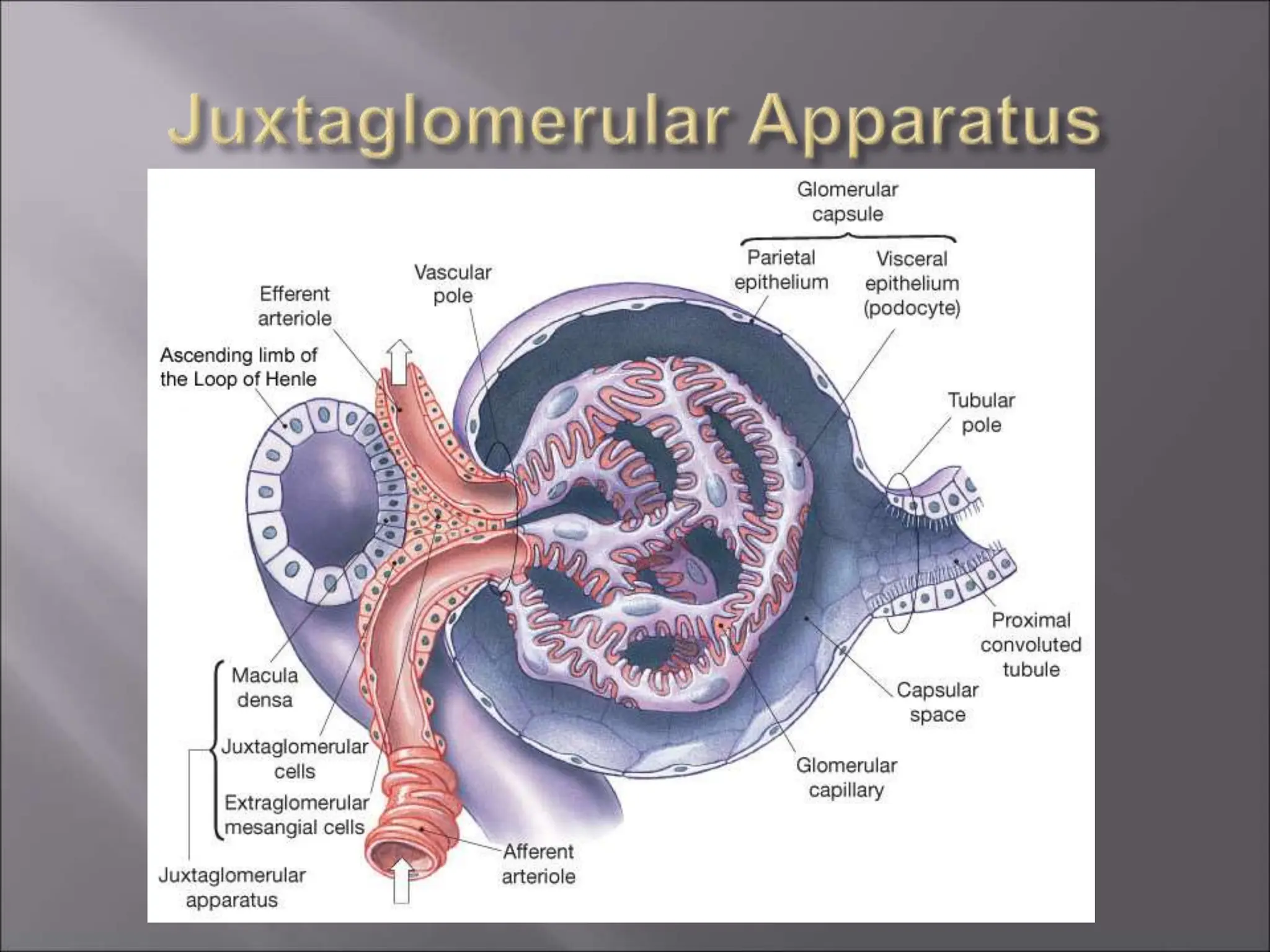
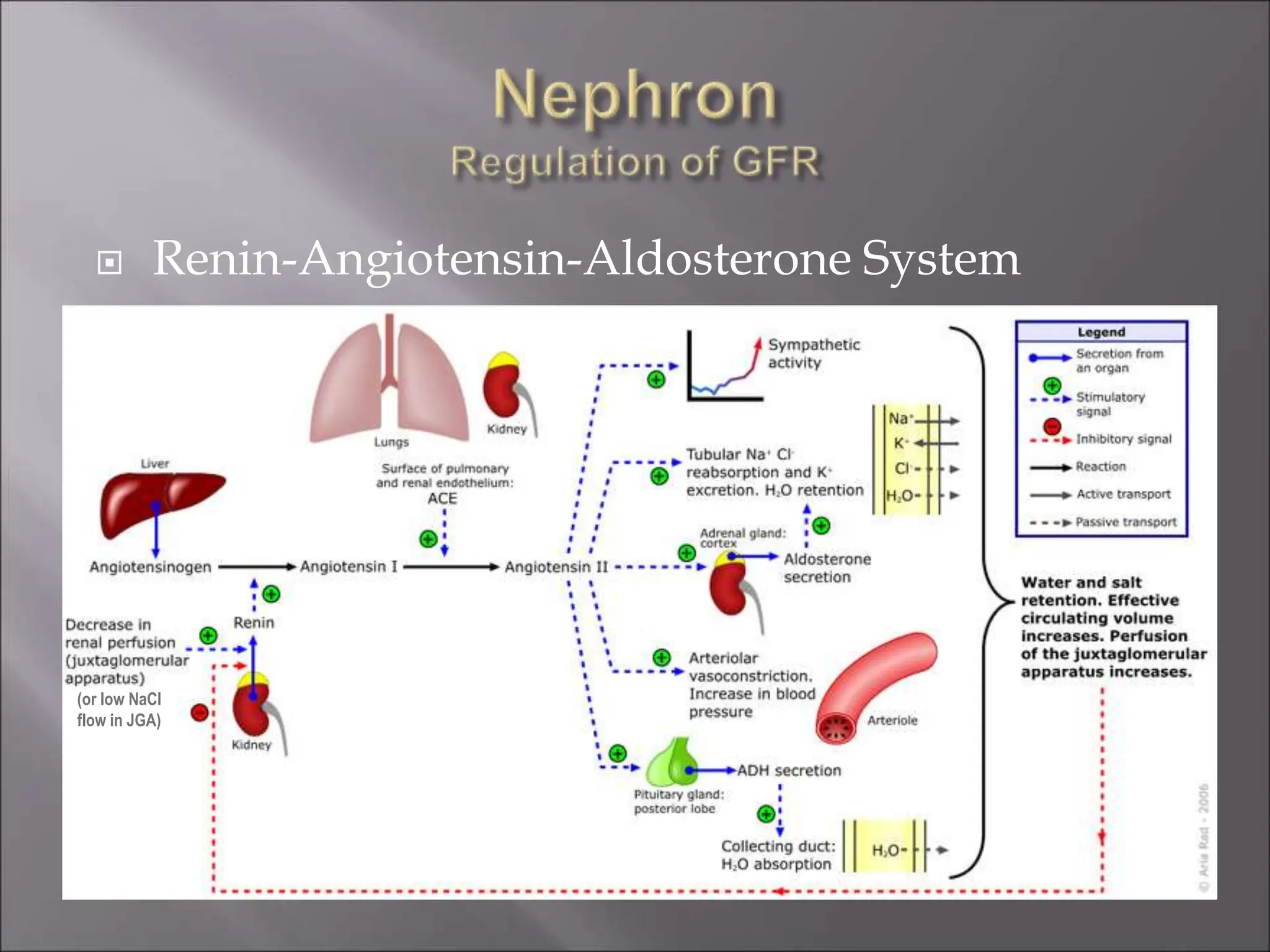
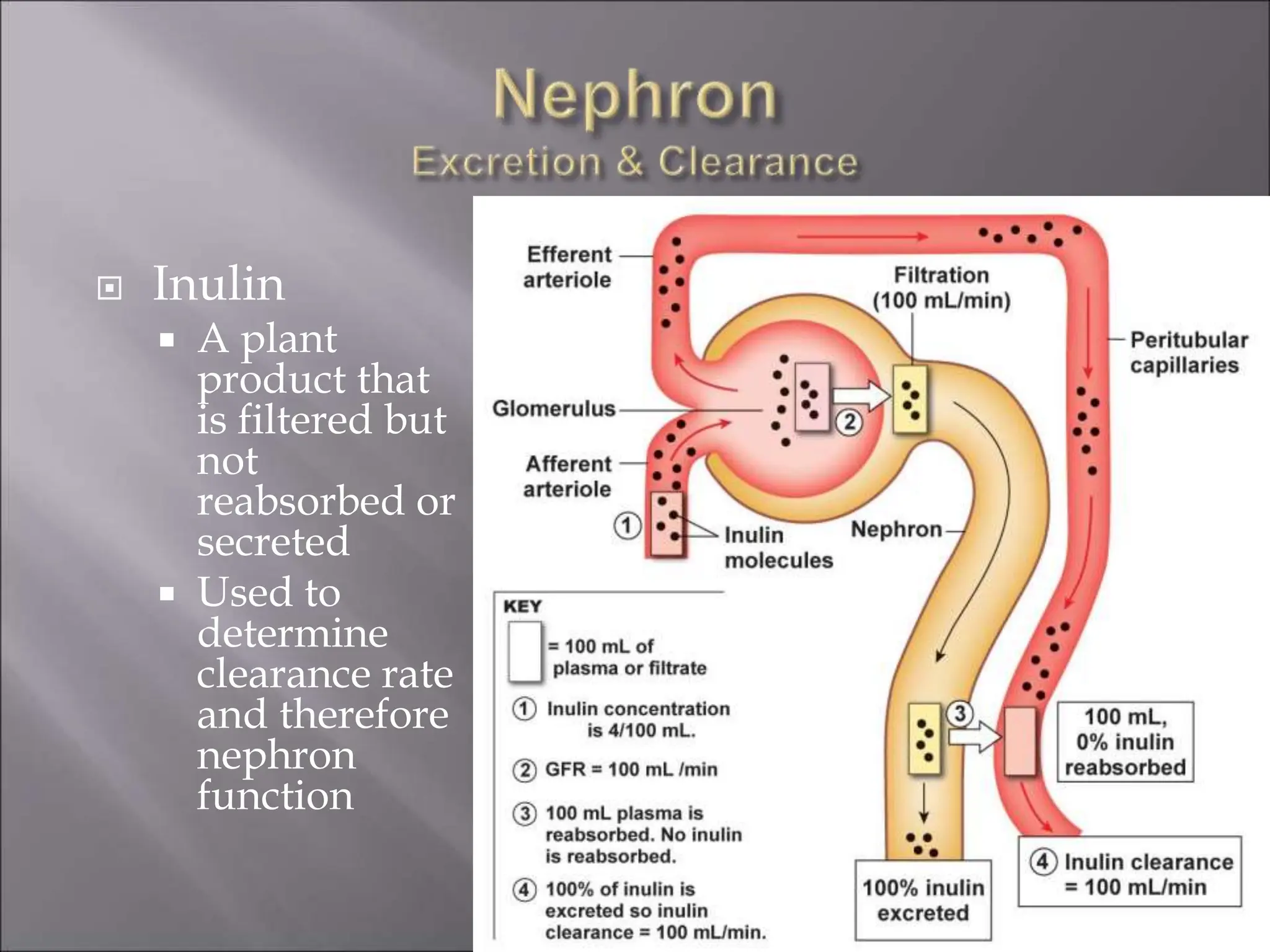
The nephron is the functional unit of the kidney that filters blood to produce urine. It consists of a glomerulus for blood filtration and a tubule for reabsorption and secretion. The kidneys regulate fluid volume and composition by precisely controlling glomerular filtration, tubular reabsorption and secretion. Hormones and the renin-angiotensin system help maintain stable glomerular filtration rate despite changes in blood pressure.