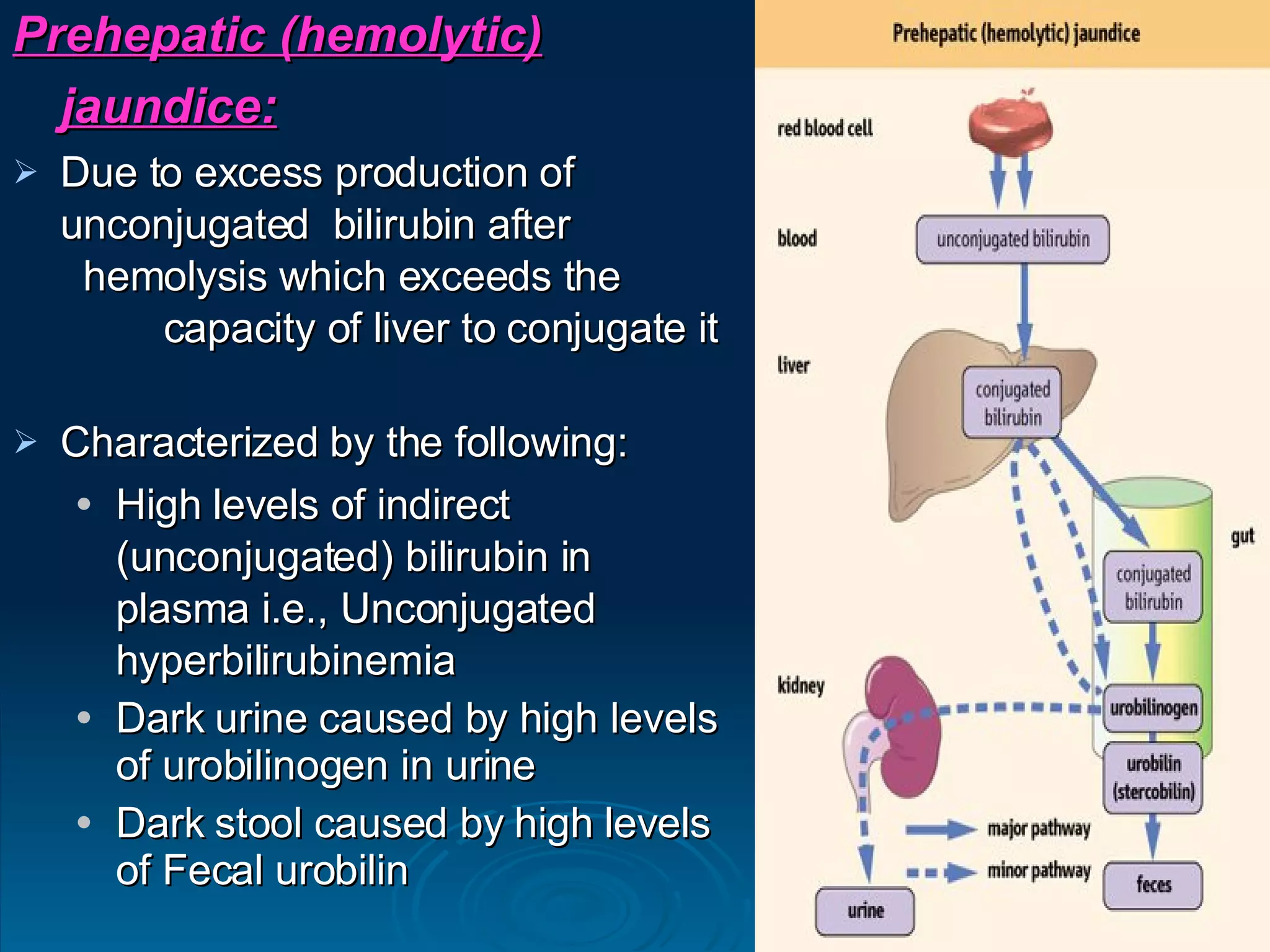
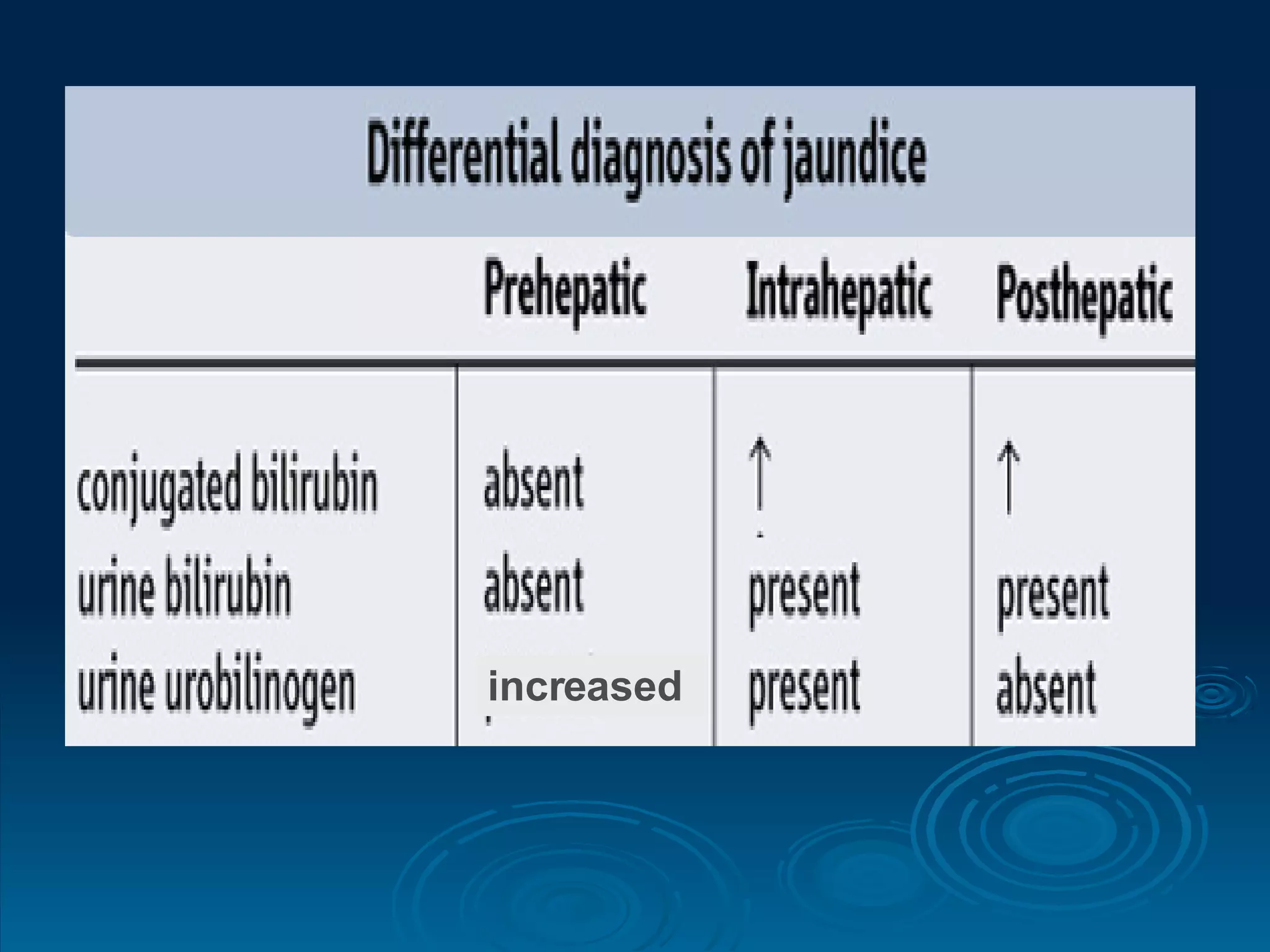
The document summarizes heme catabolism and bilirubin metabolism. It discusses the three stages of heme degradation: formation of bilirubin in the reticuloendothelial system, uptake and conjugation of bilirubin in the liver, and catabolism of bilirubin in the gut. It also describes different types of hyperbilirubinemia and jaundice, including physiological, genetic causes like Gilbert's syndrome, and obstructive jaundice.