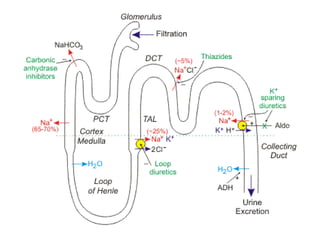
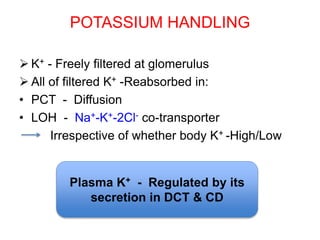
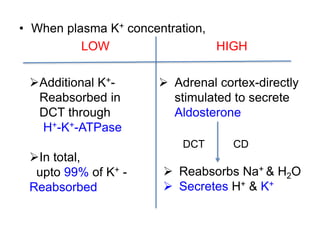
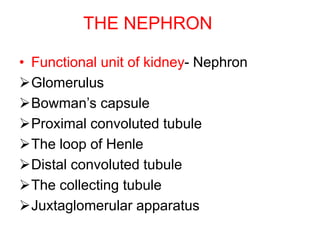
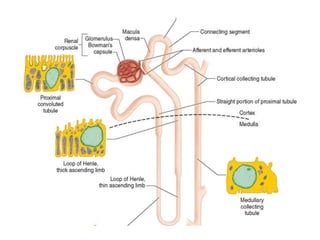
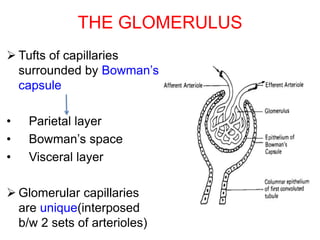
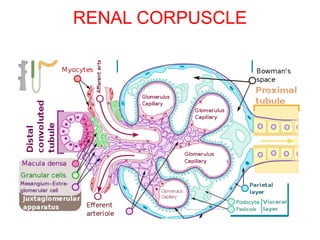
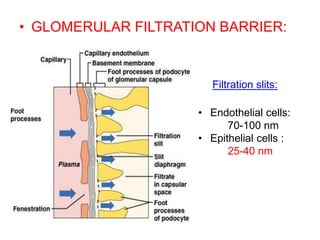
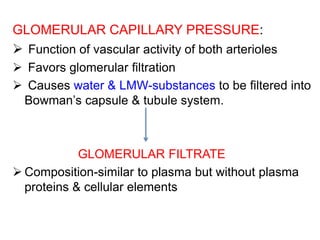
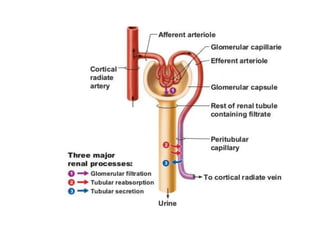
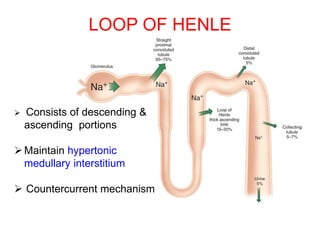
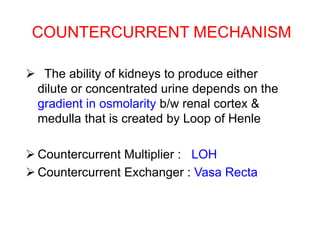
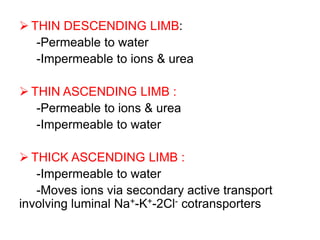
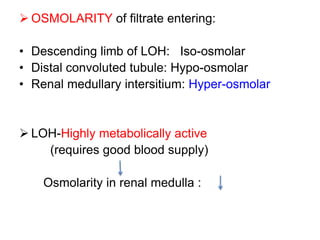
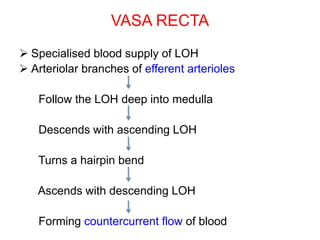
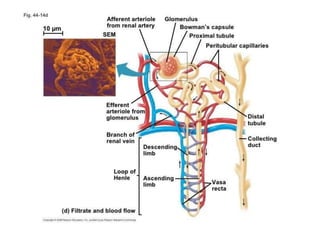
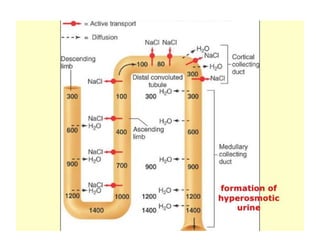
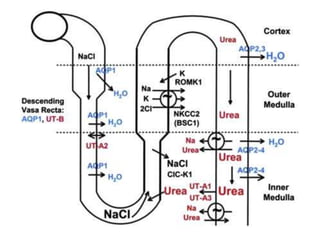
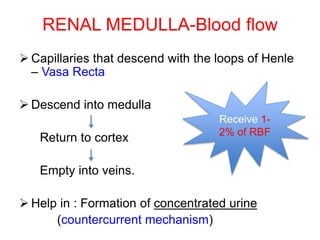
The kidneys are bean-shaped organs located in the retroperitoneal space that filter blood to produce urine. The functional unit of the kidney is the nephron, which contains a glomerulus for blood filtration and a tubule for reabsorption and secretion. Filtration occurs where glomerular capillaries are surrounded by Bowman's capsule in the renal corpuscle. Most reabsorption occurs in the proximal convoluted tubule under hormonal control. The loop of Henle and vasa recta create a medullary osmotic gradient for urine concentration. Urine is concentrated in the collecting duct by aquaporin water channels regulated by ADH.
