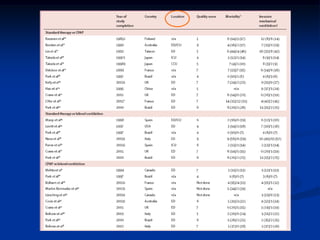
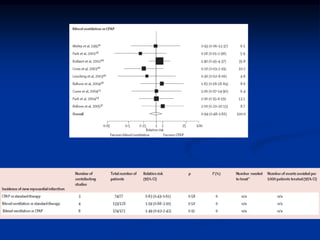
This document provides an outline and overview of non-invasive positive pressure ventilation (NPPV). It begins with a brief history of ventilation techniques and then discusses the rationale for using NPPV to avoid complications of endotracheal intubation. The document reviews several important clinical studies on the use of NPPV in conditions such as COPD exacerbation, acute cardiogenic pulmonary edema, hypoxic respiratory failure, post-operative settings, and extubation failure. It finds that NPPV can reduce intubation rates, complications, and mortality in some of these situations compared to standard care. The document concludes by discussing factors that determine the success of NPPV.