![Measurement of RBF
Renal plasma flow (RPF) : most commonly
measured by p-aminohippurate clearance
PAH : Completely cleared from plasma
RPF =Clearance of PAH= * Urine flow
RBF=
[PAH]U
[PAH]P
RPF
1-Hematocrit
Normally, RPF 660 ml/min
RBF 1200 ml/min](https://image.slidesharecdn.com/renalphysiology-200318202015/85/Renal-physiology-48-320.jpg)

![ Creatinine clearance =
[Urine]Cr * Volume
[Plasma]Cr
Filtration fraction =
GFR
RPF
• Normally, FF = 20%
• Fraction of plasma that is
filtered by glomerulus](https://image.slidesharecdn.com/renalphysiology-200318202015/85/Renal-physiology-54-320.jpg)
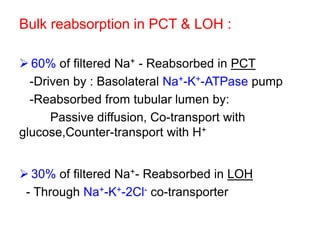
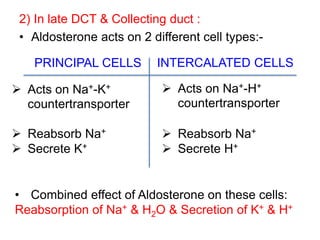
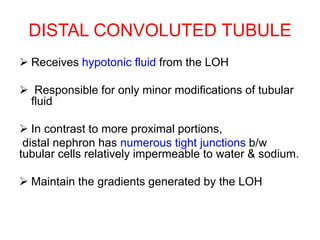
![Reabsorption in early DCT:
90% of filtered Na+ - already reabsorbed before
filtrate reaches DCT
Intracellular [Na+] –kept low as a result of
basolateral Na+-K+-ATPase
• Na+ transfer across tubular cell luminal
membrane-controlled by ALDOSTERONE
1) In DCT :
5% of filtered Na+ -Reabsorbed through Na+-Cl-
co-transporter in luminal membrane](https://image.slidesharecdn.com/renalphysiology-200318202015/85/Renal-physiology-60-320.jpg)